GLP‑1s at scale: decoding Swiss Re’s mortality forecast
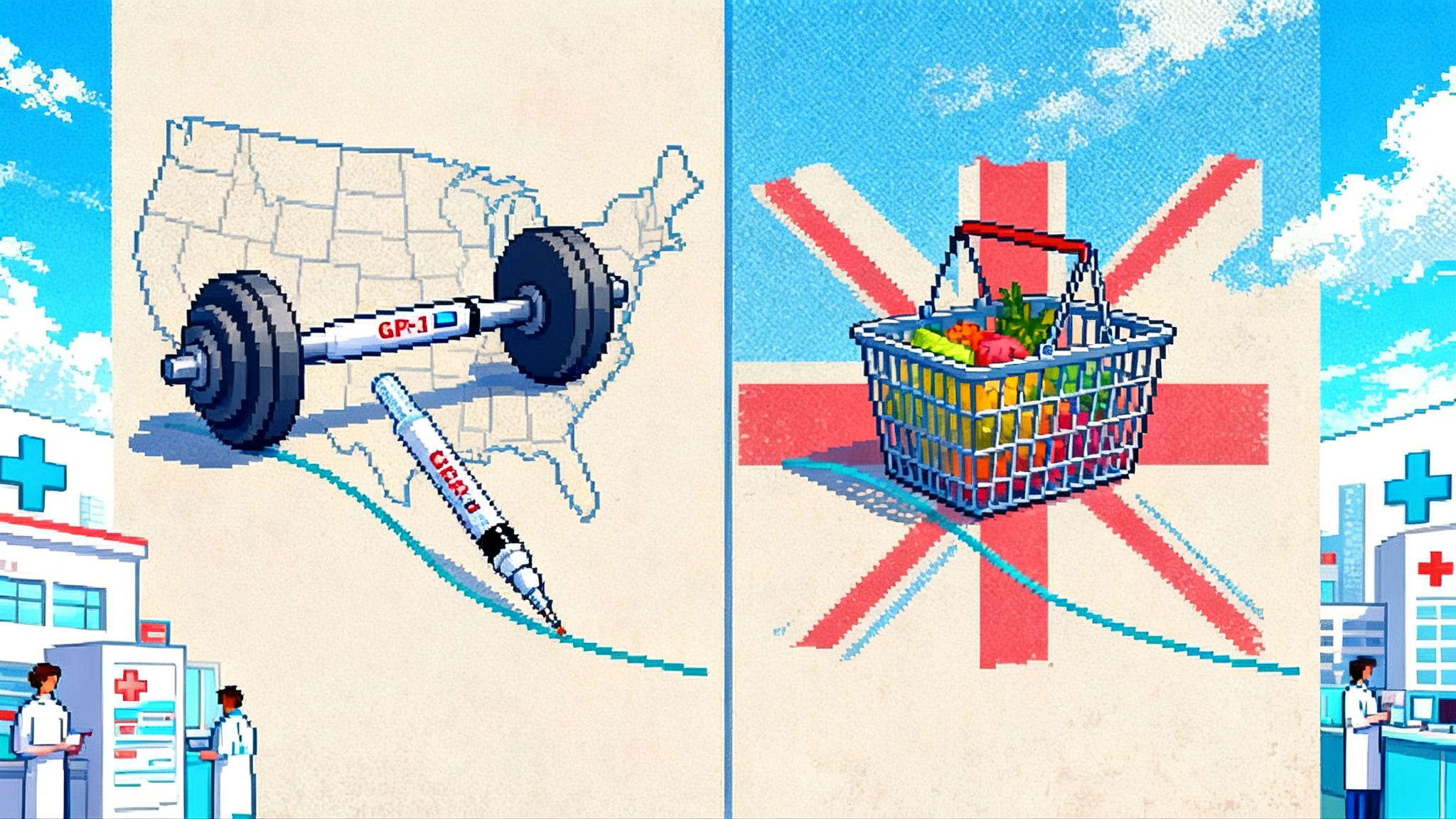
Swiss Re projects that broad GLP‑1 adoption could trim U.S. deaths by 6.4% and the U.K. by 5.1% by 2045. We stress‑test that forecast, parse the latest outcomes data, and map the ripple effects for insurers, pensions, and public health.
The headline: a mortality nudge with system‑level stakes
On September 17, Swiss Re published an arresting projection: if GLP‑1 medicines see sustained, broad uptake, cumulative all‑cause mortality could fall by up to 6.4% in the United States and 5.1% in the United Kingdom by 2045. In baseline scenarios, they estimate smaller but still meaningful declines. The modeled range hinges on adoption, adherence, and whether people pair medication with durable habit change. The signal is strong enough that it could reshape life insurance assumptions, pension liabilities, and public health planning. You can read the topline assumptions in Swiss Re’s new modeling.
This piece pressure tests that view. What would need to go right for society to realize a mortality dividend of that size? Where could it stall? And how do we capture the upside without worsening the very inequities that drive cardiometabolic risk in the first place?
What Swiss Re modeled, in plain terms
Swiss Re built three trajectories for the U.S. and U.K. general populations through 2045.
- Optimistic: high engagement, tolerable side effects, long‑term use is feasible, weight loss maintained, and real lifestyle change. That yields a 6.4% U.S. and 5.1% U.K. reduction in cumulative all‑cause mortality.
- Baseline: uptake mainly in people with obesity and higher‑risk overweight; side effects manageable for many; some yo‑yo weight patterns; partial lifestyle change. Roughly 4.0% U.S. and 3.2% U.K. reductions.
- Pessimistic: limited use beyond the sickest; discontinuation is common; weight regain typical; minimal lifestyle change. About 2.3% U.S. and 1.8% U.K. reductions.
In other words, the same drug class can produce very different futures depending on human behavior, clinical practice, pricing, and supply. The spread between those scenarios is the real story.
Stress testing the assumptions
1) Uptake
Uptake is not just desire, it is eligibility, prescription access, and payor coverage. Today’s demand is high, but the eligible population is far larger than current supply and coverage. Employers and insurers are progressively extending coverage for people with obesity and additional risk factors, while tightening criteria for lower‑risk patients. Broader adoption will depend on continued evidence of hard outcomes, clinician comfort with long‑term prescribing, and the availability of lower‑cost or oral options that reduce friction.
Where uptake could underperform:
- Narrow coverage policies, prior authorizations, and step‑therapy requirements that slow starts
- Primary care capacity, since longitudinal titration and monitoring are work‑intensive
- Hesitancy among patients who have tried and stopped due to side effects or cost surprises
Where it could outperform:
- Outcomes‑based contracts that bring payors off the sidelines
- Fixed‑dose combinations and oral agents that are easier to live with
- Employer programs that pair medication with coaching and gym benefits
2) Adherence and persistence
Adherence is the fulcrum. GLP‑1s work while you take them. Many people stop within a year due to gastrointestinal side effects, cost, supply interruptions, or the simple burden of injections and refills. After discontinuation, weight regain is common, sometimes rapid, and some of it is lean mass if people are not protecting muscle. That on‑off pattern erodes the mortality benefit Swiss Re is modeling.
Realistic mitigants:
- Slow titration with proactive side‑effect management, including temporary dose holds
- Bundled coaching that standardizes expectations, prepares for plateaus, and treats the drug as a tool rather than a cure
- Periods of maintenance dosing rather than full cessation, especially in higher‑risk patients
3) Lifetime use vs strategic de‑escalation
Will people need these drugs for life? Likely not everyone. Think in cohorts.
- High‑risk cardiometabolic patients may justify long‑term therapy, particularly if they have established cardiovascular disease, sleep apnea, fatty liver disease, or severe obesity. The risk reduction for them is largest.
- Moderate‑risk patients might benefit from an induction phase to reach a new weight set point, then a maintenance plan that blends lower‑dose pharmacotherapy with structured resistance training and nutrition.
- Low‑risk patients with aesthetic goals are where the risk‑benefit calculus is weakest. Without durable lifestyle change, discontinuation often leads to rebound weight.
Swiss Re’s optimistic curve implicitly assumes many patients land in the first two lanes and avoid the third.
4) Cost and coverage
List prices remain high, and coinsurance can be painful. Even if drug makers strike value‑based contracts, the near‑term budget impact can exceed the speed of savings from fewer cardiovascular events or diabetes complications. Public payors face statutory constraints on obesity drug coverage. Payers are experimenting with eligibility tiers, stop rules, and adherence gates to align spend with benefit. If cost trends lower with competition and scale, the modeled mortality gains become more plausible for the general population, not just the insured and affluent.
5) Supply and convenience
Supply constraints have eased in some markets but remain patchy. Manufacturing scale‑up, pen component availability, and global demand create fragility. Injectables also carry behavioral friction that oral GLP‑1s could fix, but only if efficacy holds and side effects stay manageable. The more convenient the therapy, the more realistic the sustained adherence that Swiss Re assumes in its upper‑bound scenario.
What the evidence says about hard outcomes
Swiss Re’s model only matters if the drugs reduce events that kill people. We now have randomized evidence that they do, at least in specific high‑risk groups.
-
In the SELECT trial, 17,604 adults with overweight or obesity and established cardiovascular disease but without diabetes were randomized to semaglutide 2.4 mg or placebo for a median of 3.3 years. Semaglutide reduced major cardiovascular events and reduced all‑cause mortality with a hazard ratio around 0.81. Importantly, non‑cardiovascular deaths also fell. See the full breakdown in the SELECT trial mortality analysis.
-
In people with type 2 diabetes, earlier cardiovascular outcomes trials across the GLP‑1 class showed consistent reductions in major adverse cardiovascular events. Newer dual agonists have at least preserved, and may improve upon, that cardioprotection while driving larger weight and glycemic changes. Those data reinforce a path to fewer fatal events in the highest‑risk groups.
Dementia and neuro outcomes
Observational analyses drawing on millions of records suggest that GLP‑1 therapy is associated with lower incident dementia and neurocognitive disorders in people with diabetes. The association signals are encouraging and biologically plausible through effects on inflammation, insulin signaling, vascular risk, and possibly amyloid processing. But they are not randomized data. Dedicated Alzheimer’s trials of semaglutide are underway with results expected late 2025. Until then, any claim of direct neuroprotection remains provisional.
Safety and the muscle question
Gastrointestinal side effects are common and usually manageable. Rare events like pancreatitis and gallbladder disease remain under surveillance. The underappreciated risk is losing lean mass along with fat. If people drop weight quickly without resistance training and adequate protein, they can creep toward sarcopenia, which raises fall risk, worsens insulin sensitivity, and undermines long‑term health. A mortality model that ignores muscle quality is overly optimistic.
Second‑order effects: insurers, pensions, public health
Life and health insurers
- Pricing and reserves: If mortality improves faster than expected in higher‑risk cohorts, term life claims could ease over time, but not before medical claims rise due to drug spend. Insurers will update mortality improvement assumptions, lapse behavior, and underwriting manuals.
- Benefit design: Expect more plans to cover GLP‑1s for patients with obesity plus risk factors while bundling them with structured programs. Outcomes‑based contracting can align premiums with realized risk reduction, not theoretical benefit.
- Risk selection: If coverage concentrates among employees of large firms and higher income households, individual markets may see selection effects unless subsidies or public benefits expand.
Pensions and retirement plans
- Longevity risk: Even a few percentage points of mortality improvement compound into larger liabilities for defined benefit plans and annuity writers. Swiss Re’s optimistic scenario implies meaningful shifts in duration and cash flow timing.
- Asset allocation and hedging: Plans should revisit longevity hedges and consider instruments that benefit from mortality improvement. Annuity pricing will likely adjust if healthier cohorts live longer.
- Labor supply: Improved cardiometabolic health could extend working lives and reduce disability claims. That softens some liability pressure but with a long lag.
Public health and workforce
- Morbidity mix: Fewer heart attacks and strokes mean less inpatient burden, but more long‑term medication management. Health systems should shift capacity toward prevention, titration clinics, and strength programs.
- Equity: Without careful policy, GLP‑1 access will mirror existing inequities in obesity, food environments, and clinical care. The upside for mortality at a population level depends on reaching those at highest risk, not only those with the best benefits.
- Productivity: Better weight, lipids, and glycemic control improve energy and reduce sick days. Employers that embed these programs well can capture productivity gains that justify coverage.
A pragmatic roadmap for the longevity dividend
The mortality dividend is not automatic. It requires engineering a drug‑plus‑behavior system that keeps muscle, sustains metabolic wins, and broadens access. Here is a blueprint for payors, providers, employers, and policymakers.
1) Make muscle the co‑therapy
- Program every GLP‑1 start with a simple resistance plan: two to three sessions per week that hit the big four movements, squat, hinge, push, pull. Prioritize progressive overload with safe form.
- Set a protein target matched to body weight and goals with even distribution across meals. Emphasize whole foods first, supplement only if necessary.
- Track functional markers, not just weight. Use grip strength, sit‑to‑stand, or periodic DEXA when available. The aim is fat loss with lean mass preservation.
2) Engineer adherence without overmedicating
- Use slow, patient‑friendly titration. Normalize pauses at a dose when side effects flare, then resume when tolerable.
- Pair medication with coaching that covers sleep, fiber, hydration, and micronutrient sufficiency. Patients who feel better stay on therapy.
- Plan for maintenance. For some, that means lower dosing once goals are met. For others with high vascular risk, long‑term therapy may be appropriate. Avoid abrupt stop‑start cycles that drive rebound.
3) Align coverage with outcomes
- Cover GLP‑1s for people with obesity plus a cardiometabolic condition or high predicted risk, and require participation in a strength and nutrition program. That reduces moral hazard while protecting muscle.
- Negotiate outcomes‑based contracts with clear endpoints, such as A1C reduction, blood pressure, CRP, or a composite risk score. Share savings when hospitalizations drop.
- Offer care bundles, medication plus coaching plus gym or home equipment stipend. Make the healthy path the easy path.
4) Expand access without widening gaps
- Subsidize coverage for lower income populations where obesity and cardiovascular risk are concentrated. Leverage community health centers and retail clinics for titration and follow up.
- Build community strength. Fund school and neighborhood strength spaces, safe walking routes, and food security programs. GLP‑1s cannot fix a broken food environment alone.
- Monitor equity metrics, initiation and persistence by income, race, and geography. Course correct when programs drift upscale.
5) Manage known risks up front
- Sarcopenia: Screen for frailty risk at baseline. Emphasize resistance training, adequate protein, vitamin D when deficient, and consider creatine for appropriate adults.
- Rebound weight: Before starting, agree on a maintenance plan. Use behavioral supports during dose reductions. If stopping, taper with a strength and nutrition emphasis rather than a hard stop.
- Mental health and eating disorders: Screen for active eating disorders and provide alternative care paths. Avoid prescribing where the risk outweighs the benefit.
- Pregnancy: Reinforce contraception counseling and hold therapy before conception and during pregnancy.
6) For insurers and pension funds, move now
- Build GLP‑1 scenarios into capital planning, optimistic, baseline, pessimistic. Update mortality improvement tables and lapse assumptions.
- Pilot outcomes‑based reimbursement and center‑of‑excellence networks that combine medication with strength and nutrition.
- Invest in registries and real‑world evidence pipelines to track hard outcomes. Link pharmacy, claims, and wearable data in privacy‑preserving ways.
- Consider longevity hedges and annuity repricing tied to achieved mortality improvement, not headline hype.
7) For policymakers, set the guardrails
- Clarify public coverage for high‑risk groups contingent on participation in evidence‑based lifestyle programs.
- Support training for primary care teams in resistance programming, nutrition counseling, and side‑effect management.
- Incentivize domestic manufacturing and supply chain resilience so access is not throttled by shortages.
Bottom line
Swiss Re’s model is a useful provocation. The optimistic curve is achievable only if we treat GLP‑1s as the front end of a system that preserves muscle, supports habits, and reaches the people who bear the brunt of cardiometabolic disease. The randomized data already show fewer heart attacks and fewer deaths in high‑risk patients, and large real‑world datasets are pointing in the same direction for other outcomes. But drugs alone will not deliver a population‑scale longevity dividend.
The playbook is clear. Pair medication with resistance training and nutrition. Design benefits that reward persistence and protect muscle. Expand access where risk is highest. Monitor for rebound and inequity. If we execute on that bundle, the mortality improvements Swiss Re modeled stop being a thought experiment and start becoming an actuarial reality.