Retro’s autophagy pill enters humans as AI rewrites aging
Retro Biosciences is set to begin first human testing in Australia of RTR242, an autophagy-activating pill aimed at Alzheimer’s. Paired with OpenAI’s GPT‑4b micro reprogramming work, it is a pivotal test for geroscience in the clinic.
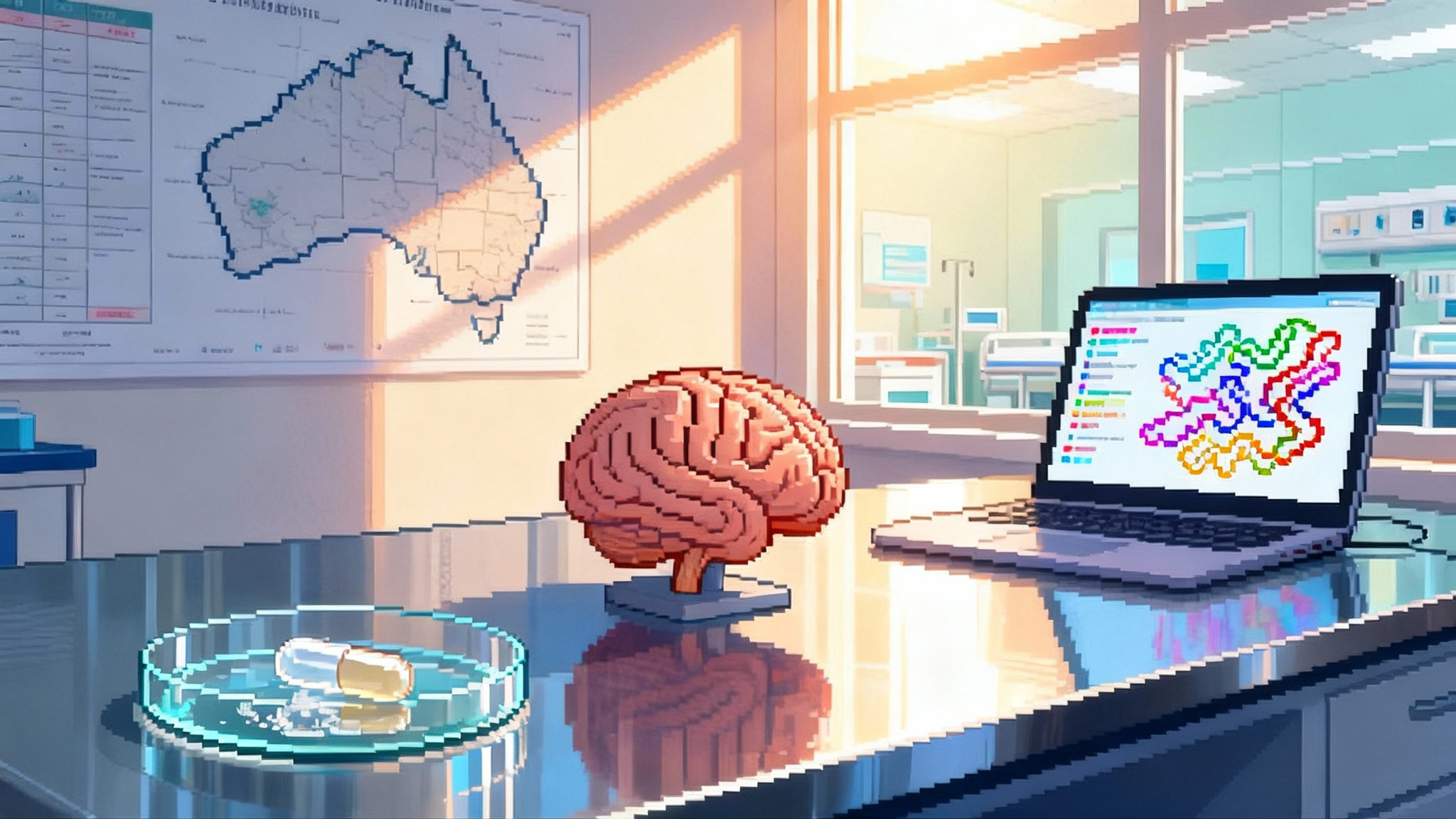
A small molecule, a big bet
Retro Biosciences has circled late 2025 for first human dosing in Australia of RTR242, a small molecule designed to activate autophagy and clear intracellular junk that accumulates with age. The company says the Alzheimer’s program will anchor its push from preclinical promise to clinical reality, with site selection and vendors already lined up. The plan surfaced in mid September 2025, with reporting that Retro plans first human dosing in Australia. If it proceeds on schedule, RTR242 will be one of the first autophagy-centric drugs for brain aging to hit the clinic.
That timing dovetails with a second story line. In August, OpenAI and Retro disclosed results from a joint research effort using a domain model called GPT‑4b micro to reengineer the SOX2 and KLF4 transcription factors, core components of cellular reprogramming. The teams reported large, fast gains in markers of induced pluripotency and signs of improved DNA damage repair in vitro. We will come back to why that matters.
Why autophagy could move the needle in Alzheimer’s
For twenty years, the Alzheimer’s playbook has mostly meant removing amyloid plaques and, increasingly, reducing phosphorylated tau. Those are important disease hallmarks. Yet the brain’s housekeeping machinery is upstream of many pathologies. Autophagy is the cell’s recycling line. It tags damaged proteins and organelles, wraps them in autophagosomes, and feeds that cargo to lysosomes for breakdown and reuse. With age, that line jams. The result is a backlog of misfolded proteins, defective mitochondria, and inflammatory debris. Neurons are especially vulnerable because they are long lived and metabolically demanding.
Turning that conveyor belt back on could influence multiple drivers of brain aging at once. In neurons and glia, enhanced autophagy may:
- Improve proteostasis by shuttling tau fragments, TDP‑43, and alpha‑synuclein toward degradation, which might reduce toxic oligomers before they aggregate into larger lesions.
- Restore organelle quality control, especially mitophagy, which can reduce reactive oxygen species and normalize bioenergetic supply to synapses.
- Quiet neuroinflammation indirectly, since dysfunctional proteostasis and leaky mitochondria feed microglial activation and astrocyte stress responses.
- Support synaptic maintenance by keeping local protein turnover and vesicle cycling in balance, which is essential for plasticity and memory formation.
Compared with plaque clearance alone, autophagy activation is a systems intervention. It does not depend on finding and binding a single extracellular target. It acts inside cells across multiple pathways that co‑evolve in disease. That breadth is a double edged sword. On the upside, it may produce additive benefits across mechanisms that rarely travel alone in an aging brain. On the downside, a broad tug on stress‑response circuits can create off‑target effects in peripheral tissues. The trial will begin to tell us which edge is sharper in humans.
The geroscience pivot: aging via disease endpoints
Regulators do not yet approve drugs for “aging” as a primary indication. Geroscience has adapted by targeting age‑related diseases with mechanisms that modulate aging biology. Think metabolic drugs that affect mTOR or AMPK moving through diabetes or kidney endpoints, or senolytics entering through fibrotic diseases. Alzheimer’s is an especially visible proving ground. It has clear clinical endpoints, an expanding toolbox of biomarkers, and urgent unmet need.
An autophagy activator that slows or reverses cognitive decline would mark a shift. It would say that tilting a core aging pathway can produce clinically relevant effects in a specific neurodegenerative disease. That would not make aging itself an approved label. It would do something more practical. It would validate the regulatory path for other aging‑mechanism drugs to advance through disease endpoints where the biology is most coupled to function.
Why start in Australia, and what that buys
Australia has become a popular venue for first‑in‑human studies for several reasons:
- Streamlined early‑phase processes. The Clinical Trial Notification or Exemption routes allow ethics‑approved studies to commence with prompt regulatory acknowledgment, which can compress startup timelines.
- Experienced Phase 1 infrastructure. Dedicated units, standardized procedures, and close integration with imaging and biomarker labs help small companies generate clean data quickly.
- Cost and speed. Startup and operational costs can be lower than in the United States, and contracting with a single site network can simplify logistics.
There are tradeoffs. Data packages must ultimately align with FDA expectations, which can mean additional preclinical work or bridging studies later. If the compound is brain‑penetrant, imaging and cerebrospinal fluid sampling harmonized to US standards will matter. Finally, recruitment pools may differ, so inclusion and exclusion criteria must consider lifestyle and comorbidity profiles that affect generalizability.
What to watch: biomarkers and early readouts
If Retro runs a classic single‑ascending dose followed by multiple‑ascending dose design, the primary outputs will be safety, tolerability, and pharmacokinetics. To turn that into a credible Alzheimer’s program, the team will need exploratory pharmacodynamics and disease‑linked signals. Expect a layered biomarker strategy.
- Pharmacokinetics and brain exposure. Plasma PK is table stakes. If RTR242 crosses the blood brain barrier, a CSF to plasma ratio or a cerebrospinal fluid concentration time curve will be a powerful early signal. If it is not brain penetrant, the mechanism would need to act peripherally to shift central proteostasis through immune or metabolic intermediates, which is possible but harder to prove early.
- Autophagy flux in human cells. In blood, ex vivo stimulation and blockade assays can estimate flux by measuring LC3‑II turnover and p62 or NBR1 degradation in PBMCs. A rise in LC3‑II with lysosomal blockade and a fall in p62 without blockade are consistent with increased flux. Gene expression panels of autophagy regulators, along with lysosomal markers like LAMP1 and cathepsin processing, can round out the picture. This is not as clean as directly imaging flux in brain, but it provides a mechanistic foothold.
- Proteopathy markers. Modern Alzheimer’s trials lean on plasma and CSF p‑tau217 or p‑tau181, Aβ42 to Aβ40 ratio, neurofilament light chain, and GFAP. Autophagy activation could conceivably lower p‑tau species by accelerating intracellular clearance or altering kinase and phosphatase balance, and could lower NfL if axonal injury slows. Any movement on these markers in a Phase 1b cohort would be notable even without cognitive change.
- Imaging. Amyloid and tau PET will likely be too slow or costly for early dose finding, but MRI volumetrics and diffusion markers of microstructure could be included if the study enrolls mild cognitive impairment or early Alzheimer’s. Imaging‑enabled substudies often pay off later when selecting doses for Phase 2.
- Cognition and function. Short instruments such as MoCA or ADAS‑Cog can be insensitive over weeks. Digital composites, smartphone tasks, and sleep or activity measures provide continuous signals that might catch early benefit or side effects. The key is to prespecify minimal clinically important differences to avoid wishful thinking from noisy data.
Safety, risk, and the realistic timeline
Autophagy is a stress response. Turning it up is not inherently benign. The principal risks to monitor include:
- Metabolic overreach. Chronic autophagy activation could tip cells toward excessive catabolism. Watch for unintended weight loss, muscle weakness, or impaired wound healing if pathways intersect with mTOR or AMPK.
- Immune modulation. Autophagy intersects with antigen presentation and pathogen handling. Both immunosuppression and unwanted immune activation are theoretical risks. Track infection rates, vaccine responses if applicable, and cytokine profiles.
- Cancer interplay. Autophagy can suppress tumor initiation by clearing damaged organelles, yet established tumors sometimes rely on autophagy to survive stress. Early trials will exclude participants with active malignancy, but long follow up will be important for signal detection.
- CNS specifics. If RTR242 penetrates the brain, look for mood changes, sleep disruption, headache patterns, and seizure threshold shifts, all routine in CNS safety monitoring.
- Drug interactions. Because autophagy knobs may touch nutrient sensing, be cautious with concomitant rapalogs, metformin, or strong CYP modulators until the pathway and metabolism are mapped in humans.
As for timeline, a clean Phase 1 with a small Phase 1b cohort could complete enrollment and primary analyses within 12 to 18 months from first dose. That points to initial human safety and mechanistic signals in 2026, with Phase 2 possibly starting in 2027 if everything breaks right. That is an optimistic path for any new CNS agent, even more so for a first‑in‑class aging‑mechanism drug.
The AI kicker: what GPT‑4b micro suggests about reprogramming
OpenAI and Retro’s collaboration used a biology‑specialized model to propose redesigned SOX2 and KLF4 sequences that Retro screened in human fibroblasts. The reported outcome was a step‑change in reprogramming markers and a drop in DNA damage signals, validated across donors and cell types. The companies summarized the technical approach and the headline results in August 2025, outlining OpenAI’s GPT‑4b micro results.
Why is this relevant to an autophagy pill for Alzheimer’s? Three reasons:
- Shared hallmarks. Proteostasis and genome integrity are entangled hallmarks of aging. If AI‑designed factors accelerate safe partial reprogramming while reducing DNA damage, and a drug like RTR242 safely restores cellular housekeeping, the field begins to assemble a playbook that attacks aging biology from complementary angles.
- Platform credibility. A clinical win on RTR242 would not validate reprogramming directly, yet it would strengthen the case that Retro’s discovery engine and translational judgment can convert bold mechanisms into human data. That matters when the next step requires regulators to entertain reprogramming‑derived biologics or gene therapies.
- AI for wet lab speed. The most important sentence in the OpenAI disclosure is not the fold‑change number, it is the idea that a small, steerable model plus a well designed screen can compress a decade of protein tinkering into months. If that pace holds, longevity biotech shifts from waiting on slow serendipity to engineering on demand.
Of course, reprogramming brings its own risk profile. The historical concern is tumorigenicity from pushing cells too close to a pluripotent state. That is why delivery modality, dosing schedule, and engineered safety brakes matter. The OpenAI and Retro work focuses on factor design to improve efficiency and reduce damage, not on in vivo delivery in humans. Any therapeutic built on these factors will face intense scrutiny on insertional mutagenesis, off‑target epigenomic remodeling, and long term surveillance for neoplasia. A positive signal from RTR242 will not erase those risks, but it will shift investor and regulator psychology toward the view that aging mechanisms can be disciplined into druglike behavior.
What success would signal for longevity medicine
If RTR242 delivers in Phase 1 and an early patient cohort shows coherent biomarker movement, several dominoes fall:
- Geroscience in the clinic. The field gains a precedent that a core aging pathway can be modulated safely in humans with a brain indication and that the biomarker toolbox can register a response. That validates trial designs others can copy.
- A pivot from single target to systems pharmacology. Alzheimer’s drug development has rewarded specificity, often at the cost of breadth. An autophagy hit would support multi‑pathway strategies for complex age‑related conditions like Parkinson’s, ALS, and even frailty syndromes.
- Acceleration of AI‑designed therapeutics. Investors tend to fund what just worked. A clinical green light on a Retro program would strengthen confidence that the same discovery culture can bring AI‑designed proteins and gene circuits to IND‑enabling studies efficiently.
- A broader biomarker standard. If flux assays, modern plasma p‑tau, and NfL move together under autophagy modulation, those panels could become default in early neuro‑geroscience trials, improving comparability across companies.
If the trial disappoints, that will be informative too. A failure to see flux change at tolerated doses would send the team back to chemistry or delivery. A flux change without any shift in proteopathy markers would force a rethink of how pivotal autophagy is in human Alzheimer’s physiology at the adult stage. A safety signal would argue for narrower, localized strategies, for example CNS cell replacement or reprogramming ex vivo followed by cell therapy.
The bottom line
Retro is trying to thread a needle. On one end is a small molecule that should, in principle, help neurons take out the trash. On the other is an AI‑accelerated effort to rewrite some of the master switches of cell identity in a safer, more controlled way. The company does not have to win both bets at once. It needs one program to cross the clinical threshold while the other matures. Starting an Australian first‑in‑human trial of RTR242 while showcasing a credible advance in engineered reprogramming is a clear statement of intent.
If you care about longevity medicine moving from TED talks to treatment rooms, this is the moment to watch. The first biomarkers from RTR242 will tell us whether nudging cellular housekeeping can really move the trajectory of brain aging. The second story, AI‑assisted reprogramming, will show whether the tools of the 2020s can compress biology’s timelines enough to matter within a decade. Together, they sketch a path where aging biology becomes a clinical discipline, not a slogan.