Lilly’s Verve buy puts one-and-done LDL editing in reach
On July 25, 2025, Lilly closed its Verve acquisition, betting that in vivo base editing of PCSK9 could replace decades of statins with a single infusion. Early Phase 1b data show up to 69% LDL-C reductions, FDA Fast Track, and Phase 2 on deck.

The bet: one infusion instead of decades of adherence
On July 25, 2025, Eli Lilly completed its purchase of Verve Therapeutics, folding the gene editing upstart into a cardiometabolic powerhouse that already sells blockbuster incretins. It is not a small swing. The company is wagering that a single infusion that edits one gene in the liver could replace decades of pills and injections for people at high lifetime risk of heart disease. Lilly framed the move as a paradigm shift, and the timing fits: the company now controls Verve’s lead program, VERVE-102, which edits PCSK9 in vivo and is advancing from Phase 1b into Phase 2. If the bet pays off, cardiovascular prevention starts to look a lot more like a vaccine clinic than a monthly refill. For the record, Lilly says it has completed its Verve acquisition.
Lilly’s cardiometabolic strategy also intersects with GLP-1 medicines. For context on the expected population impact of incretins, see our GLP-1s at scale analysis.
How VERVE-102 works in plain English
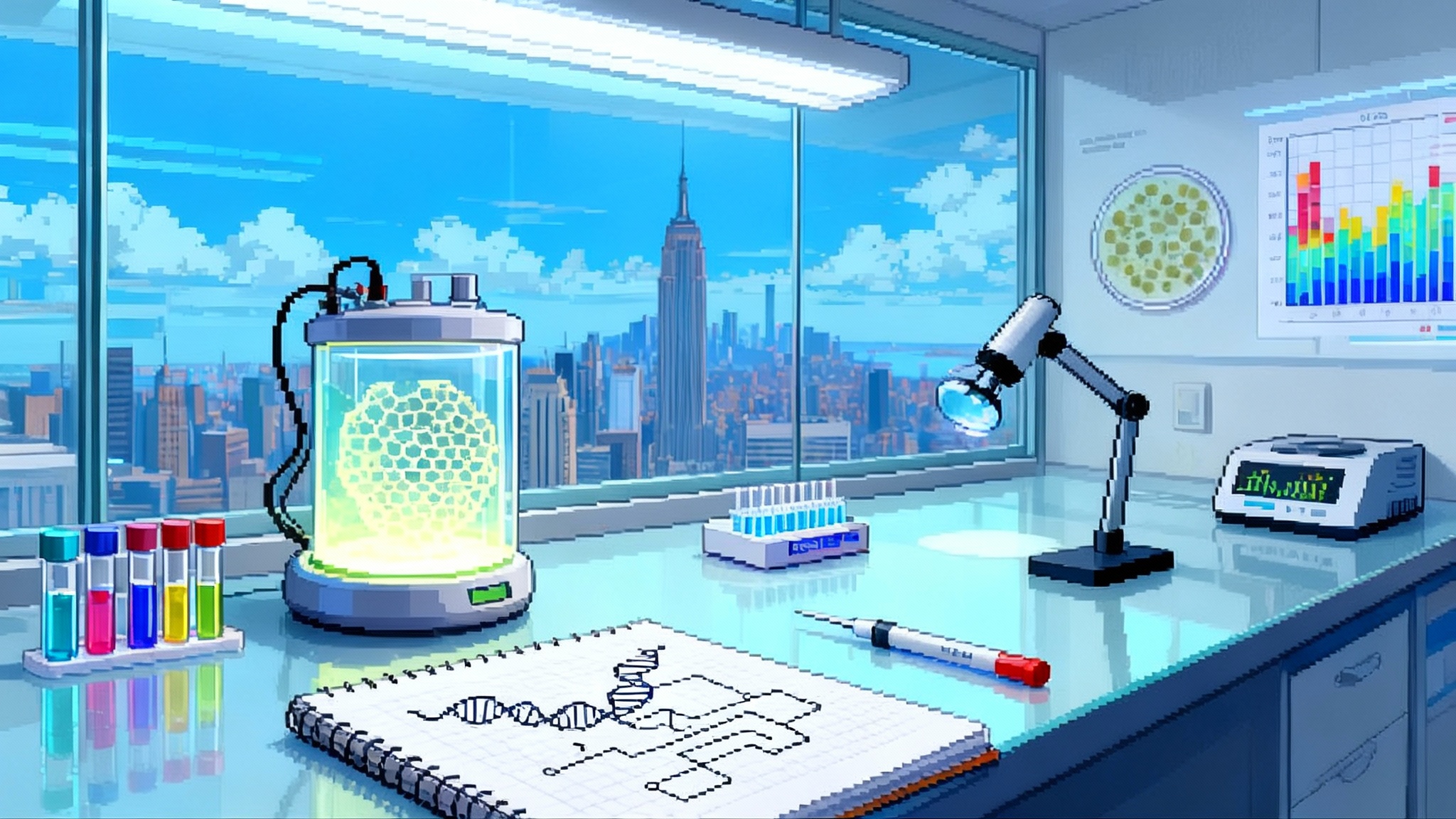
VERVE-102 delivers an adenine base editor and a guide RNA inside a lipid nanoparticle that homes to hepatocytes. Once inside the liver cell, the editor swaps a single DNA letter in the PCSK9 gene. That single change turns the gene off. With PCSK9 muted, LDL receptors recycle more efficiently and the liver clears LDL cholesterol from the blood more effectively. The idea is permanent LDL-C reduction from a one-time dose, because hepatocytes keep that change as they divide.
Two design choices matter for safety and potency. First, base editing does not cut both DNA strands like classic CRISPR. It makes a chemical conversion on one base, which can reduce double-strand break risks. Second, VERVE-102 uses a GalNAc-decorated LNP to engage the ASGPR pathway as well as LDLR, improving liver targeting and potentially lowering the dose needed. That design is a response to lessons from Verve’s first PCSK9 candidate, VERVE-101, which used a different LNP and saw a serious, transient safety signal that prompted a program pivot. VERVE-102 is the cleaner, more targeted iteration.
What the early data show
The first human data from the Heart-2 Phase 1b trial read out in April 2025. In 14 participants across three ascending dose cohorts, a single infusion produced dose-dependent drops in circulating PCSK9 and LDL-C. The highest cohort, 0.6 mg/kg, delivered a mean LDL-C reduction of 53%, with a maximum reduction of 69% in one participant. The emerging story is that total RNA dose, not just mg/kg, correlates with depth of editing, which is consistent with LNP-delivered nucleic acid drugs. Safety looked clean in this small data set: no treatment-related serious adverse events, no clinically meaningful elevations in liver enzymes, and no platelet drops reported through at least 28 days of follow-up. Verve has said the Phase 1b dose escalation will wrap with durability data in the second half of 2025, and that Phase 2 starts thereafter, subject to regulatory clearance. For the headline results, see Verve’s initial Heart-2 results.
Separately, the FDA granted VERVE-102 Fast Track in April 2025, which enables more frequent interactions and the possibility of rolling review. For a program built around a surrogate biomarker, those touchpoints with regulators will matter.
Why LDL editing is a longevity story
Atherosclerotic cardiovascular disease remains the leading global killer. Risk accumulates with time because arteries experience a long, quiet exposure to LDL-laden particles. The epidemiology is clear: lower LDL-C, for longer, yields larger absolute risk reductions. That is why lifelong genetic variants that keep LDL-C low confer striking protection, and it is why earlier and deeper LDL-C control in clinical trials translates to fewer heart attacks and strokes years later. For more on the strategy, see our explainer on how to edit once, lower for life.
VERVE-102 takes that principle to the limit. Rather than asking people to take a statin for decades, or to return for injections every month or every six months, it aims to create a one-time edit that pushes LDL-C down for years. If durability holds, the public health math gets interesting. Imagine reaching millions of midlife adults at high lifetime risk with a single infusion that keeps LDL-C down 50% or more. In settings where adherence to chronic therapy often fades within a year, a one-and-done approach could capture the full theoretical benefit of LDL lowering. We unpack this in a single edit to cholesterol.
The stakes for biomarkers and endpoints
The regulatory ground is familiar but not trivial. LDL-C is an accepted surrogate endpoint for high-risk lipid disorders. It earned that status through mountains of genetics, physiology, and outcomes trials with statins, ezetimibe, PCSK9 antibodies, and siRNAs. VERVE-102 builds on that foundation, but there are new scientific questions that only time can answer.
- Durability: How long do edited hepatocytes keep PCSK9 down in humans. VERVE-102’s 2025 durability readout will be the first real test of the current editor and LNP.
- Depth versus safety: Do we see a plateau around a 50% to 60% LDL-C reduction, or can dosing strategies safely drive deeper edits.
- Clinical outcomes: Regulators can approve on LDL-C for certain indications, but the long game for a broad prevention label will still pull toward hard endpoints like major adverse cardiovascular events.
The biomarker measurement itself will need rigor. LDL-C assays, non-HDL-C, apoB, and PCSK9 protein will all be followed. If editing creates very low LDL-C for a long time, the field will debate how low is low enough in primary prevention. The key will be harmonized, long-term follow-up that captures cardiovascular events, new diagnoses, and any late adverse effects that might emerge years after editing.
Safety and off-target risk, explained simply
Base editing changes a single letter of DNA. That is elegant, but it is still gene editing. The two broad risk buckets are editing where you do not want it and immune or infusion reactions you do not want.
- Off-target edits: These can happen when the guide RNA binds a similar sequence elsewhere. Modern guide design and off-target screening lower this risk, and the liver is a well-characterized target. Still, rare off-target edits could matter if they land in tumor suppressors or other vital genes. That is why regulators will scrutinize unbiased off-target profiling, and why long-term surveillance is essential.
- Immune and infusion reactions: The editor protein itself can stimulate immunity. Most people have some preexisting antibodies to Cas proteins, and repeated exposure could be a problem. VERVE-102 is a one-time treatment, which reduces the chance of multi-dose immune complications, but the first exposure still matters. LNPs can also cause infusion reactions, transient liver enzyme rises, or platelet changes. Early VERVE-102 data did not show clinically significant liver or platelet signals in a small sample. That is reassuring, yet it is not definitive.
Finally, lessons from VERVE-101 are relevant. That earlier program reported a serious but transient safety event and then gave way to VERVE-102 with a different LNP and GalNAc targeting. The upgrade was designed to boost hepatocyte uptake at lower total RNA doses. If the Phase 1b and Phase 2 data continue to show clean lab profiles and stable platelets, that will help the safety case considerably.
Reimbursement and equity: preventing a new prevention gap
The economics will be complex. A one-time gene editing infusion will likely carry a premium price that tries to bundle decades of value into a single payment. Payers will ask for clear eligibility criteria, robust LDL-C lowering, and a plan for outcomes follow-up. In the United States, coverage could start with heterozygous familial hypercholesterolemia and very high-risk secondary prevention patients, where LDL-C lowering as a surrogate is most established.
But longevity gains at scale require access beyond narrow genetic diagnoses. If VERVE-102 proves safe and durable, the case for broader primary prevention in people with high lifetime risk will be strong. That raises equity questions. Will safety-net systems adopt the therapy early, or will uptake cluster in well-resourced centers. Will pricing models include outcomes-based contracts and annuities to align up-front cost with long-term benefit. If the therapy prevents heart attacks 10 to 20 years out, who pays and who benefits when patients move between insurers. These are solvable problems, but they require proactive design so a one-time medicine does not widen the prevention gap.
What to watch next
- Durability from Heart-2 dose escalation. Look for multi-month to multi-year LDL-C and PCSK9 curves, plus any new safety flags as more patients cross six and twelve months.
- Phase 2 initiation and design. Inclusion criteria, dosing strategy, and whether the trial seeks a defined LDL-C target, a percentage reduction, or both.
- The ANGPTL3 program, VERVE-201. ANGPTL3 inhibition lowers remnant cholesterol and triglyceride-rich lipoproteins and may be especially useful in refractory hypercholesterolemia and HoFH. A coherent update in the second half of 2025 would add a second pillar to the platform.
- The Lp(a) program, VERVE-301. Elevated lipoprotein(a) is an independent causal risk factor for ASCVD and aortic stenosis. If base editing can durably suppress LPA, that would open a new front in lifetime risk reduction.
- Label path and surrogate acceptance. Watch whether regulators signal comfort with LDL-C as a primary endpoint in specific high-risk groups for registration, and what post-marketing outcomes commitments might look like.
- Manufacturing and delivery. Consistent, scalable LNP manufacturing and infusion workflows will matter as much as clinical efficacy if this becomes a population-level intervention.
The upside case for healthy lifespan
If VERVE-102 or a successor demonstrates three things, the longevity impact could be real and broad. First, consistent LDL-C reductions of 50% or more across diverse patients. Second, durable effect over many years with minimal drift. Third, a clean long-term safety profile with no pattern of late adverse events. Combined, those conditions would compress a large burden of first cardiovascular events into the never-happened category. That does not add birthdays so much as it shifts them into healthier territory.
Now add platform effects. If ANGPTL3 and Lp(a) join LDL-C in the single-dose toolbox, clinicians could personalize combinations based on genetics and baseline risk. Someone with high LDL-C and high Lp(a) might receive two edits over a few years and then never touch a statin or PCSK9 antibody again. That is science fiction turning into service line.
The cautionary notes
Science rarely grants free lunches. A one-and-done edit is not reversible. If a rare off-target effect emerges years later, pharmacovigilance needs to be robust and transparent. Sequencing surveillance, blood markers, and cancer registries will all play a role. The field also needs humility about biology in older, inflamed, or comorbid livers. Editing efficiency and safety could differ from fit midlife volunteers.
There are practical concerns too. Consent must be grounded and thorough. People deserve to understand what permanent means. Real-world data systems must be ready, because outcomes that justify broad prevention claims will take time to accrue.
Bottom line
With the Verve acquisition, Lilly placed a big, very specific bet on shifting cardiovascular prevention from chronic adherence to a single dose. Early data with VERVE-102 suggest that in vivo base editing of PCSK9 can push LDL-C down in the 50% to 60% range, with a maximum signal near 70% so far. FDA Fast Track and a Phase 2 start point to momentum. The scientific, regulatory, and economic questions are all answerable, but they require steady follow-through and long-term visibility.
If durability holds and safety stays clean, one-and-done LDL editing becomes a real longevity play. The payoff would be fewer heart attacks and strokes across the population, with gains measured not just in years added, but in years lived well.