Autophagy in the clinic: Retro's pill targets brain aging
Retro Biosciences plans to begin first-in-human testing of RTR242, an autophagy-boosting oral drug aimed at Alzheimer’s, by the end of 2025. Here is how cellular cleanup could translate into healthspan gains, the endpoints that matter, and the regulatory pathway most likely to deliver approval.
A quiet milestone for brain aging
Retro Biosciences says it will dose the first human with RTR242 by the end of 2025 in Australia, positioning an autophagy‑enhancing small molecule to tackle Alzheimer’s disease and potentially broader brain aging. The company’s plan, covered in a Business Insider report on RTR242, brings a durable geroscience idea into the clinic: restore cellular cleanup and you may slow age‑linked decline.
Why autophagy matters for the aging brain
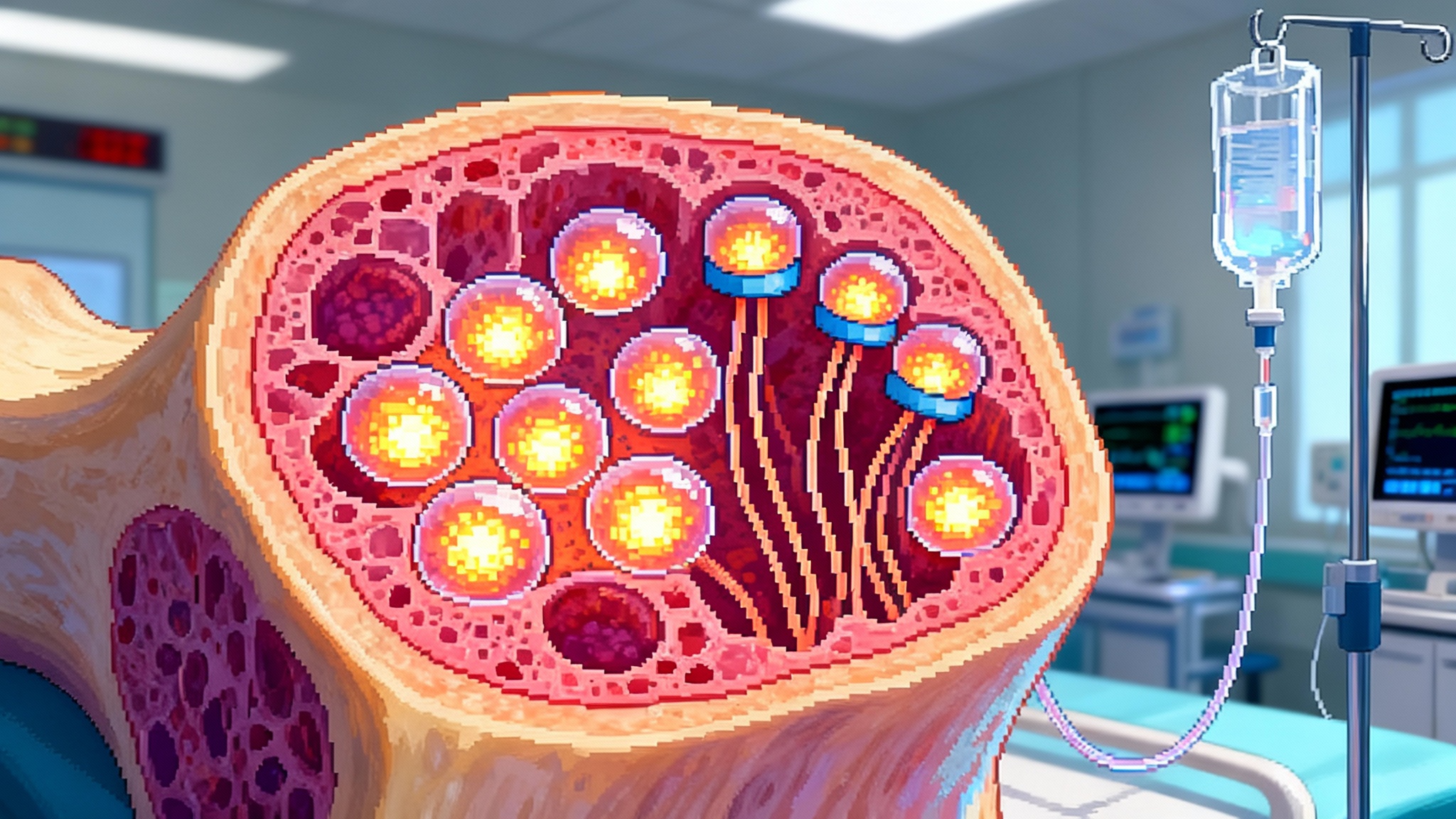
Cells preserve proteostasis by folding new proteins correctly and degrading damaged ones. Autophagy is the cleanup crew, routing worn components to lysosomes for breakdown. With age, this system clogs. Misfolded proteins accumulate, organelles drift off spec, and resilience falls. Neurons are especially vulnerable.
In Alzheimer’s, impaired cleanup collides with disease drivers. Amyloid and tau dominate headlines, but lysosomes can stall, autophagic vesicles pile up, and damaged mitochondria linger. An autophagy activator aims to restore throughput across the system. Do that and you could reduce toxic protein load while improving organelle quality control, stress responses, and cellular energy balance. For context, see our guide to autophagy basics.
A geroscience strategy regulators can evaluate
Aging is not an approved indication in the United States. The practical route is to prove benefit in a specific disease where the mechanism matters. Early Alzheimer’s fits that model and has a maturing playbook for clinical outcomes and biomarkers. The agency’s current view is summarized in FDA guidance for early Alzheimer’s. In plain language, the path exists. The trade is evidence.
What to watch as RTR242 moves forward
The initial Australian study will be a Phase 1 package focused on safety, tolerability, pharmacokinetics, and early pharmacodynamic signals. The value proposition shows up in the next stage, likely in prodromal or early Alzheimer’s populations.
1) Cognition and function people feel
- Sensitive cognitive composites such as the Preclinical Alzheimer Cognitive Composite and the Integrated Alzheimer’s Disease Rating Scale can detect small but meaningful shifts over 6 to 12 months.
- Functional measures tied to daily life, like managing finances or medication schedules, offer patient‑centered evidence that maps to real outcomes. For more, see our primer on Alzheimer’s endpoints.
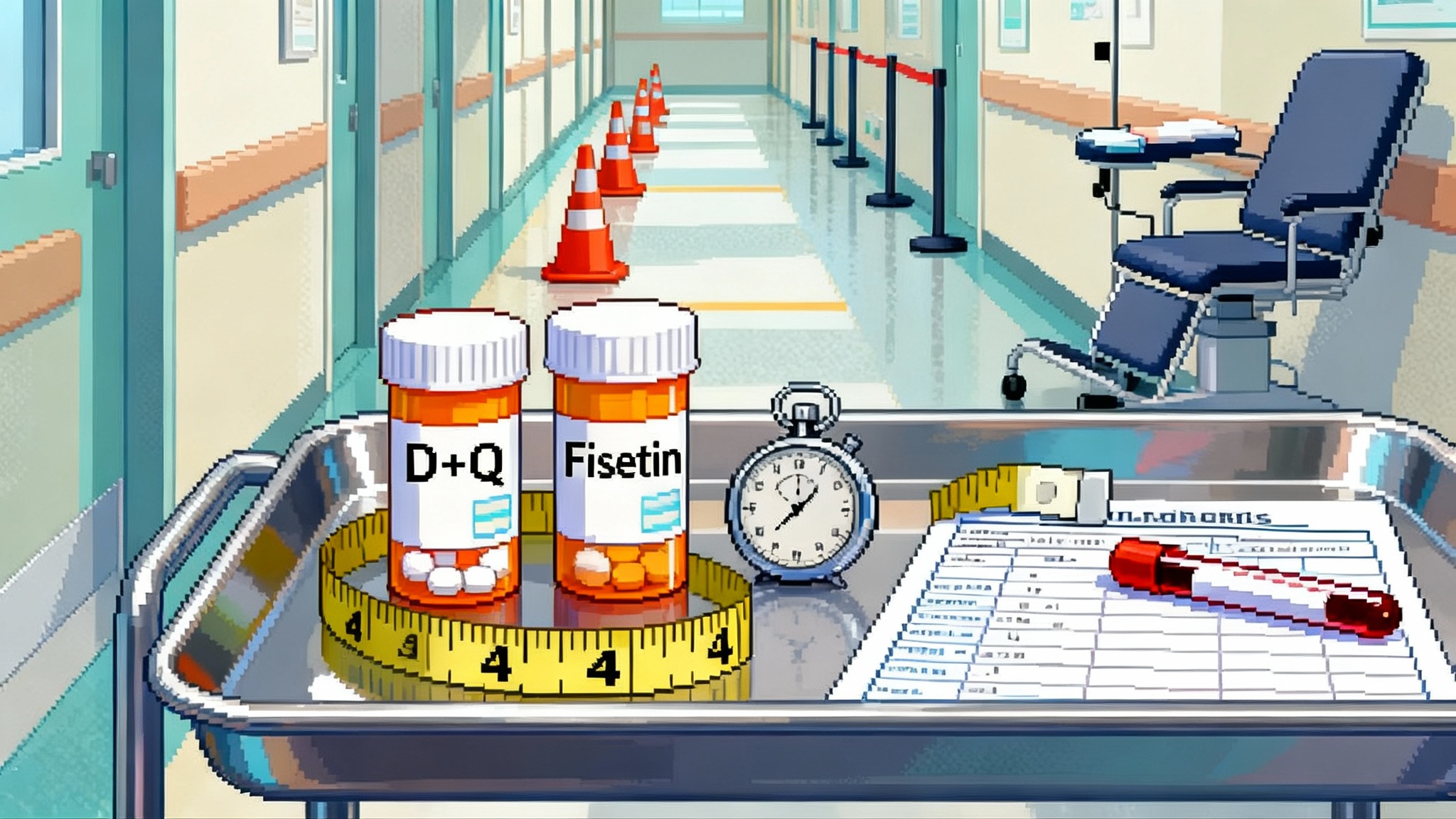
2) Fluid biomarkers that track biology
- Alzheimer’s activity: Plasma and CSF p‑tau217 and p‑tau181, Aβ42/40 ratio, neurofilament light chain, and GFAP are leading indicators in early disease.
- Autophagy pharmacodynamics: Ex vivo LC3 turnover, p62 dynamics, or lysosomal enzyme activity in peripheral cells can show the drug is engaging the cleanup machinery.
3) Aging‑system measures that widen the claim
- Epigenetic clocks and other pace‑of‑aging measures can be exploratory signals alongside clinical outcomes.
- Digital phenotypes from speech, gait, sleep, and real‑world assessments can connect cellular mechanism to function. Related perspective: how healthspan trials are evolving.
The mechanistic case for proteostasis in neurodegeneration
Autophagy sits where multiple Alzheimer’s pathologies converge. Enhancing clearance can relieve stress across tau aggregation, mitochondrial damage, oxidized proteins, and lipofuscin. Animal data suggest improvements in pathology and behavior, and human observational evidence aligns lifestyle levers that raise autophagy with better brain health. None of this guarantees a clinical win, but it raises plausibility.
Competitive context and the clinical bar
Amyloid‑targeting antibodies can slow decline in early disease, yet they require infusions and intensive monitoring. A safe oral small molecule with modest cognitive and functional benefit would be meaningful and easier to scale. Success does not require beating every antibody on every metric. It requires clearing a patient‑centered bar with a mechanism that generalizes across brain aging.
Trial design principles that will matter
- Precise staging: Amyloid‑positive early Alzheimer’s or MCI due to Alzheimer’s provides better signal‑to‑noise over 6 to 12 months.
- Tight hierarchy of outcomes: One or two primaries that matter clinically, with secondaries and biomarkers aligned to mechanism, and a prespecified analysis plan that controls multiplicity.
- Biomarker packages used wisely: Biomarkers should illuminate the clinical story rather than replace it.
- Real‑world validation: Pragmatic studies that track function, falls, hospitalizations, caregiver burden, and adherence will bolster value and access.
Why small molecules may arrive before reprogramming
Partial reprogramming is promising but hard to control, with open questions around identity, growth, dosing, delivery, and long‑term safety. Oral small molecules are manufacturable at scale, fit existing care pathways, and can be evaluated with large safety datasets. If they engage network hubs like autophagy, they can influence multiple age‑related processes. Effect sizes may be modest and may require careful selection or combinations, which aligns with real clinical practice.
Bottom line
By centering on cellular housekeeping in a disease where housekeeping fails, Retro is testing a simple thesis with potentially broad benefits. If data over the next few years show that an autophagy modulator improves cognition, function, and biology, it could become a deployable mechanism‑driven tool for brain healthspan.