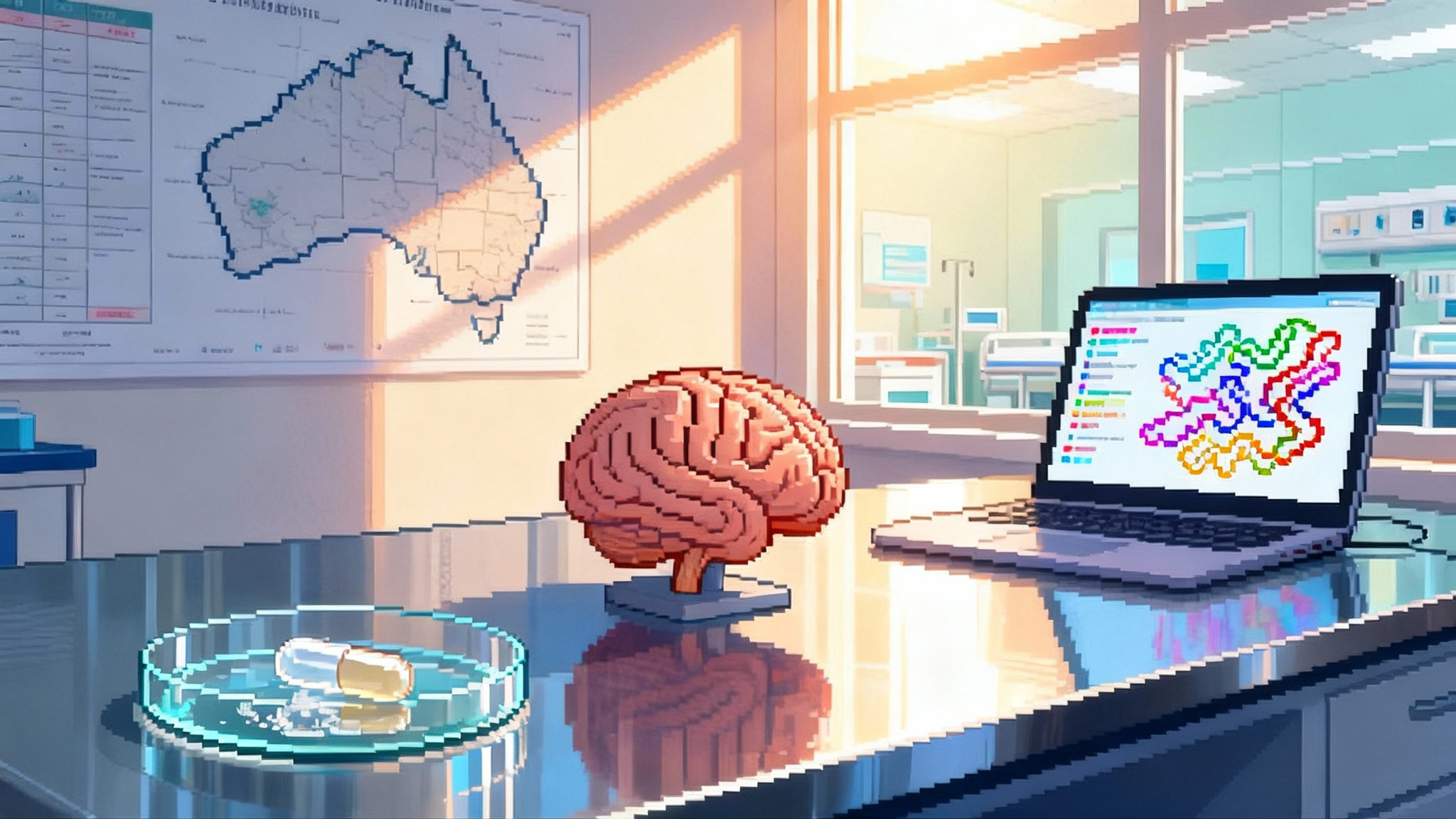
UK Biobank’s 500k proteomes will redefine aging biomarkers
Starting in January 2025, UK Biobank began profiling thousands of plasma proteins across 500,000 participants. The dataset could validate or retire today’s aging clocks, enable earlier disease prediction, and set a higher evidence bar for longevity care.
The population-scale proteome finally arrives
On January 10, 2025, UK Biobank announced a project with a simple premise and enormous implications: quantify thousands of proteins in the blood of every one of its 500,000 participants, plus 100,000 second samples collected up to 15 years later. The first wave covers 300,000 samples, with data released to the global research community in stages from 2026 and the full dataset expected by 2027. Members of the biopharma consortium that funded the initial tranche receive a short, nine month head start before the wider research release. This is the first time true population-scale proteomics meets deep longitudinal phenotyping, whole genome sequencing, and imaging in a single cohort. It sets the stage to rethink how we measure biological aging and predict disease risk. See the official UK Biobank plan and timeline.
What is being measured and why it matters
Proteins are the dynamic layer of human biology. Genes are relatively stable. Proteins change with time, lifestyle, environment, and disease. UK Biobank will quantify about 5,400 plasma proteins per person using a high throughput affinity panel. The protocol includes:
- 500,000 baseline blood samples taken at enrollment
- 100,000 repeat blood samples from the same participants up to 15 years later
- Protein detection run at industrial scale to complete the first 300,000 samples in roughly a year
Two features make this resource unique:
-
Longitudinal signal. The repeated samples let researchers see how proteins drift within people, not just across people. That is the foundation for credible aging biomarkers, because aging is defined by change within an individual over time.
-
Context-rich outcomes. Every participant is tied to electronic health records, imaging, lifestyle, and genetics. A single proteomic profile can be tested against thousands of outcomes ranging from incident dementia to cancer subtypes to cardiovascular events, with time-to-event precision.
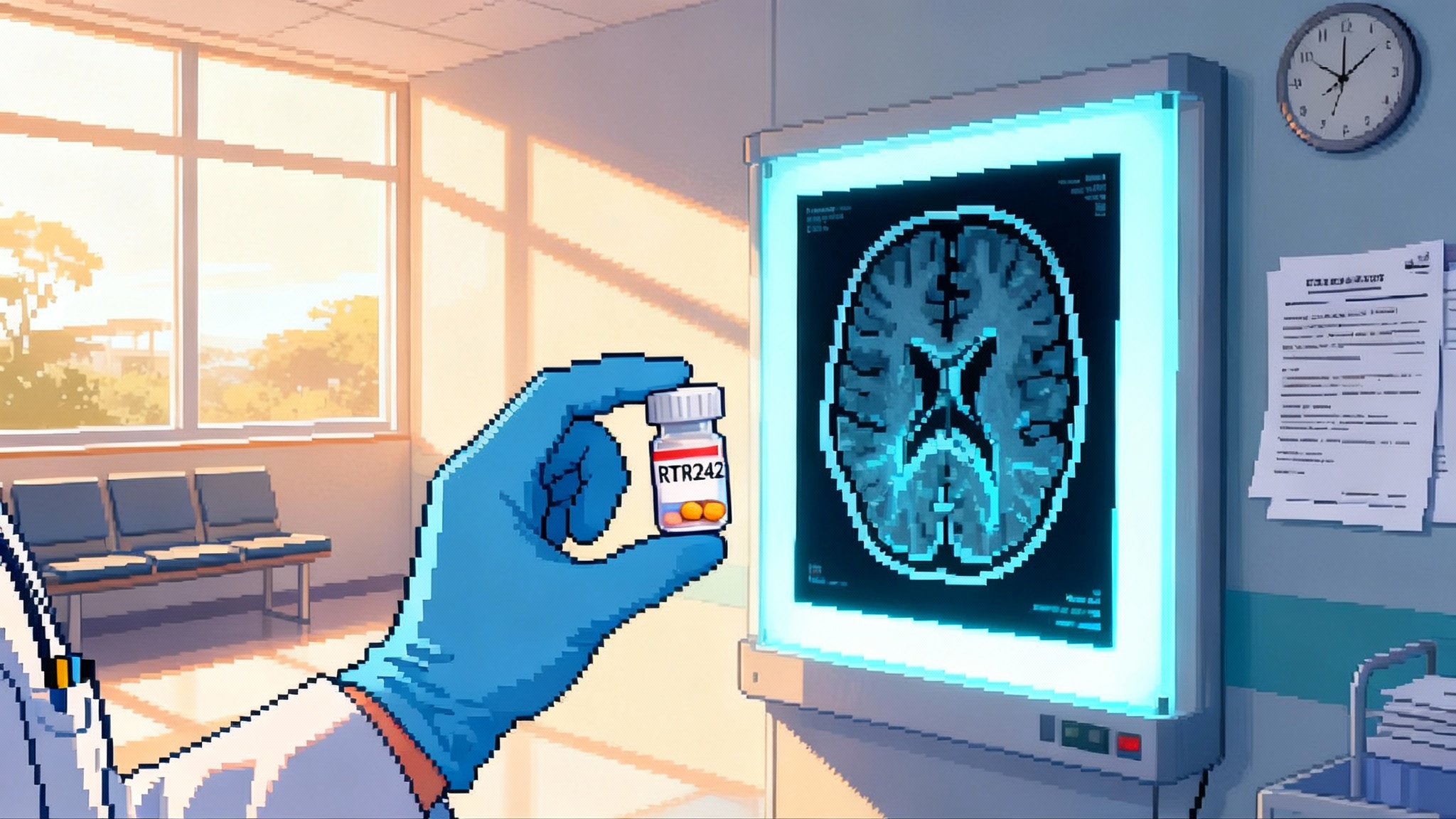
Aging clocks meet their moment of truth
Aging clocks have boomed over the past five years across DNA methylation, proteins, and metabolites. Many show strong correlations, but when asked to predict hard outcomes such as mortality, hospitalizations, or incident disease, performance varies and transportability often fails.
The UK Biobank proteome will force clarity, quickly:
- Cross-sectional versus longitudinal aging. With repeat samples on 100,000 people, researchers can quantify within-person proteomic aging rates and link those trajectories to later outcomes.
- Event-anchored validation. At scale, clocks can be tested on their ability to predict specific events at 1, 3, 5, and 10 years using time-dependent AUC, integrated Brier score, and net reclassification improvement against clinical baselines.
- Causal flags. Proteomic signals can be triangulated with genetics to infer whether a protein is on the causal path. Correlates without genetic support and weak longitudinal dynamics are likely passengers, not drivers.
- Transportability and fairness. With half a million participants across regions and socioeconomic strata, researchers can test behavior across age groups, sexes, deprivation indices, and multimorbidity.
A likely outcome is a thinning of the field. Some clocks will fail on transport or longitudinal tests. Others will emerge with stronger, disease-agnostic predictive power and clear calibration plans.
Earlier disease prediction moves from promise to playbook
Large studies already suggest proteomic signatures can flag cancer, neurodegeneration, cardiometabolic disease, autoimmune flares, and severe infections years before diagnosis. What UK Biobank adds is scale, breadth, and timeline alignment.
- Scale. The first 300,000 samples alone enable development and validation across thousands of endpoints, including rare diseases and early onset events.
- Breadth. A single panel can reflect inflammation, extracellular matrix remodeling, vascular signaling, and neuronal stress, supporting multi-disease risk stratification that matches real-world practice.
- Timeline. Staggered releases beginning in 2026 mean validated risk models could flow into trials and health system pilots within the next 24 months. Full release in 2027 enables comprehensive meta-analyses and external validations.
The practical gains could include pre-symptomatic referral thresholds, risk-tailored screening schedules, and earlier intervention windows for conditions like heart failure, type 2 diabetes, and several cancers. For clinical relevance, models can also be evaluated against all-cause hospitalization and mortality.
Who is paying for it and what they get
The initial 300,000-sample tranche is funded by a consortium of 14 biopharma companies. Per UK Biobank access rules, the consortium receives a short period of exclusive access before the data become available to all approved researchers. In June 2025, the UK Government committed £20 million to complete the full 500,000 participants plus the 100,000 repeat samples, signaling that this dataset is national research infrastructure. See the government funding commitment.
What gets released when
UK Biobank has specified a staged plan:
- Data generation for the first 300,000 samples takes about a year from the January 2025 launch.
- Consortium members have nine months of exclusive access to each tranche.
- Staggered releases to all approved researchers begin in 2026 via the Research Analysis Platform.
- The full proteomic dataset is expected on the platform by 2027.
Researchers should plan for rolling availability. If a question depends only on baseline protein levels and common outcomes, work can likely start as soon as the first tranche opens. If the analysis requires repeat samples, rare diseases, or extensive imaging linkage, plan for later in the release cycle.
How this could change prevention and primary care
Prevention hinges on two things: identifying who is truly at risk and acting early enough to matter. The proteomic dataset can elevate both.
- Risk tiers that move outcomes. With such a large cohort, researchers can set risk thresholds that map to absolute event rates, supporting decisions like statin initiation, GLP-1 allocation, or early cardiology referral. For cardiometabolic strategy context, see our analysis of GLP-1 longevity math.
- Timing. Longitudinal protein trajectories can reveal when risk accelerates, enabling dynamic follow-up intervals instead of fixed annual cycles.
- False positives and harm minimization. The dataset allows rigorous assessment of downstream testing cascades, measuring scans, incidentalomas, and procedures per case found, not just AUC.
Primary care teams could eventually receive proteomic scores alongside cholesterol, A1c, and eGFR in the EHR. The first credible prototypes could be piloted by health systems within two years where actionability is clear.
A new evidence bar for longevity clinics and startups
Longevity offerings often sell age scores and claim that supplements, diets, or drugs lower biological age. Without event-level validation, those claims are not clinically meaningful.
UK Biobank’s proteomes set a higher standard:
- Outcome-anchored endpoints. If a clock or intervention claims to slow aging, show that the clock changes in the expected direction and that those changes track lower hospitalizations, mortality, and disease onset in external validation.
- Benchmarks that matter. Compare against robust baselines like QRISK, pooled cohort equations, or simple age plus BMI models.
- Registered analysis plans. Pre-specify endpoints, windows, and validation rules. Declare handling of missingness, batch effects, and multiplicity. Test on hold-out data or future waves.
- Intervention claims. Therapeutic claims should include randomized or quasi-experimental designs with proteomic endpoints and clinical outcomes. For perspective on contentious interventions, see our review of plasma exchange and aging.
Startups that embrace these rules will stand out to payers and regulators. Those that do not will look increasingly out of date once the first UK Biobank proteomic papers land.
Implications for trials and drug development
Proteomic readouts can accelerate trials in several ways:
- Enrichment. Use proteomic risk scores to identify high event rate subgroups, shortening trials or reducing sample size without sacrificing power.
- Pharmacodynamic markers. If a drug targets a pathway with a measurable protein, on-treatment changes can serve as early success signals and help with dose selection.
- Subtyping. Proteomic profiles can split clinically similar diseases into biological subtypes with different therapy responses.
- Surrogacy exploration. With event data, researchers can test whether early proteomic changes mediate clinical benefit. For a related cardiometabolic example, see our coverage of the PCSK9 editing bet.
Reimbursement and regulatory outlook
Payers will ask three questions about proteomic tests: do they predict outcomes better than current tools, do they change decisions, and do those decisions improve outcomes at acceptable cost. UK Biobank makes it feasible to answer all three.
- Better than standard of care. Expect head-to-head comparisons of proteomic scores with guideline models across many diseases.
- Decision impact. Using linked prescribing and outcomes data, researchers can model how acting on a proteomic score would shift therapy thresholds.
- Cost-effectiveness. The scale allows realistic modeling of downstream costs from false positives, scanning burden, and treatment side effects.
Regulators tend to welcome assays that improve risk stratification when paired with clear action pathways and post-marketing evidence plans. Tests that drive correctable interventions will see smoother paths than tests that only label risk.
Limits and open questions
This project is a leap forward, not a magic wand. Key issues include:
- Batch and platform effects. Even with careful QC, platform updates can introduce shifts. Robust normalization and cross-wave calibration will be essential.
- Clinical translation. Affinity panels are research grade. Translating multi-protein signatures into validated clinical assays requires targeted platforms, reference ranges, and CLIA-grade validation.
- Generalizability. UK Biobank participants are healthier at baseline than the general population. External validations in more diverse cohorts are needed.
- Mechanism versus marker. Not every predictive protein is causal. Drug targets require genetic and experimental triangulation.
- Privacy and equity. As models become more powerful, teams must monitor for hidden biases and ensure benefits reach underserved populations.
The 24 month outlook
- Through 2025. Data generation continues for the first 300,000 samples. Consortium teams run early analyses during their short exclusive period and prepare manuscripts and tools.
- 2026. First public tranches land on the Research Analysis Platform. Expect a wave of method papers, external validations of existing aging clocks, and new multi-disease risk models. Health systems and payers begin piloting targeted use cases.
- 2027. Full dataset expected. Meta-analyses, cross-wave calibration papers, and stronger surrogacy claims appear. Regulators entertain submissions that cite these data as external controls or validation backbones.
By the end of this window, many marketed aging clocks will have been validated, recalibrated, or quietly retired. A smaller set will meet clinical standards and support reimbursement arguments.
What to do now
- Researchers. Pre-register analyses, define primary endpoints that payers care about, and lock in hold-out strategies. Plan to use repeat samples for longitudinal validation.
- Clinicians and health systems. Identify two or three conditions where earlier detection clearly changes care. Prepare pathways for what to do when a proteomic score flags high risk.
- Startups. Build for translation. Aim for signatures that can run on clinical platforms with clear reference intervals. Assemble economic models now, not later.
- Payers. Define decision thresholds and evidence standards in advance. Consider coverage for pilot programs with outcomes tracking to de-risk adoption.
The bottom line
Population-scale proteomics is no longer a slide deck. It is running now, with staged releases that will reshape biomarker science over the next two years. Aging clocks will either earn their keep or exit the stage. Disease prediction will become more precise and practical. Most importantly, evidence will strengthen to the point where prevention can be planned, reimbursed, and delivered at scale. That is the promise when 500,000 proteomes meet rigorous outcomes data in the world’s best characterized cohort.