Biannual RNAi for Hypertension Enters Global Outcomes Trial
ESC 2025 delivered first KARDIA-3 results for zilebesiran and a green light from Roche and Alnylam for ZENITH, a global cardiovascular outcomes trial. Here is what twice yearly blood pressure control could mean for adherence, safety, healthspan, and equity.

The moment hypertension care has been waiting for
At ESC Congress 2025 in Madrid, the KARDIA-3 study of zilebesiran, an investigational RNA interference therapy that turns down hepatic angiotensinogen, took the Hot Line stage. The headline was nuanced but important: a single 300 mg subcutaneous dose led to a placebo adjusted 5 mmHg reduction in office systolic blood pressure at month three in high risk patients with uncontrolled hypertension on multiple drugs, with control maintained through month six. The overall multiplicity adjusted test was not met, but predefined analyses pointed to who may benefit most, especially those on a diuretic with baseline systolic pressure above 140 mmHg. That readout set the table for what came next: Roche and Alnylam confirmed they are moving ahead with a global Phase 3 cardiovascular outcomes trial. Together, those two facts mark the strongest signal yet that hypertension care may be shifting from daily pills to twice yearly injections. For core details, see the ESC press summary on KARDIA-3.
What makes zilebesiran different
Zilebesiran is a GalNAc conjugated siRNA that silences angiotensinogen in hepatocytes. That target selection matters. Angiotensinogen sits at the top of the renin angiotensin aldosterone cascade that regulates vascular tone and sodium balance. By reducing the supply of angiotensinogen itself, zilebesiran aims to flatten the whole RAAS axis downstream, not just block one node. The GalNAc tag delivers the siRNA into liver cells via the asialoglycoprotein receptor. Once there, the RNAi machinery degrades angiotensinogen mRNA, which lowers protein levels for months. The result is a pharmacology curve more like a platform than a peak: relatively smooth, durable suppression that does not depend on taking a pill every morning.
Hypertension is a textbook adherence disease. It is usually silent, the pills are cheap yet numerous, and the benefits of control are deferred while the costs are immediate. Even in well resourced systems, a significant share of patients do not reach their blood pressure targets. The appeal of a twice yearly injection is obvious. It converts a daily behavioral task into two planned health care moments a year. If the effect is durable, stable, and safe, it could close an adherence gap that has resisted decades of education and reminder apps.
Reading the KARDIA program as a whole
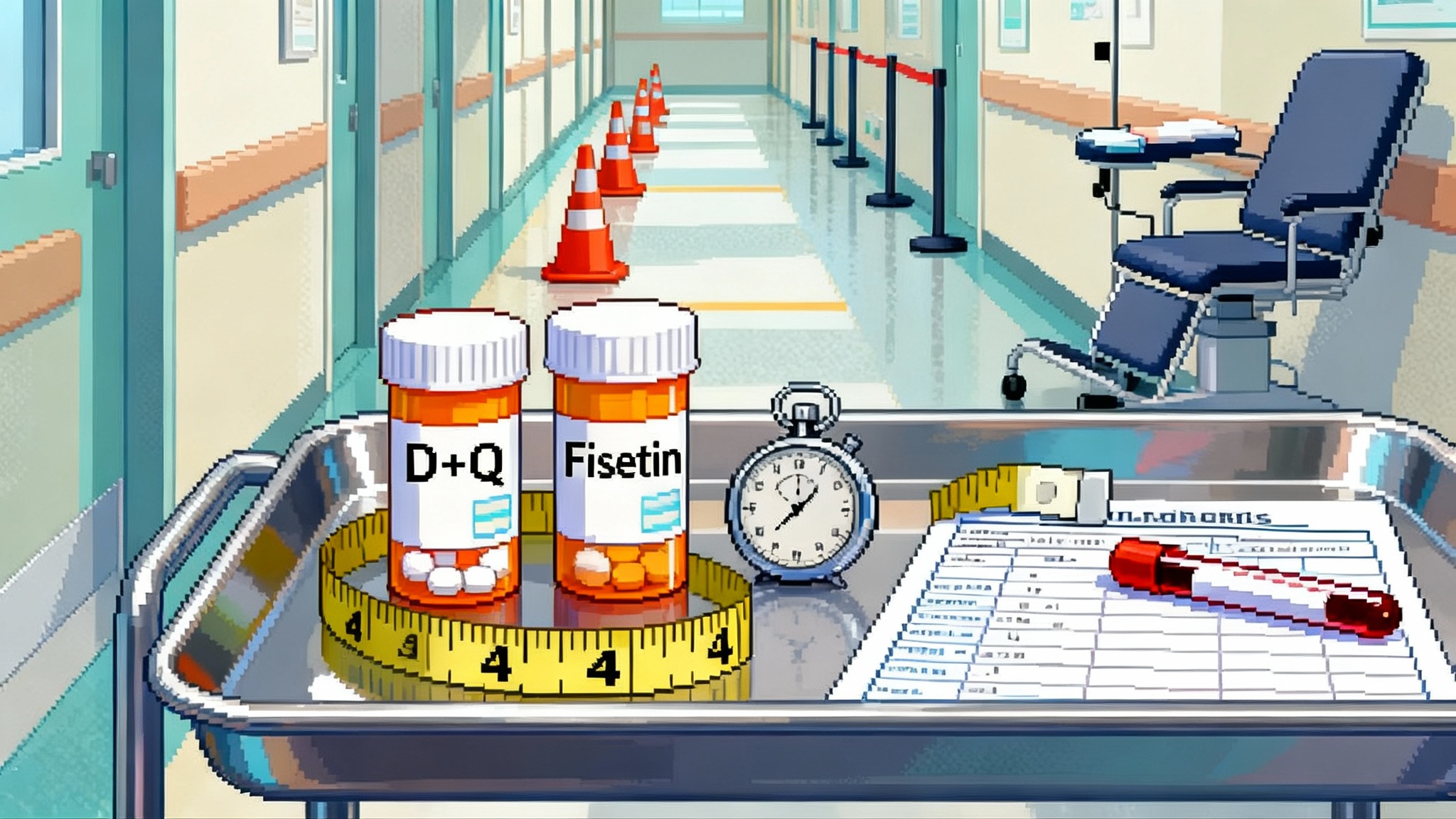
KARDIA-1 showed monotherapy blood pressure reductions with biannual dosing. KARDIA-2 established that adding zilebesiran to standard antihypertensives can enhance control. KARDIA-3 pushed into a tougher population: people at high cardiovascular risk with uncontrolled hypertension despite two to four drugs. In that context, KARDIA-3’s overall month three office systolic reduction of about 5 mmHg versus placebo, while not meeting the strict multiplicity adjusted threshold, is clinically relevant and aligns with a pattern seen before. The most compelling signal was in the subgroup on a diuretic with baseline systolic pressure over 140 mmHg, where placebo adjusted reductions approached 9 mmHg at month three and remained strong at month six. Safety across the program has been encouraging, with serious adverse events similar to placebo in the six month double blind period and no deaths reported in that window.
The take home is not that zilebesiran is a magic bullet. It is that an upstream RAAS silencer can add steady control on top of background therapy, particularly when combined with a diuretic. That combination makes physiologic sense. Diuretics relieve sodium and volume load, while RAAS suppression counters vasoconstriction and neurohormonal compensations. If the most benefit accrues where baseline pressure remains high despite standard combinations, that is exactly the cohort clinical practice struggles to control.
From blood pressure to outcomes
Blood pressure itself is a validated surrogate for cardiovascular risk. Still, the field has been burned before by drugs that looked promising on surrogates yet failed on hard events. That is why the next step matters. Roche and Alnylam are launching ZENITH, a global, event driven Phase 3 cardiovascular outcomes trial enrolling roughly eleven thousand patients with uncontrolled hypertension on at least two agents, one being a diuretic. The trial will test 300 mg every six months versus placebo added to standard of care. The primary endpoint is a composite of cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, and heart failure events that require hospitalization or urgent care. The sponsors expect to start ZENITH by the end of 2025, with timing of readout driven by event accrual rather than a fixed calendar. For design and rationale, see how Roche outlines ZENITH design.
For readers tracking timelines, event driven designs in similar risk populations often require several years to accrue endpoints, depending on background therapy and absolute risk. If enrollment begins in late 2025 and completes over 12 to 18 months, an outcomes signal may not emerge until the later 2020s. Interim analyses will be overseen by an independent data monitoring committee for safety. Whether regulators would consider a filing based on blood pressure lowering alone is an open question for a modality this novel and a program with mixed p values in its toughest Phase 2 cohort. The more likely path is to read out ZENITH.
Durability and safety so far
The essence of RNAi in hypertension is durability with predictability. The KARDIA data suggest that a single subcutaneous injection can deliver meaningful systolic reductions that persist through six months. That is not just convenient. It is a different rhythm of care. There is no daily fluctuation in drug exposure from missed pills, no weekly resets at the pharmacy counter, and less potential for drug holidays during travel or illness.
Safety remains central. The RAAS is ubiquitous in physiology, so upstream suppression raises reasonable concerns about hypotension, renin rebound, effects on renal hemodynamics, and interactions with ACE inhibitors or ARBs. The early signal is reassuring. In the double blind period of KARDIA-3, serious adverse events were numerically lower with zilebesiran than placebo, and no deaths occurred. Hyperkalemia, acute kidney injury, syncope, and orthostatic symptoms warrant continued monitoring, especially in older adults, those with chronic kidney disease, and people on potassium sparing regimens. Because zilebesiran is long acting, clinicians will want clear guidance for how to manage transient volume depletion from illness or heat, how to sequence background drugs if pressure falls too low, and how to handle the rare patient who needs rapid reversal.
The other safety domain is special populations. Pregnancy is a known contraindication for RAAS blockade because of fetal risks. Expect strict labeling and registries if and when the drug is approved. The RNAi platform brings additional specifics, such as liver targeting and the potential for off target transcripts. So far, the chemistry and delivery look clean, but outcomes trials often surface the rare events that small studies cannot see.
How twice yearly control could change healthspan
Hypertension is the midlife accelerator of cardiovascular aging. It stiffens arteries, feeds left ventricular hypertrophy, and primes the brain and kidney for microvascular injury. The good news is that millimeter by millimeter reductions translate to fewer events. A 5 mmHg drop in systolic pressure at the population level shifts the entire risk distribution toward safety. If you can deliver that drop in a durable, adherence agnostic way, you turn prevention into infrastructure.
Imagine a 50 year old with borderline metabolic risk who starts missing pills during stressful work months. Every skipped week raises the daily probability of an event by a tiny amount that compounds over decades. A twice yearly injection changes that equation. It compels at least two encounters per year where vitals are checked, refills are reconciled, and health advice is refreshed. It reduces the variance in exposure that makes real world effectiveness so much lower than trial efficacy. In actuarial terms, steadier control reduces tail risk. In lived terms, it buys quiet years of brain, heart, and kidney function.
For readers mapping the broader prevention stack, see how weight loss medicines may shift risk in GLP-1s 2025 healthspan inflection and how LDL lowering is evolving in PCSK9’s 2025 tipping point.
Complement, do not compete, with statins and GLP 1s
Zilebesiran is not a substitute for statins, PCSK9 inhibitors, ezetimibe, or GLP 1 receptor agonists. It targets a different axis. The most effective prevention in cardiometabolic disease is usually cumulative. Lipids, blood pressure, weight, and glycemia each contribute to vascular risk. Bringing them all closer to physiologic targets yields super additive benefit. In that frame, an RNAi antihypertensive is a plug and play addition to the modern prevention stack.
Mechanistically, the pairing with a diuretic looks especially helpful. That will matter if payers and guidelines require that background therapy be optimized. For patients on statins or PCSK9 therapy, there is no known pharmacokinetic reason zilebesiran would interfere. For those on GLP 1s, weight loss can itself lower blood pressure, so clinicians may want to taper background agents if orthostatic symptoms appear. The key is that these tools are orthogonal. They work together because they solve different parts of the same problem.
What to watch in ZENITH
Several design choices will shape how cleanly we can interpret ZENITH.
- Primary endpoint and components. The composite includes cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, and heart failure events requiring hospitalization or urgent care. Watch the mix. A signal driven by fewer heart failure admissions is still important, but a broad reduction across components would cement impact.
- Ambulatory blood pressure and nocturnal control. Office readings can miss nocturnal hypertension and variability that drive risk. A well designed ABPM substudy could show whether zilebesiran smooths the 24 hour curve and restores dipping.
- Background therapy standardization. KARDIA-3 hinted at synergy with diuretics. ZENITH requires at least two drugs including a diuretic. How tightly sites manage that background will determine how much additive effect can be attributed to zilebesiran versus optimization of existing pills.
- Renal outcomes and safety. Changes in eGFR, albuminuria, hyperkalemia rates, and acute kidney injury will be closely watched, especially in those with CKD or diabetes.
- Adherence dynamics. Even in a blinded outcomes trial, adherence to background oral therapy will vary. If zilebesiran attenuates the harm from missed pills, event curves may separate more in the real world than in the trial. Subanalyses using digital pill caps or pharmacy refill data could be revealing. For biomarker context, see UK Biobank proteome biomarkers.
Payer math and primary care workflows
RNAi therapies are not inexpensive. Payers will likely require step therapy, such as documented use of at least two or three generics including a diuretic and an ACE inhibitor or ARB, before approving a twice yearly injection. That is defensible if the goal is to reserve a novel agent for patients who remain uncontrolled. Yet it can also entrench inequity if the paperwork burden blocks access for those least able to navigate prior authorization.
The path through primary care matters. The simplest version is a standing order protocol: check creatinine and potassium, confirm background therapy, inject, schedule the next dose, and set a six week blood pressure follow up. Pharmacies or nurse led clinics can administer injections with point of care vitals. Remote monitoring between visits can catch hypotension or drift. For systems thinking in value based terms, reducing emergency visits and admissions for stroke, heart failure, and hypertensive crises creates budget room for a higher drug cost.
One underappreciated advantage is logistics. Two predictable injections per year fit cleanly into outreach models. Mobile clinics can set up in workplaces or community centers and deliver hypertension control at scale. That is a better match to the social reality of busy midlife adults than a stack of daily bottles on a nightstand.
Equity implications
Hypertension burden is not evenly distributed. It hits communities facing structural barriers to care. Daily adherence suffers where jobs are unstable, pharmacies are distant, and co pays compete with other bills. A twice yearly option could be a leveling force, but only if designed with equity in mind. That means broad coverage without punitive copays, flexible delivery sites, and culturally competent counseling about what an RNAi drug is and is not. Data sharing with trusted community clinics will matter as much as launch campaigns.
Guardrails against overreach
Enthusiasm is warranted, hype is not. The KARDIA-3 signal is promising but not definitive. The most optimistic path would have shown unequivocal superiority across the full study population at the prespecified primary endpoint. Instead, we have clinically meaningful reductions that appear stronger in a subgroup, a supportive safety profile, and a mechanistic rationale that hangs together. That is exactly why a large outcomes trial exists. It prevents us from anchoring a generation of care on inference alone.
Meanwhile, the day to day work of blood pressure control does not change. Optimize background therapy with combinations that patients can tolerate. Use diuretics early and often. Check adherence compassionately and creatively. Deploy GLP 1s, statins, and PCSK9 inhibitors according to guidelines. Zilebesiran, if and when approved, will be another tool. A compelling one if it delivers durable control without daily friction, but still one piece of a broader prevention strategy.
The bottom line
ESC 2025 nudged the field toward a new paradigm for hypertension. A liver targeted siRNA taken twice per year lowered blood pressure in high risk, hard to treat patients and did so with encouraging safety. Those data unlocked a global cardiovascular outcomes trial that will test whether biannual control can translate into fewer deaths, heart attacks, strokes, and heart failure admissions. If ZENITH confirms the promise, primary care could trade some pill burden for planned procedures, payers could exchange hospital costs for drug costs, and millions of midlife adults could carry a lower daily risk of catastrophe. That is prevention that is scheduled, steady, and simple enough to stick.