FDA Rollback Puts Biological Age Tests Back in Play
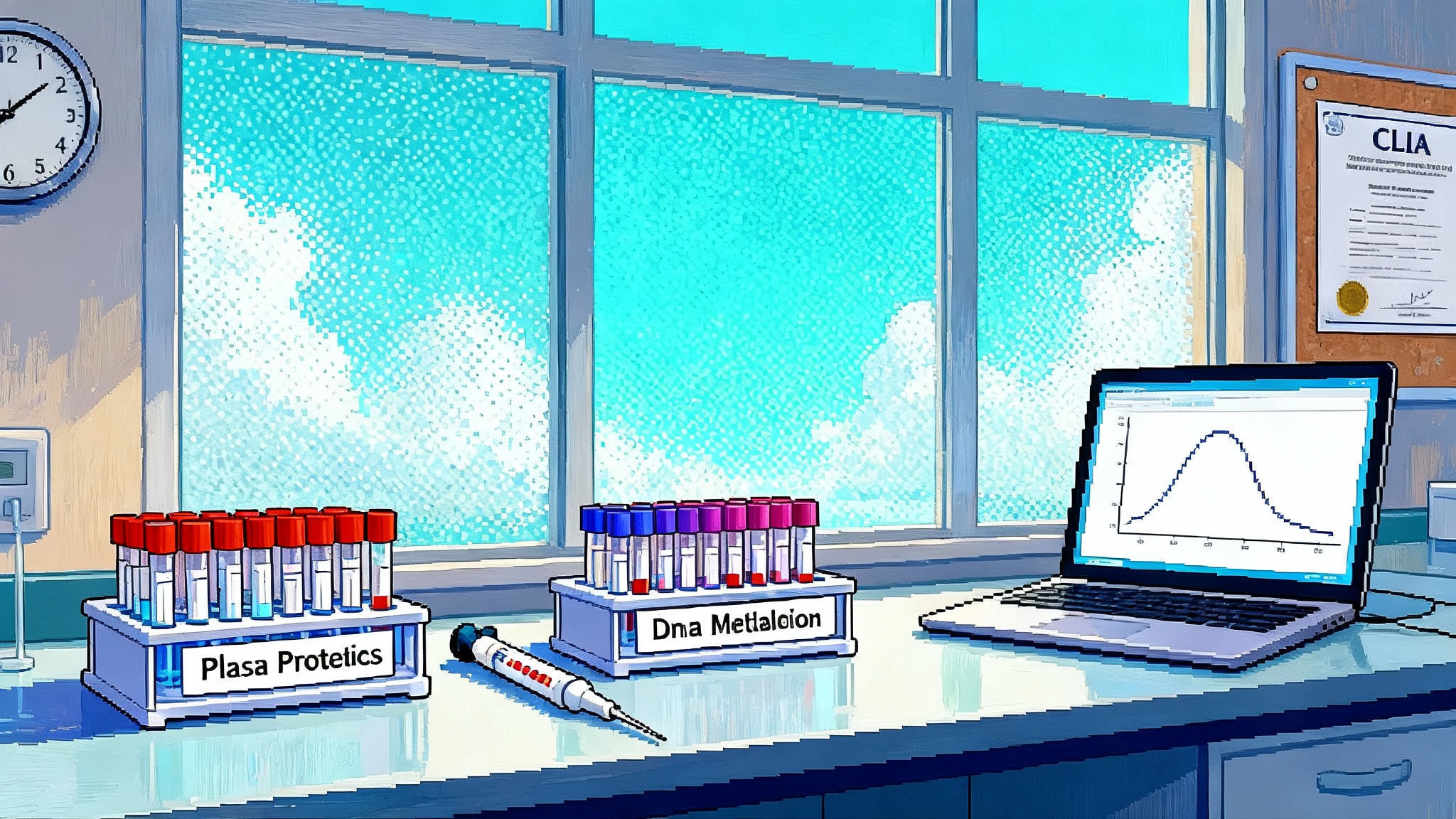
On September 19, 2025 the FDA implemented a court-ordered vacatur of its 2024 LDT framework, shifting oversight back to CLIA. Expect faster epigenetic clocks, proteomic age panels, and multi-omic biomarkers in clinics, along with greater variation in quality. Here is what changed and how to judge credibility.
The day the brakes came off
On September 19, 2025 the Food and Drug Administration published a final rule implementing a court-ordered vacatur of its 2024 framework for laboratory-developed tests, reverting the definition of in vitro diagnostics in 21 CFR 809.3 to its pre-2024 text. In practical terms, the agency stepped back from device-style oversight of LDTs. That reopened a pathway for clinical labs to bring new assays to market under CLIA without FDA premarket review, including biological age tests that stalled over the past year. See the official notice in the Federal Register LDT vacatur notice.
The policy consequence is straightforward. We are back to a CLIA era for LDTs. CLIA governs laboratory quality systems and personnel standards but not clinical claims. That means clinical labs can validate an assay’s analytical performance and begin offering it clinically if they meet CLIA and any applicable state requirements. For background on CLIA’s scope, review the CMS overview of the CLIA program.
For a primer on the certification landscape, see our internal guide to how CLIA lab certification works, and for biomarker basics, start with epigenetic clocks explained for clinicians.
Why this matters for biological age tests
Biological age testing has lived in regulatory limbo. Epigenetic clocks that read methylation patterns, proteomic panels that infer systemic wear and tear, and multi-omic models that blend DNA methylation, proteins, metabolites, and clinical data are typically LDTs. Under the now-vacated device framework, many of these assays would have needed premarket submissions, slowing iteration and access. Returning to CLIA oversight lowers the regulatory friction to launch or update these tests.
Three immediate effects follow:
- Faster iteration cycles: Labs can recalibrate models with new training data or improve pre-analytical handling without reopening an FDA submission. That is critical for epigenetic clocks where batch effects, normalization, and reference panels evolve quickly.
- Wider clinical deployment: Hospital and reference labs can add age-biomarker LDTs to menus after internal validation and proficiency testing. Expect more clinics to integrate biological age readouts into preventive cardiometabolic, oncology survivorship, and geriatric assessments.
- More variation in quality: The flip side of speed is heterogeneity. In CLIA, analytical validity is the focus. Clinical validity and utility are not pre-cleared by FDA, so claims can outrun evidence unless labs self-impose strong validation standards.
For a quick refresher on the policy history, see our overview of LDT regulation and recent shifts.
The pipelines that will accelerate
- Epigenetic clocks: Array-based methylation clocks will likely proliferate as LDTs, including versions tuned for distinct tissues, smoking exposure, cardiorenal risk, and surgical risk. Labs will compete on precision, calibration across ethnic and age strata, and responsiveness to interventions.
- Proteomic age panels: Olink, SomaScan, and mass-spectrometry platforms support multi-hundred-analyte panels. Under CLIA, labs can tune models for organ-specific aging or frailty risk and roll them out with internal validation.
- Multi-omic composites: Combining methylation, proteomics, metabolomics, and clinical markers into a single biological age score will be more feasible as an LDT. Expect composite endpoints tailored for cardiometabolic healthspan, cognitive resilience, or musculoskeletal function.
What this means for longevity trials
The biggest bottleneck in longevity therapeutics is waiting for hard outcomes. Senolytics, partial reprogramming, geroprotective combinations, and organ-specific rejuvenation strategies all need faster readouts than mortality or incident disease. A CLIA-first environment allows sponsors to:
- Use biological age as a secondary endpoint that is operational today.
- Iterate adaptive designs with interim biomarker shifts to improve sample efficiency.
- Pre-specify composite biomarker panels that capture multi-system benefit rather than one molecule at a time.
But caution is warranted. Surrogate acceptance standards do not change with CLIA. A biomarker can be analytically impeccable yet clinically unproven. To make biological age credible in trials:
- Anchor biomarkers to prospective clinical outcomes with pre-registered statistical analysis plans.
- Demonstrate within-person reliability and minimal detectable change over the study horizon.
- Show intervention specificity. If every lifestyle change moves the biomarker, it may not discriminate drug effect.
Expect more platform trials that use a battery of CLIA LDT biomarkers for enrichment and signal detection, with hard outcomes tracked longer term. With LDTs back on-ramp, teams can standardize pre-analytical handling and blinded split-sample workflows across sites, making multi-site healthspan endpoints more practical.
The new DTC risk landscape
A rollback invites a new wave of direct-to-consumer offerings that translate biological age into confident-sounding decade adjustments, body-system ages, and micro-targeted supplement plans. The risks are predictable:
- Overfitting and optimistic cross-validation inflate claims.
- Minimal transparency on sample stability, batch correction, and lab-to-lab variance.
- Misinterpretation by consumers and coaches when a single number is treated as a diagnosis or therapy monitor.
Consumers will see slick apps, instant scores, and promises of reversing years in weeks. Without device-level premarket reviews, the burden shifts to labs, clinicians, and payers to demand evidence on analytical validity, clinical validity, and clinical utility.
Validation and quality frameworks labs should follow now
Even without FDA premarket review, high-quality LDTs can meet rigorous standards. Labs should formalize the following:
Accreditation and governance
- Maintain CAP accreditation or ISO 15189 accreditation in addition to CLIA certification.
- Appoint an independent assay oversight committee with biostatistics, clinical, and laboratory medicine expertise to approve claims and monitor drift.
Analytical validation
- Precision and repeatability: Conduct multi-operator, multi-day precision studies with predefined acceptance criteria. Include replicate measures across the assay’s reportable range.
- Accuracy and trueness: Use reference materials or cross-lab comparison on well-characterized samples. For methylation assays, confirm array normalization and probe filtering pipelines with spike-ins and external controls.
- Limits and robustness: Define limit of detection and quantitation as applicable, evaluate matrix effects, and test robustness to pre-analytical variation like shipping temperature, storage time, and freeze-thaw cycles.
- Interference: Quantify hemolysis, lipemia, bilirubin interference, common medications, and inflammatory states when relevant to the biology.
Bioinformatics and model validation
- Pre-specify the feature space, normalization, and model class. Lock the pipeline before external validation.
- Use nested cross-validation during development to avoid information leakage. Reserve a true external test set sourced from different time periods and geographies.
- Report calibration, not only discrimination. Provide calibration plots and net reclassification improvement against standard risk tools.
- Establish model governance for drift monitoring with control charts on key features and outputs.
Clinical validation and utility
- Link baseline biomarker to prospective outcomes such as incident disease, functional decline, hospitalization, or mortality in observational cohorts.
- For interventional claims, run randomized or well-controlled studies that evaluate within-person change versus control and correlate biomarker shifts with clinical or functional changes.
- Publish methods and summary performance, including failure rates and proportion of samples excluded for quality reasons.
Reporting and interpretation
- Provide measurement uncertainty for the age estimate and the minimal detectable change at 95 percent confidence.
- Report domain-specific subscores only if each submodel has independent validation.
- Include a decision-use guide that maps score ranges to recommended clinical actions or to no-action zones to prevent overuse.
Payers, coding, and liability
Coverage dynamics
- Under CLIA, most biological age tests will be self-pay until there is evidence of clinical utility tied to outcomes or cost offsets. Medicare Administrative Contractors may evaluate coverage via molecular diagnostics policies. Private payers will look for published prospective validation, change management protocols, and real-world utility.
- Expect labs to pursue PLA CPT codes for distinct panels. Coverage will likely track indications, for example perioperative risk stratification rather than general wellness.
Liability shifts
- With the device-rule rescinded, classic medical malpractice, negligence, and consumer protection frameworks loom larger for LDTs. If a test is marketed with disease claims without adequate validation, plaintiffs will not face device preemption hurdles.
- Clear labeling, conservative claims, and documented clinician education reduce risk. Software pipeline change control and audit trails are essential for defensibility.
Contracting and data
- Health systems adopting these tests should require data rights for outcomes tracking and insist on performance guarantees tied to analytical failure rates and turnaround time.
State-by-state realities to watch
Federal CLIA sets the floor, but states can go further.
- New York: The Clinical Laboratory Evaluation Program requires test-specific review or recognition pathways for many LDTs before they can be offered on New York specimens, with explicit risk tiering and approvals. Labs that plan to serve New York patients should budget time and evidence for this process.
- Washington: Operates a CLIA-exempt Medical Test Site program. Laboratories testing in-state must meet state licensure standards that are at least as stringent as CLIA.
- Direct access testing limits: Several states restrict direct access testing or require physician orders for most lab testing. Companies planning nationwide DTC offerings will need a physician network and state-by-state compliance program.
CLIA is the floor, not the ceiling
CLIA focuses on laboratory quality, personnel qualifications, proficiency testing, and process control. It does not preclear clinical claims about disease risk reduction or therapeutic monitoring. As LDT oversight returns to this regime, labs and clinics should center the CLIA program in their compliance stack and then layer on additional quality controls. For authoritative program scope and requirements, consult the CMS overview of the CLIA program.
A practical checklist for clinicians
Use this to triage which biological age tests deserve space in your clinic:
- Regulatory and accreditation
- Is the lab CLIA certified, CAP or ISO 15189 accredited, and in good standing with any state licensure programs it claims to operate under?
- If the clinic serves New York patients, does the test have NYS approval or a documented pathway that permits use for those specimens?
- Analytical transparency
- Do you see a validation summary with precision, bias, reportable range, sample stability, and failure rates? Are pre-analytical requirements clear and practical for your workflow?
- Model performance
- Are external validation datasets described with demographics, sample handling, and timeframes? Are calibration plots available, not just correlations?
- Is minimal detectable change reported so you can interpret follow-up tests?
- Clinical evidence and use case
- Is there evidence linking the score to outcomes you care about for your patients? Are there decision thresholds tied to actions or is the output purely informational?
- Interoperability and support
- Can results flow into your EHR discretely? Does the lab provide clinician guides and patient-friendly reports that avoid therapeutic overreach?
- Contracting and risk
- Does the agreement include performance SLAs and a process to notify you of pipeline updates? Is there a recall or reanalysis plan if a software defect is found?
A practical checklist for consumers
If you are considering a biological age test, look for:
- Lab quality: CLIA certification and reputable accreditation. Beware of pop-up labs without a clear facility address and director.
- Plain-language validation: A one-page summary should show how consistent the test is on the same person over time and how results relate to real health outcomes.
- Conservative claims: Look for careful language. If a company promises to reverse your age in weeks or to treat disease, walk away.
- Reporting clarity: Good reports show uncertainty bands and explain what a reasonable change looks like between tests.
- Data practices: Your consent should state how your data is used, whether it is sold or shared, and how to delete it. Prefer vendors that let you download raw data.
- Physician involvement: For tests that could influence medical decisions, make sure a licensed clinician is involved and reachable for questions.
What to expect next
- Rapid relaunches: Expect several labs to reintroduce paused assays and to announce new panels optimized for specific populations.
- Quiet standard-setting: Professional societies, payers, and large health systems will converge on practical validation thresholds. The first covered use cases will likely be risk stratification where biomarkers add value on top of existing scores.
- Real-world evidence networks: To convince payers, labs will partner with systems to track outcomes linked to biomarker-guided decisions. Transparency will be a competitive advantage.
Bottom line
FDA’s September 19, 2025 implementation of the LDT vacatur returns biological age tests to a CLIA-first world. That will accelerate innovation and access, but it also shifts responsibility for evidence and restraint onto labs, clinicians, and payers. The winners in this next phase will not simply market the most optimistic biological age scores. They will show their work, quantify uncertainty, connect biomarker change to meaningful outcomes, and protect patients from overreach. If we get that right, these tools can become reliable instruments for healthspan research and clinical decision making rather than glossy dashboards for curiosity.