Lp(a) goes mainstream: RNA shots reset lifelong heart risk
In March 2025, lepodisiran delivered striking and durable Lp(a) reductions, while pelacarsen’s first outcomes readout is guided for 2026. Here is why Lp(a) is causal, why lifestyle will not fix it, and how rare dosing could reshape midlife heart risk.
The moment Lp(a) went mainstream
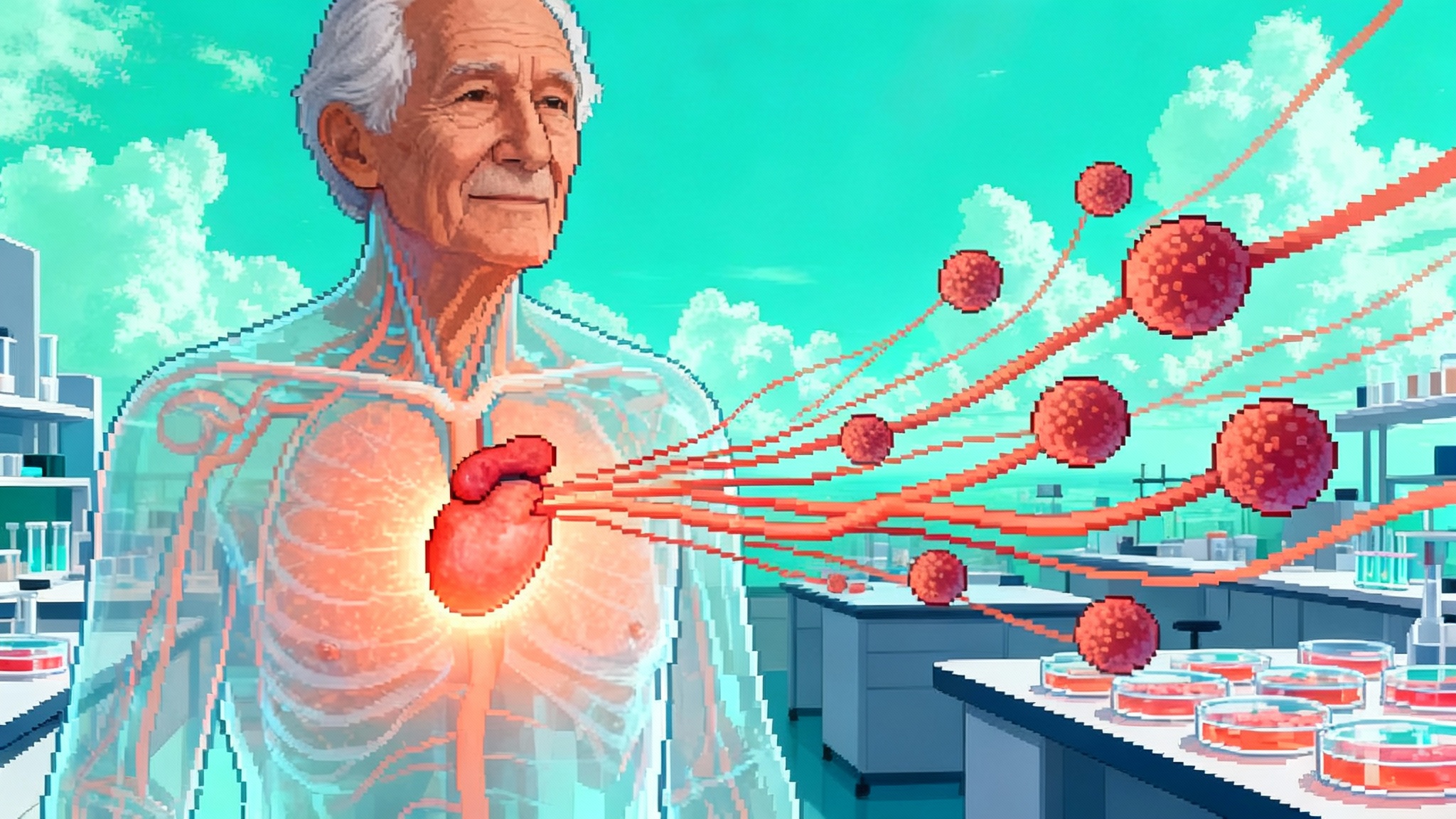
On March 30, 2025, a quietly persistent heart risk factor stepped into the spotlight. At ACC.25 and in the New England Journal of Medicine, investigators reported that lepodisiran, an investigational siRNA that turns down liver production of apolipoprotein(a), reduced lipoprotein(a) by roughly 94 percent at its highest tested dose, with suppression that lasted many months after a single injection. The magnitude and durability were unlike anything seen before for this target, and they were achieved with infrequent dosing. It was the first time many clinicians realized that a lifelong genetic driver of atherosclerosis might soon be modifiable with a schedule closer to vaccines than daily pills, as summarized in the NEJM lepodisiran trial results.
That splash matters because Lp(a) has long been the risk factor patients discover only after their first heart attack. Unlike LDL cholesterol, which we can diet, exercise, and medicate down, Lp(a) is largely set by your genes at birth and barely budges across a lifetime. Until RNA medicines arrived, there was no specific, effective therapy.
Why Lp(a) is not just another cholesterol number
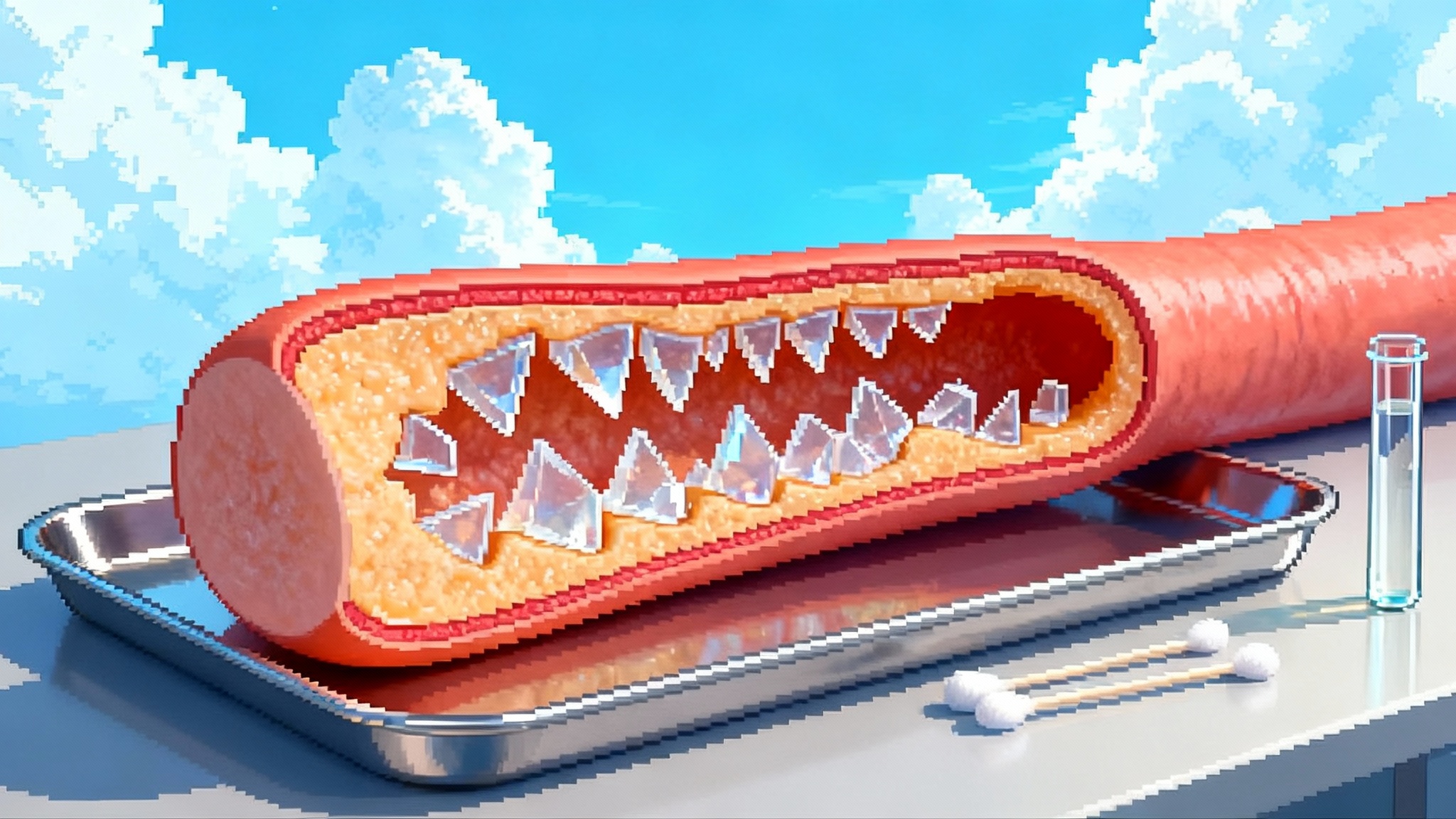
Lp(a) is an LDL-like particle with an extra apolipoprotein called apo(a) attached to apoB. That add-on changes biology in three crucial ways:
- It raises atherogenic burden. Lp(a) is a cholesterol-rich particle that contributes to the plaque that narrows arteries.
- It is proinflammatory in the vessel wall. Oxidized phospholipids carried on Lp(a) amplify plaque inflammation.
- It is prothrombotic. Structural homology between apo(a) and plasminogen may promote clot formation at the worst possible time.
Population genetics, Mendelian randomization, and prospective cohorts converge on the same message. Elevated Lp(a) is a causal, inherited driver of atherosclerotic cardiovascular disease. It increases risk of myocardial infarction, ischemic stroke, and calcific aortic valve stenosis. Levels are highly heritable and stable, and standard lifestyle tools do not lower it. Statins, while lifesaving for LDL, generally do not reduce Lp(a); PCSK9 inhibitors trim it modestly; niacin can lower Lp(a) but failed to improve outcomes when added to statins in modern trials. For people with high Lp(a), even perfect LDL control may leave a sizable residual risk. For broader context on apoB lowering and future one-time approaches, see the internal overview of the PCSK9 base editing roadmap.
From numbers to outcomes: pelacarsen’s pivotal moment
The field now awaits the first large cardiovascular outcomes trial that asks the only question that matters for patients: does specifically lowering Lp(a) prevent heart attacks and strokes. That trial is Lp(a)HORIZON, testing pelacarsen, a monthly antisense oligonucleotide that blocks apo(a) synthesis. Novartis, which is running the event-driven study in more than 8,000 patients with established cardiovascular disease and high Lp(a), has guided investors that the readout shifted into 2026 due to blinded event accrual, as noted in the Novartis 2024 results transcript.
If pelacarsen demonstrates a clinically meaningful reduction in major adverse cardiovascular events, it will validate Lp(a) as a modifiable risk factor and set a benchmark for the rest of the class. It would also inform what degree of Lp(a) suppression translates into risk reduction, and in which patients the benefit is greatest.
How RNA therapies work here, and why dosing cadence is the twist
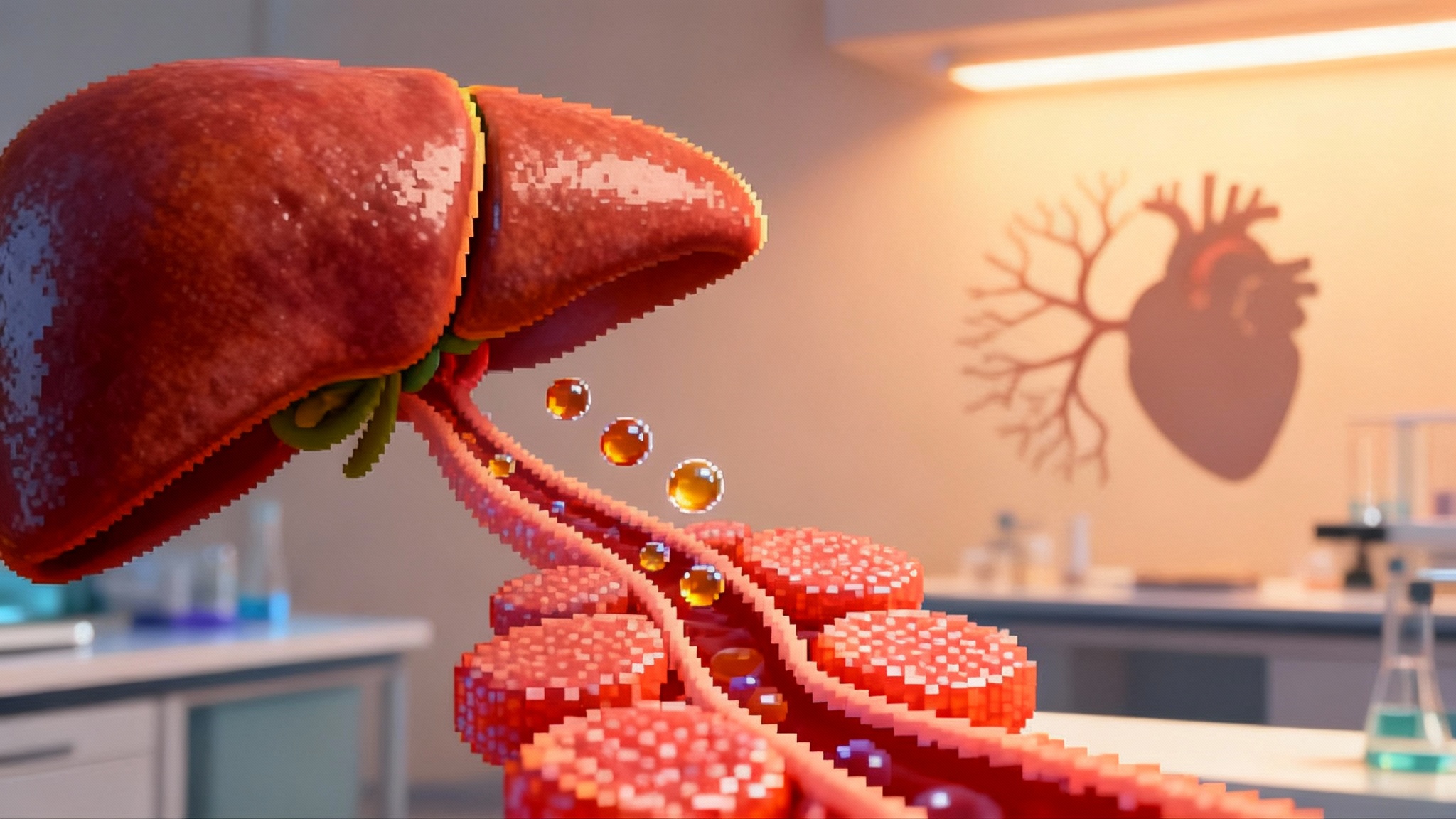
siRNA and antisense medicines both target the message, not the protein. They direct the liver to destroy the mRNA template for apo(a), so fewer Lp(a) particles are assembled.
- siRNA agents like lepodisiran or olpasiran load into the RISC complex and repeatedly guide it to cleave LPA mRNA. The result is long on-target action even after the drug has cleared, enabling quarterly, twice-yearly, or possibly even annual dosing.
- Antisense oligonucleotides like pelacarsen bind their specific mRNA and recruit RNase H to degrade it. With the latest conjugation chemistries, monthly dosing has delivered large reductions.
The cadence is not a trivial convenience. Infrequent injections change adherence math. Instead of wrestling with a daily pill for decades, many people may be able to sustain profound Lp(a) suppression with a few visits a year. That is how a genetic risk starts to feel modifiable at the scale of a lifetime.
Lp(a) is not LDL: different target, different playbook
It is tempting to treat Lp(a) as another LDL. That would be a mistake.
- Causality is genetic. LDL is a mix of diet, metabolism, and genes, which makes it responsive to lifestyle and multiple drug classes. Lp(a) is almost entirely inherited and stable, so lifestyle interventions that work for LDL do not lower Lp(a) meaningfully.
- Biology is two-pronged. LDL drives plaque. Lp(a) likely adds both extra plaque burden and a prothrombotic spark. That duality may influence how quickly risk falls once we suppress it.
- Measurement differs. Labs report Lp(a) in nmol/L or mg/dL. There is no fixed conversion because apo(a) isoform size varies. In practice, 125 nmol/L approximates 50 mg/dL, which many labs and societies flag as elevated. Know which units your lab uses, and avoid casually converting values across units.
For a systems view of nontraditional contributors to vascular aging, see the discussion of microplastics and vascular aging.
What screening should look like now
Screening for Lp(a) is simple and does not require fasting. A single blood test is informative for life, barring major liver disease.
Who should test today:
- Adults with a personal history of premature atherosclerotic cardiovascular disease.
- Anyone with a first-degree relative who had early heart attack, stroke, or known high Lp(a).
- People with calcific aortic valve disease, particularly if premature or unexplained.
- Individuals with high LDL despite adherence, or with unexplained progression despite well-controlled LDL.
- Many experts now endorse once-in-a-lifetime testing for all adults, with earlier testing in high-risk families. For the evolving diagnostics landscape, review the internal guide to the FDA LDT rollback and biomarkers.
How to interpret results:
- Labs typically flag elevated Lp(a) at 125 to 150 nmol/L, roughly 50 mg/dL. Above that threshold, risk rises with level, especially in the very high range.
- Use absolute numbers in the same units over time. Do not chase tiny within-person fluctuations; day-to-day variation is small compared with differences between people.
What to do now if elevated:
- Intensify proven risk reducers. Lower apoB and LDL aggressively, control blood pressure, treat diabetes, stop smoking, and pursue physical activity. These steps do not lower Lp(a) yet they blunt overall risk and stabilize plaques.
- Consider PCSK9 inhibitor therapy in very high-risk patients, which can lower Lp(a) modestly while driving LDL to very low levels.
- Document the family pattern. Siblings and adult children should be offered testing so you can risk-stratify the whole family.
Expected benefit timelines once Lp(a) lowering arrives
How fast will events fall when we finally suppress Lp(a) at scale. The honest answer is that outcomes trials will tell us. There are plausible mechanisms for both early and late benefits:
- Early benefit could come from reducing the prothrombotic and inflammatory milieu around vulnerable plaques. If fewer clots form on top of less inflamed plaques, nonfatal myocardial infarction and urgent revascularization could fall within months.
- Late structural benefit may take years, as reduced atherogenic burden slows plaque growth. Effects on calcific aortic valve disease, which appears tied to Lp(a), may require even longer horizons.
Magnitude will hinge on baseline risk and absolute Lp(a) lowering. Patients with established ASCVD and very high Lp(a) are most likely to benefit in absolute terms. For primary prevention in midlife, the gain is more about shifting the area under the risk curve. If you can start at 40 to 55 and keep Lp(a) low for decades with two or fewer injections a year, modeling suggests a meaningful reduction in lifetime heart attack and stroke risk, even if yearly absolute risk is modest.
Safety, access, and the practical unknowns
The early safety picture for Lp(a) RNA drugs has been encouraging. Across programs, the most common adverse events are mild, transient injection site reactions. Class effects to watch include liver enzyme elevations and, for some antisense chemistries historically, thrombocytopenia, though pelacarsen’s program has not shown a clear platelet signal to date. It will be essential to see long-term safety from outcomes trials and extension studies that follow people for years.
Key access questions on the horizon:
- Who qualifies. Regulators will decide initial labels based on outcomes data. Early use will likely focus on secondary prevention in patients with established ASCVD and high Lp(a). Thresholds such as 125 nmol/L or higher are plausible starting points, potentially with higher cutoffs for primary prevention.
- How often to dose. siRNA agents may support twice-yearly or even annual dosing, while antisense therapies may be monthly. Real-world adherence and patient preference will shape choices.
- Cost and coverage. These are advanced biologics, so list prices may be substantial. Payers will likely require documented elevation and guideline-directed LDL control, at least initially. Over time, competition across modalities could bring more options and tiered pricing.
- Health equity. Black patients have a higher prevalence of elevated Lp(a). Ensuring equitable testing and access must be part of any rollout, from primary care awareness to payer policies that do not create barriers in the communities with the highest burden.
How this differs from the LDL playbook in the clinic
Expect Lp(a) therapy to be additive, not a replacement. Optimizing LDL remains foundational because LDL lowering prevents events across the board. The practical clinic flow may look like this:
- Test Lp(a) at least once in adulthood, earlier if family history is strong. Record the value and units.
- If elevated, double down on LDL and apoB lowering with statins, ezetimibe, and PCSK9 inhibitors as needed. Manage blood pressure, diabetes, weight, sleep apnea, and lifestyle.
- Reassess global risk. Coronary calcium scoring can help clarify near-term risk in primary prevention.
- Discuss Lp(a)-targeted therapy once approved and available, prioritizing those with established ASCVD or strong family histories and very high levels.
- Choose the regimen that fits the patient. For some, monthly antisense may be fine. For others, a twice-yearly siRNA injection could be far easier to sustain.
- Monitor with Lp(a) measurements in the same units, plus standard safety labs, at reasonable intervals. Expect large percentage reductions; the clinical question is how that maps to fewer events.
The broader longevity upside if Lp(a) suppression becomes routine
Cardiovascular aging is partly about the burden of atherosclerosis you carry into your 60s, 70s, and beyond. If you have elevated Lp(a), you accumulate risk faster for the same LDL and blood pressure. The promise of these RNA therapies is not only fewer events next year. It is a gentler slope of cumulative vascular damage for decades.
Imagine a midlife care model where everyone knows their Lp(a) by 40 to 55. Those with high levels keep LDL very low, address lifestyle comprehensively, and start Lp(a) suppression with injections as infrequent as twice a year. Over a lifetime that combination could mean fewer heart attacks, fewer strokes, and possibly a slower march toward valve replacements. Even if the first labels focus on secondary prevention, the long-term public health impact will depend on how we operationalize screening and how far into primary prevention regulators, payers, and patients decide to go once outcomes evidence matures.
What to watch through 2026
- Outcomes data for pelacarsen. Event-driven trials answer the only question that counts for approval and guidelines. The size of risk reduction and which subgroups benefit most will guide practice.
- Dosing cadence and durability. Longer intervals with sustained suppression will favor adherence and scale. Lepodisiran’s early durability signal raises the bar for convenience.
- Primary prevention signals. Trials in secondary prevention will lead. Over time, observational data and dedicated studies will inform the benefits and boundaries of treating high Lp(a) in asymptomatic midlife adults.
- Health system readiness. Lab order sets, EHR prompts, and payer criteria will determine whether once-in-a-lifetime testing and targeted therapy reach the people who need them most.
Bottom line
The science has caught up to a stubborn gene. March 2025 was the inflection point when a once-untreatable risk became convincingly druggable, and with a cadence that fits real life. Lp(a) is not LDL and will require a different strategy, but the destination is familiar. If outcomes trials confirm that big, durable reductions translate into fewer heart attacks and strokes, suppressing Lp(a) could become as routine in midlife care as statins are today, with a compounding payoff in healthier decades ahead.