Tiny plastics, aging arteries, and your heart risk
New data from 2024 and spring 2025 detect micro and nanoplastics inside human carotid plaques and link them to higher rates of heart attack and stroke. Learn what this means for vascular aging and the practical steps you can take to reduce exposure today.
The new signal inside our arteries
In April 2025, scientists presented early but striking evidence that carotid artery plaques can harbor a dense load of tiny plastics. In preliminary data highlighted at AHA’s Vascular Discovery meeting, plaques from the neck contained far more micronanoplastics than arteries without plaque, and the highest burdens were seen in people who had stroke or mini stroke symptoms. These signals add a human, vascular context to a problem we have mostly framed as environmental. See the research summary in the AHA Vascular Discovery 2025 findings.
This is not happening in isolation. In 2024, a prospective human cohort linked plastic fragments lodged within endarterectomy plaques to real outcomes, not just lab markers. Patients whose plaques contained micro and nanoplastics experienced more heart attacks, strokes, or death over roughly three years compared with those whose plaques were free of these particles, even after accounting for traditional risk factors. The study used strict contamination controls and multiple analytical methods to confirm particle identity. For prevention, this is the kind of evidence that moves a topic from concern to priority. For details on methods and risk estimates, see the peer reviewed NEJM carotid plaque cohort.
A fast primer on what was found
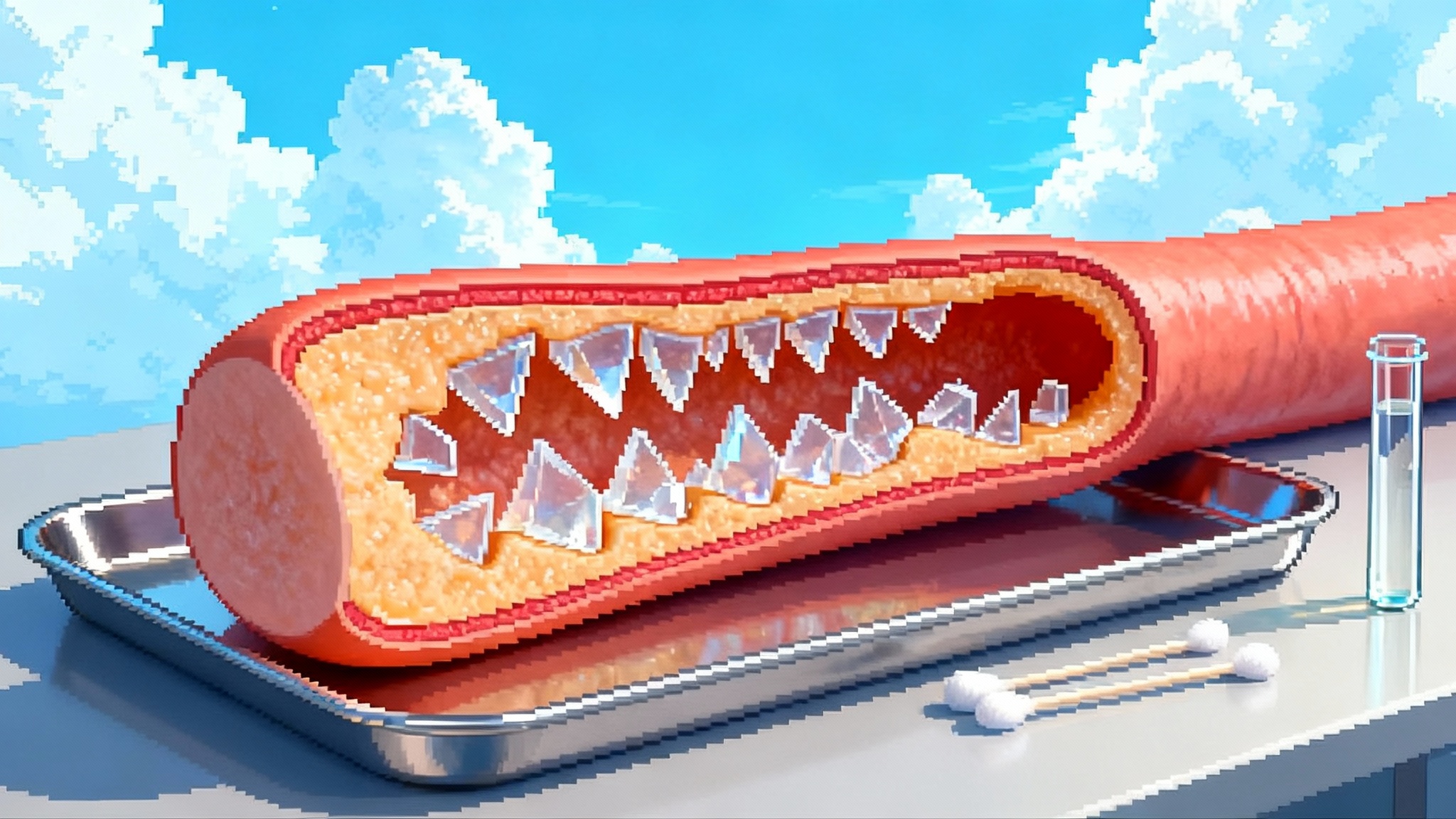
- Where the particles sit: In both the 2024 outcomes study and the 2025 conference data, plastic fragments were detected within the atherosclerotic plaque itself, including inside macrophages and in the extracellular matrix. Imaging showed irregular, shard like particles that look nothing like smooth biological debris.
- What types of plastics: Polyethylene was common, and some plaques also contained polyvinyl chloride. These are ordinary ingredients in packaging, pipes, and many consumer products. Their presence in plaque suggests sustained systemic exposure.
- Why this matters: When a foreign body is embedded in inflamed tissue that already struggles to heal, the stage is set for chronic irritation, immune activation, and potentially more brittle plaque biology.
How environmental plastics could accelerate vascular aging
Vascular aging is not just about time. It is about the sum of injuries and repairs that endothelium, smooth muscle, and immune cells perform across decades. Tiny plastics add several plausible hits to that cycle.
- Endothelial stress and nitric oxide loss
- Physical irritation: Jagged micro and nanoplastics can abrade or press on the endothelial glycocalyx, the sugar rich protective layer that coats blood vessels. Microlesions promote platelet adhesion and create entry points for lipoproteins.
- Oxidative imbalance: In vitro work shows that microplastics can increase reactive oxygen species and reduce nitric oxide bioavailability. Less nitric oxide means stiffer arteries, more vasoconstriction, and greater leukocyte adhesion. Chronic stiffness and endothelial activation are hallmarks of vascular aging.
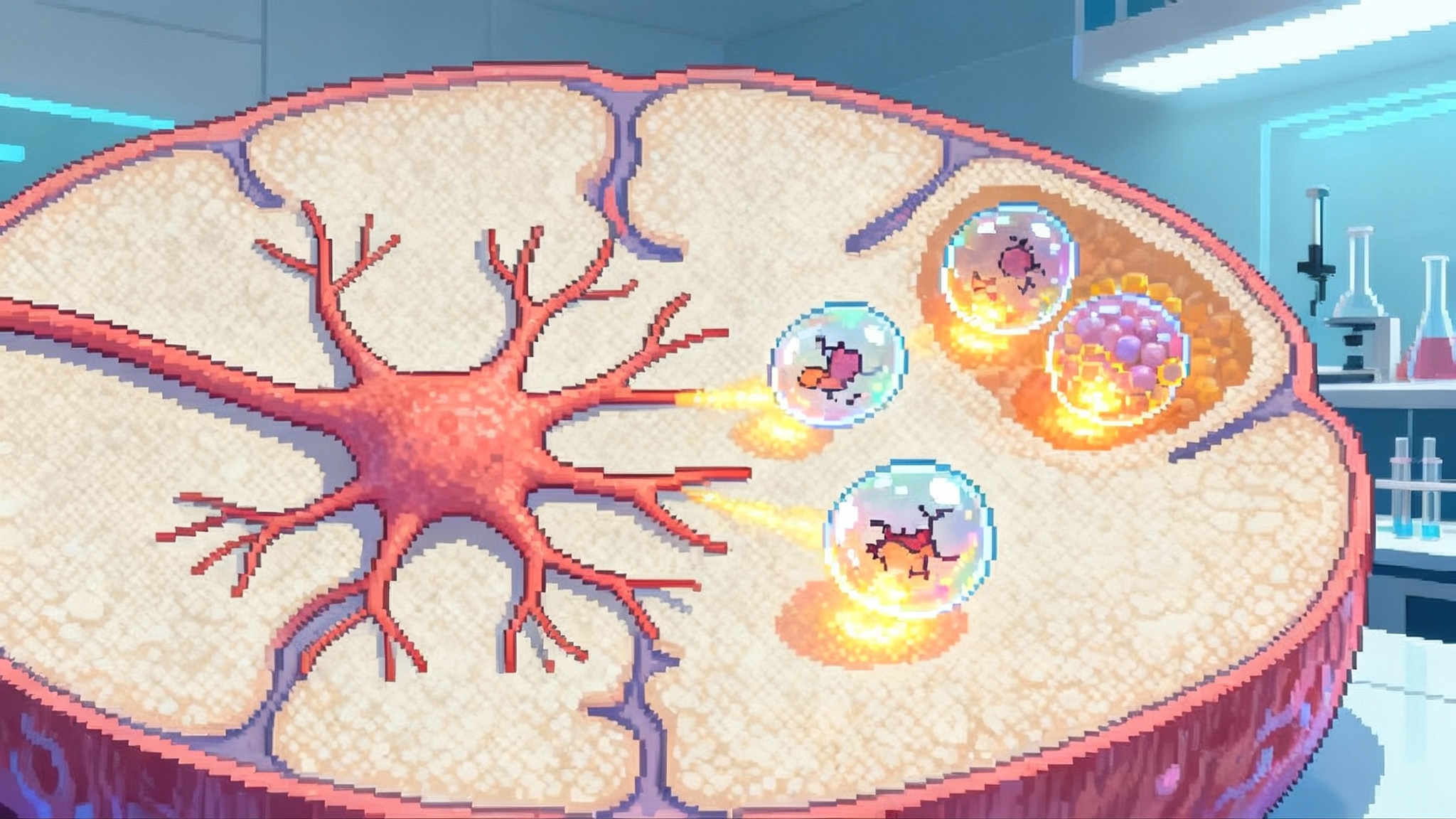
- Persistent inflammation inside plaques
- Inflammasome activation: Plastics and their surface chemistries may trigger pattern recognition receptors and prime the NLRP3 inflammasome, driving IL 1 family signaling. These cytokines amplify local inflammation and can destabilize plaques.
- Macrophage burden: Macrophages that engulf nondegradable particles shift toward a proinflammatory state and often fail to clear apoptotic cells efficiently. Impaired efferocytosis enlarges the necrotic core and weakens the fibrous cap.
- Immune remodeling that skews healing
- Trained immunity: Repeated exposure to persistent particles can epigenetically reprogram myeloid cells, leaving them quick to inflame and slow to resolve. That bias can outlast the original insult and may accelerate atherosclerosis.
- T cell crosstalk: Dendritic cells exposed to particle stress favor costimulatory signals that recruit T helper 1 and T helper 17 responses within plaques, further pushing a proinflammatory loop.
- Additive chemical stress carried on the particles
- Additives and adsorbates: Many plastics carry additives like plasticizers or heat stabilizers. Their surfaces can also adsorb polycyclic aromatic hydrocarbons and metals. In the bloodstream or plaque, that cargo can leach and amplify oxidative and endocrine stress.
- Smooth muscle cell switching
- Phenotypic drift: Vascular smooth muscle cells exposed to oxidative and inflammatory signals switch from a contractile to a synthetic state. Synthetic cells make collagen poorly and contribute to microcalcification, both of which can destabilize plaques over time.
No single mechanism proves causality. Together, they outline how chronic exposure could push arteries toward an older, more injury prone state, especially in people with existing risk factors. For a broader look at inflammation targeted strategies, see how senolytics move to the clinic.
Measuring what we cannot see
Detecting plastic at the micro to nano scale inside human tissue is hard. The strongest studies use layered methods to minimize false positives and background contamination.
- Thermal chemistry: Pyrolysis gas chromatography mass spectrometry converts polymer fragments into identifiable chemical fingerprints. It quantifies total polymer mass but not particle shape.
- Stable isotope and elemental analysis: Chlorine or other elemental signatures can help confirm polymer types like PVC and distinguish them from lookalike biological debris.
- Imaging: Scanning or transmission electron microscopy reveals particle morphology and location relative to cells. Energy dispersive X ray analysis can show elemental components.
- Vibrational spectroscopy: Raman and Fourier transform infrared spectroscopy identify polymer types by their spectral fingerprints and are already part of standardized protocols for water testing.
- Contamination controls: Clean room adjacent workflows, cotton lab coats, filtered air benches, and procedural blanks are essential to prevent airborne fibers from confounding results. Tissue blanks and replicate runs help prove the signal is real.
As labs converge on methods, expect regulatory shifts that affect test availability and validation, including the FDA LDT rollback and biomarkers.
Who is most exposed today
Exposure is not evenly distributed. Patterns emerge across lifestyle, location, and work.
- Urban traffic corridors: Tire and road wear generate rubbery microplastics that load the air near busy roads. Commuters, cyclists, and residents in these areas inhale more particulate debris.
- Indoor environments: Indoor air often contains higher microfiber concentrations than outdoor air. Carpets, synthetic upholstery, and fleece clothing shed fibers that settle in dust and resuspend with movement.
- Food and drink contact with plastic: Hot liquids and prolonged contact increase microplastic shedding. Convenience foods and single use packaging increase opportunities for transfer.
- Bottled beverage reliance: People who drink mostly bottled water or soft drinks likely ingest more particles than those who use well maintained filtered tap water.
- Occupational exposure: Workers in plastics manufacturing, recycling, textiles, 3D printing, and tire production face higher airborne loads without robust controls.
- Coastal and arid regions: Sea spray and windblown dust can carry microplastics inland. Drought driven dust events may increase exposure in some areas.
- Social determinants: Lower income neighborhoods often sit closer to high traffic roads or waste sites and may have less access to effective filtration or fresh unpackaged foods.
Practical steps to lower your personal burden
These actions target where most exposure happens: water, air, and hot food contact with plastics. None of them claim to eliminate risk, but together they likely dial exposure down.
Water
- Prefer tap water run through a certified point of use system that combines activated carbon and a reverse osmosis membrane. RO removes a wide range of particle sizes, and carbon polishes taste and captures some organics.
- If RO is not feasible, choose high quality carbon block filters with small nominal pore sizes and replace cartridges on schedule. Pair with a sediment prefilter to maintain flow and prevent channeling.
- Store water in glass or stainless steel. Avoid long hot storage in plastic bottles.
Air and dust
- Use a portable HEPA purifier in bedrooms and living areas sized for the room. Central HVAC should use MERV 13 or higher filters if the system can handle the pressure drop. Change filters on schedule.
- Vacuum with a sealed HEPA vacuum. Wet mop or use microfiber cloths that you wash in full, cold loads to reduce shedding.
- Ventilate when cooking and limit processes that sharply increase indoor particulates, such as frequent oven self cleaning cycles.
Kitchen contact and food choices
- Do not microwave plastic containers or cling film. Reheat in glass or ceramic. Use silicone sparingly for high heat and replace at signs of wear.
- Favor loose produce and bulk dry goods in reusable containers over heavily packaged options. Cut down on single use cups and utensils for hot beverages and meals.
- Prefer paper or metal mesh filters for hot drinks rather than plastic containing pods or bags when feasible.
Laundry and clothing
- Wash synthetic garments less often, on cold, in full loads to reduce fiber shedding. Air dry when possible.
- Install a washing machine filter designed to capture microfibers or use a capture bag to intercept lint before it reaches wastewater.
- When buying new clothes, consider natural fibers or tight knit synthetics that shed less.
Home and habits
- Choose cellulose or natural fiber sponges and cloths over plastic heavy scrubbers. Replace them before they crumble.
- Open windows when outdoor air is clean and traffic is low. Close them during rush hour or dust events.
Healthcare alignment
- These steps pair well with standard cardiovascular prevention. Keep doing the basics that have the strongest outcome data: blood pressure control, LDL lowering, exercise, sleep, and smoking cessation. For cardiometabolic risk reduction at scale, see GLP 1s at scale. Environmental load reduction is not a substitute for proven therapies.
Policy momentum that matters
The policy landscape is beginning to catch up.
- Europe: The European Union’s restriction on intentionally added microplastics under REACH began applying in October 2023, with phase ins and guidance updated in 2025. It will not erase legacy plastics, but it should reduce new releases over time and drive product reformulation.
- United States: There is no federal drinking water standard for microplastics yet. California has moved ahead with a state definition, test methods, and a multi year monitoring program for drinking water. That program has spurred method development and lab accreditation and should generate public reports to inform utilities and consumers.
- Health societies: Microplastics are now showing up at cardiology and vascular meetings, signaling movement from environmental health circles into mainstream prevention. As replication builds, expect professional statements on measurement, exposure reduction, and clinical communication.
Large institutions can act quickly. Hospitals, schools, and municipalities can shift purchasing toward lower shedding textiles, avoid unnecessary single use plastics in food service, and specify high efficiency filtration in HVAC retrofits.
From association to action: what to watch next
- Replication cohorts with outcomes: Additional prospective studies in diverse populations undergoing carotid or coronary procedures that analyze plaques for micro and nanoplastics and track events. Look for standardized contamination controls, blinded adjudication, and dose response analyses.
- Interventional trials that measure risk markers: Randomized household trials comparing multi stage water filtration and HEPA air cleaning against usual care, with endpoints like flow mediated dilation, arterial stiffness, inflammatory cytokines, and microplastic counts in stool or blood.
- Surgical tissue biobanks: Multicenter efforts to archive plaque samples with detailed exposure histories and parallel blood and stool samples. Linking tissue burden to plaque morphology and gene expression will clarify mechanisms.
- Nanoplastic analytics: Validation of rapid assays that can quantify nanoplastics in biological fluids with high sensitivity and specificity. Portable or high throughput methods will make population studies feasible.
- Occupational cohorts: Longitudinal studies in plastics, textiles, tire, and recycling workers with personal air monitoring, biomarkers of exposure, and cardiovascular imaging.
- Pediatric and prenatal windows: Studies of placental tissue and early life exposures related to vascular function could reveal sensitive windows where exposure reduction has outsized payoffs.
- Policy triggers: State or federal inclusion of microplastics in standard drinking water monitoring cycles, plus procurement standards for low shedding textiles and food packaging in public institutions.
Bottom line
Two things can be true at once. The causal chain from tiny plastics to clinical events in humans is not proven end to end. At the same time, the newest human data show plastic fragments embedded in plaques and an association with higher cardiovascular events. For a disease defined by decades of small injuries, it is reasonable to treat avoidable environmental stress as one more modifiable exposure. Cut the load where you can, keep doing the prevention basics, and watch for the next studies that will tell us how far exposure reduction can move vascular risk.