Autophagy, Alzheimer’s, and the Fast Track to Longevity
Retro Biosciences plans a first-in-human study of RTR242, an autophagy-enhancing pill for Alzheimer’s. Learn why a disease label can accelerate longevity drugs, the biomarker stack to watch through 2026, and how this brain-first strategy compares with partial epigenetic reprogramming.
A brain-first pivot for longevity
Silicon Valley’s longevity push is moving from petri dishes to patients. Retro Biosciences plans to start a first-in-human study in Australia of RTR242, a small molecule designed to revive autophagy and treat Alzheimer’s disease. If successful, this could become a template for hallmarks-first drug development. Retro expects dosing to begin by late 2025, making this first-in-human RTR242 trial a bellwether for brain-first longevity.
Why a disease label can be the shortest path to healthspan
Longevity therapeutics face a fundamental constraint. Regulators approve medicines for specific diseases with validated endpoints, not for aging as a single condition. That makes disease-first footholds essential.
Alzheimer’s is a compelling starting point because:
- The disease burden is large and rising, which concentrates trial sites, patient registries, and payer focus.
- Biomarker infrastructure is mature. Assays for amyloid, tau, neurofilament light, and advanced imaging allow early signals of target engagement and disease modification.
- Regulators now accept mechanistic strategies beyond symptomatic relief, which opens the door for disease-modifying approaches tied to core aging biology.
Starting with Alzheimer’s can also shorten time to a readout. Prevention trials in healthy older adults are slow and expensive. Early Alzheimer’s programs can produce safety and biomarker signals within 12 to 24 months.
Autophagy 101: the proteostasis reset switch
Autophagy is the cell’s housekeeping system, responsible for identifying damaged proteins and organelles, sequestering them in autophagosomes, and recycling them via lysosomes. Major modes include macroautophagy, microautophagy, and chaperone-mediated autophagy. Together with the ubiquitin proteasome system and molecular chaperones, autophagy maintains proteostasis across tissues. For a broader primer, see our cellular cleanup primer and hallmarks of aging explainer.
In brain aging and Alzheimer’s, autophagy flux declines. Misfolded proteins accumulate, lysosomes clog, and neurons lose clearance capacity. Both amyloid beta and pathological tau interact with the autophagy lysosome system, either overwhelming it or derailing it. Pharmacologic restoration aims to restart full flux, not just increase autophagosome counts. In neurons, successful flux could improve clearance of toxic species, stabilize synapses, and reduce neuroinflammation.
The regulatory strategy: shoot for Alzheimer’s, build toward healthspan
A pragmatic path for an autophagy enhancer:
- Prove safety and pharmacokinetics in humans.
- Show target engagement with peripheral and central biomarkers that report autophagy flux and downstream proteostasis.
- Demonstrate Alzheimer’s biology moving in a favorable direction.
- Deliver early cognitive and functional signals that match the biomarker story.
If those steps align, expansion into other organs becomes more credible.
What to measure: the biomarker stack that matters
Alzheimer’s trials now use an extensive toolbox. The most convincing package integrates target engagement, disease biology, and clinical function. For more detail, see our guide to Alzheimer’s biomarkers.
-
Central Alzheimer’s biology
- CSF Aβ42 and Aβ42 to Aβ40 ratio, interpreted by disease stage and alongside other markers.
- CSF phosphorylated tau species, especially p-tau217 or p-tau181, with sustained declines indicating reduced tau activity.
- CSF total tau as a general neurodegeneration readout.
- Amyloid and tau PET for mechanistic differentiation, used selectively due to cost.
-
Neuronal injury and neurodegeneration
- Plasma or CSF neurofilament light, where reductions suggest less axonal injury.
- Plasma GFAP for astroglial activation, particularly in early disease.
-
Cognitive and functional outcomes
- Sensitive composites such as PACC, iADRS, or ADAS-Cog 13 for early symptomatic disease.
- CDR Sum of Boxes and activities of daily living scales for functional meaning.
- Digital assessments and passive monitoring to increase sensitivity to change.
-
Peripheral autophagy target engagement
- LC3 lipidation states in PBMCs, ideally with ex vivo flux assays using lysosomal inhibitors.
- p62 or SQSTM1 levels, interpreted within a flux framework.
- Upstream phosphorylation signatures, such as ULK1 activation, to distinguish direct autophagy effects from general nutrient sensing.
- Lysosomal function markers, including cathepsin activity and CLEAR network gene activation.
- Proteostasis stress tests in PBMCs or participant-derived induced neurons pre and post dosing.
A persuasive package links autophagy engagement in blood, favorable shifts in CSF tau and neurodegeneration markers, and consistent improvements on a cognitive composite.
Safety first: autophagy is powerful biology
Because autophagy intersects many systems, safety monitoring should be broad:
- Immune balance, including infection susceptibility and vaccine response.
- Metabolism, given crosstalk with nutrient sensing pathways.
- Neuronal homeostasis, avoiding excessive activation that could harm neurons.
- Drug interactions, especially with agents that influence lysosomes or translation.
A clean Phase 1 profile and dose-proportional pharmacokinetics would set the stage for biomarker-heavy Phase 1b to Phase 2 designs.
Why start with the brain
- Biomarkers and diagnostics are advanced, enabling biologically defined enrollment and mechanistic tracking.
- Clinical need is acute, so even modest benefits matter.
- Payers already reimburse high-complexity diagnostics and specialty therapies in this category, which creates a clearer path for novel mechanisms with supportive data.
How it compares to partial epigenetic reprogramming
Partial epigenetic reprogramming seeks to reset gene expression toward a youthful state via transient expression of a subset of Yamanaka factors. Companies in this space are moving into targeted tissues. Life Biosciences reports nonhuman primate data in ocular models and says its lead program is on track to enter human trials in 2026.
Comparison highlights:
-
Modality
- Autophagy small molecules: oral, titratable, reversible exposure, straightforward manufacturing.
- Reprogramming gene therapies: durable expression, higher safety bar due to potential off-target effects and long tissue residency.
-
Mechanism scope
- Autophagy: proteostasis and organelle quality control with potential cross-tissue benefits where toxic protein accumulation drives disease.
- Reprogramming: broader gene program reset with potentially larger effects, balanced against complexity and dedifferentiation risk.
-
Regulatory path
- Autophagy in Alzheimer’s: can leverage accepted biomarker frameworks and cognitive endpoints.
- Reprogramming: likely to begin in localized indications where delivery is confined and safety margins are tightly monitored.
-
Time to iteration
- Small molecules: faster dose finding and structure-activity optimization.
- Gene therapies: longer manufacturing and safety cycles but potentially durable benefit once optimized.
These strategies are complementary and could eventually be combined.
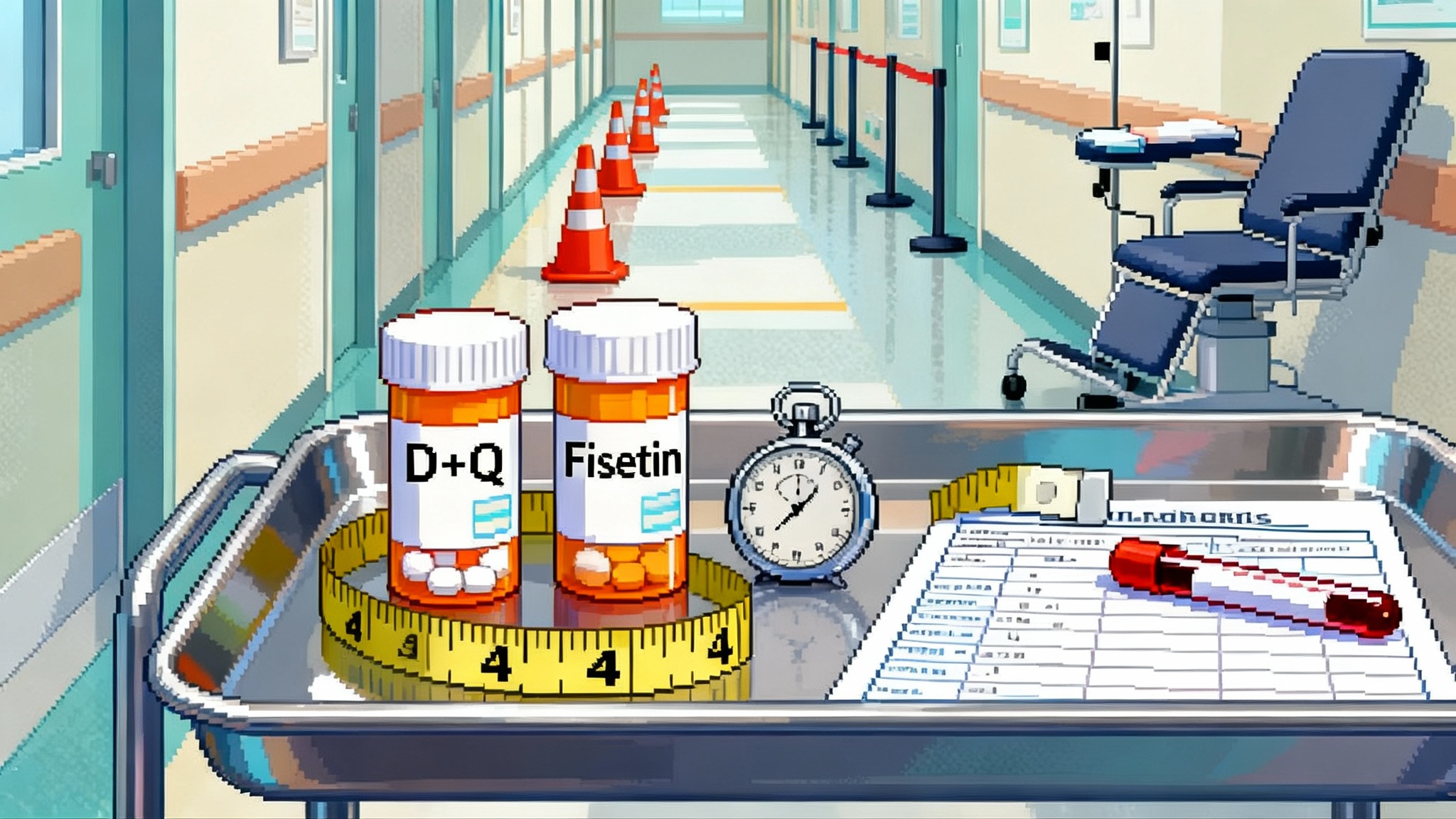
The de-risk checklist for broader healthspan claims
- Mechanism: robust, orthogonal evidence of restored autophagy flux in humans.
- Disease biology: directional changes in CSF tau species and neurodegeneration markers such as plasma NfL, ideally with astroglial marker support.
- Clinical function: statistically significant benefits on cognitive composites and functional measures aligned with the biomarker trajectory.
An additional layer after an Alzheimer’s readout would be translation to a second organ, for example liver disease with imaging-based fat and fibrosis metrics plus peripheral autophagy markers.
What to watch through 2026
-
Safety and tolerability
- Adverse events across dose levels in healthy volunteers and patients, with attention to infection and metabolic signals.
- Pharmacokinetics that support brain exposure modeling and low variability at steady state.
-
Target engagement
- Peripheral autophagy readouts showing real flux restoration.
- CSF biomarker movement in early cohorts, with a coherent pattern across p-tau, total tau, and possibly amyloid.
-
Early clinical signal
- Directional improvement on sensitive cognitive composites at 6 to 12 months that matches biomarker shifts.
-
Comparative momentum across rejuvenation approaches
- Ocular reprogramming programs entering first-in-human testing in 2026 with careful safety monitoring and dose control.
-
Pipeline spillover
- If brain-first autophagy shows promise, expect mitophagy in heart failure, proteostasis restoration in liver disease, and immune autophagy tuning in immunosenescence to follow.
The bigger picture
Longevity is unlikely to arrive as a single sweeping pill. It will enter medicine through organ-specific wins that map back to core hallmarks of aging. Retro’s brain-first autophagy study is a pragmatic bet that the fastest route to healthspan is to succeed on a disease label today. If safety, biomarkers, and cognition line up, RTR242 could help patients with Alzheimer’s and open a scientific and regulatory lane for hallmarks-driven therapeutics across the body.