FDA LDT Rollback Resets the Longevity Biomarker Market
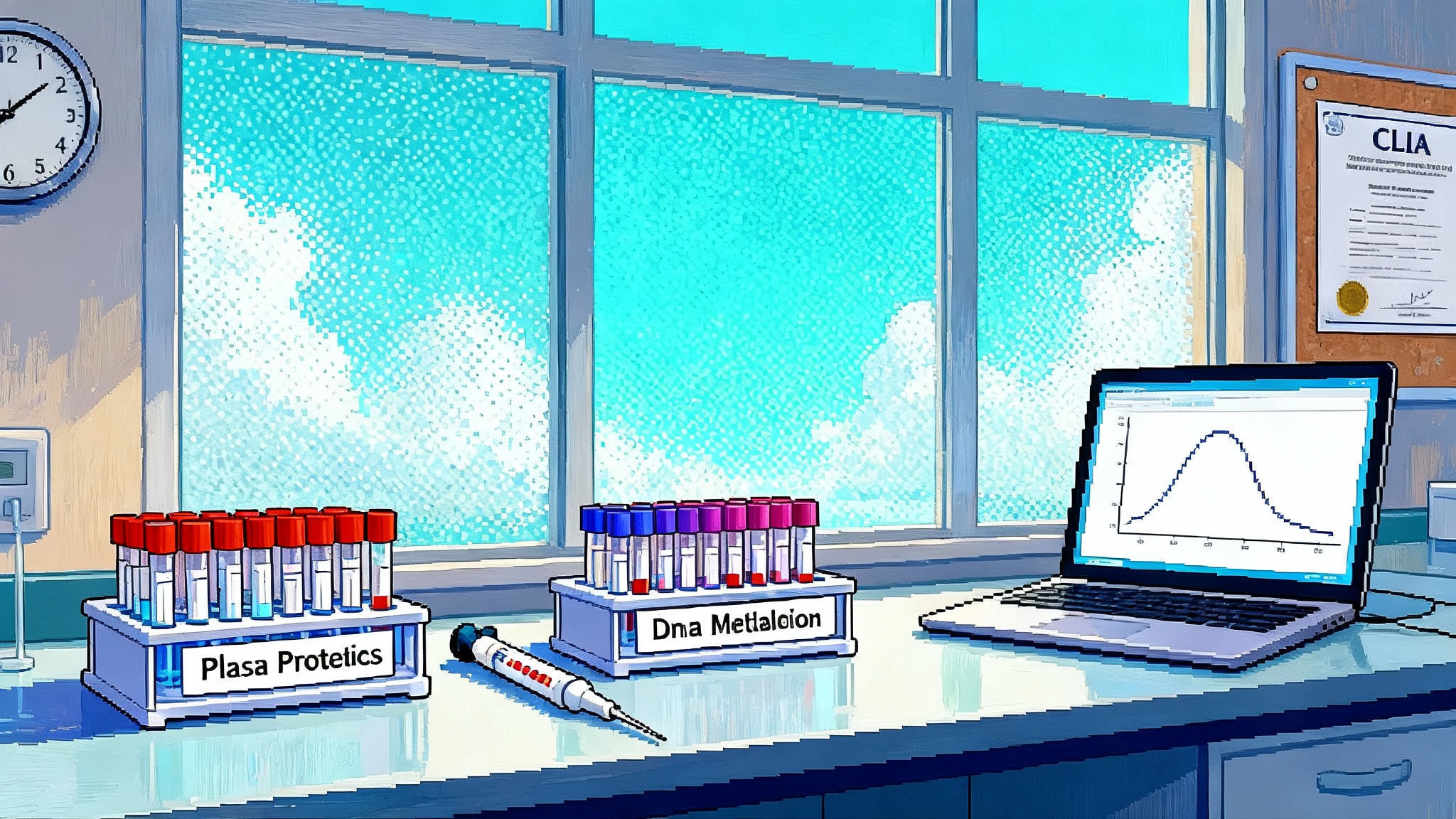
A 2025 court decision and FDA rescission return LDTs to CLIA oversight. Epigenetic clocks and proteomic biological age panels are reentering clinics. Here is what changes for validation, safety, and reimbursement.

The regulatory reset that reopened the door
On March 31, 2025, a federal district court in Texas vacated the FDA’s 2024 rule that would have brought most lab-developed tests under device regulations. The agency did not appeal within the 60-day window, and on September 18, 2025 it issued a final action to rescind the rule, effective September 19, 2025, returning LDT oversight to the long-standing framework of CLIA certification and inspection. For diagnostics at the heart of longevity care, that change is not academic. It is the reason epigenetic clocks and proteomic biological age panels are flowing back into hospital labs and specialty clinics. For a primary report on the policy turn, see how the FDA rescinds the LDT rule.
The immediate consequence is simple. Labs can again launch and offer LDTs without FDA premarket review, so long as they meet CLIA requirements and any applicable state standards. The practical consequences are more nuanced. CLIA is built to ensure a lab can run a method accurately and reproducibly. It is not designed to weigh whether a test actually changes clinical outcomes. That distinction sits at the center of how longevity biomarkers will be used, paid for, and trusted in the years ahead. For background, see our primer on CLIA vs FDA oversight.
What “back under CLIA” really means for longevity tests
CLIA classifies all LDTs as high complexity. That triggers rigorous requirements for laboratory personnel, quality systems, proficiency testing where available, and method validation. In plain terms, a lab must establish that its assay produces numbers that are accurate, precise, and stable across conditions. CLIA does not, however, make a lab prove that those numbers correlate with disease risk, that they respond to interventions, or that acting on them improves outcomes. A useful summary from NIH’s NCBI explains that CLIA does not regulate clinical validity, while FDA review, when it applies, considers whether a test’s claims are supported by clinical evidence.
For longevity biomarkers, this distinction is decisive. Epigenetic age acceleration or a proteomic age score can be measured with high analytical fidelity. Whether those scores should prompt a statin, a GLP-1, a sleep apnea referral, or a specific training block is a different threshold. The rollback puts the burden of that gap on laboratories, clinicians, payers, and professional societies rather than on an FDA review process.
Epigenetic clocks reenter the clinic
DNA methylation assays that estimate biological age have always lived a dual life. In research, where the first generation clocks were built, they have been invaluable for studying aging trajectories, social determinants of health, and the impact of exposures. In clinics, they have had a bumpier path, with questions about batch effects, cell-type composition, and algorithm transportability from research cohorts to real-world patients. For a deeper overview, see epigenetic clocks explained.
With the rollback, expect a new wave of methylation-based LDTs to show up in longevity and preventive cardiometabolic clinics. What changes this time is not just permission but maturity. Second and third generation clocks, often trained on morbidity and mortality rather than chronological age alone, are more clinically relevant. Some labs now bundle age acceleration with estimates of inflammation load, immune cell composition, and telomere length proxies, then present a composite risk narrative. The strong labs will be transparent about preanalytical variables like shipping time and temperature, bisulfite conversion controls, and how they correct for white blood cell subtype fractions. The best will publish method comparison data against orthogonal platforms and will show test-retest metrics in the same individual over short intervals.
Still, clinicians should remember what these scores are not. An epigenetic clock is not a diagnosis. It is a biomarker that may correlate with future risk and may capture multisystem physiology. It should be interpreted alongside traditional risk calculators, imaging, and phenotypic markers such as VO2max, grip strength, and visceral adiposity.
Proteomic biological age panels return with scale
Proteomics has raced forward in the last five years. High-plex platforms can now quantify thousands of proteins from a small plasma volume. Aging-focused models have emerged that compress this high-dimensional data into an age estimate or a risk score that purports to anticipate incident disease and mortality. The appeal is obvious. Proteins are closer to phenotype and to druggable pathways than DNA methylation marks. They can respond quickly to training, diet shifts, and new medications. Explore implementation essentials in our proteomic biomarkers guide.
Under CLIA, clinical labs can again offer these panels without FDA clearance, provided they establish performance specifications, instrument calibration, internal control limits, and lot-to-lot comparability. Expect more clinics to offer a simple blood draw that yields a biological age number plus pathway-level insights, for example inflammatory tone or cardiometabolic burden, within two weeks. The implementation details will matter. How a lab handles sample stability, freeze-thaw cycles, biotin interference, and calibration drift across instrument runs will determine whether a 3-point change in a patient’s age score is signal or noise.
Validation that actually matters: three layers
If you are a physician, medical director, or self-pay consumer, look for evidence at three distinct levels:
- Analytical validity
- Precision and reproducibility: Same sample, different runs, how tight is the coefficient of variation. Labs should share replicate data and quality control charts.
- Accuracy and traceability: What external standards or reference materials are used. For methylation arrays, how are control probes and normalization handled. For proteomics, how do they correct for batch effects and instrument drift.
- Reportable range and limits: What is the range over which the assay is linear. What is the lower limit of detection and quantitation for key features.
- Clinical validity
- Association with outcomes: Does the score predict incident disease, mortality, or relevant phenotypes in independent cohorts that resemble real patients, not just biobank volunteers.
- Transportability: Has the model been validated across ages, sexes, ancestral backgrounds, and comorbidities. Are there calibration plots that show error by subgroup.
- Responsiveness: Does the biomarker change in a biologically plausible direction after interventions known to move risk, such as weight loss, smoking cessation, antihypertensives, or sleep apnea treatment. Beware short studies with lifestyle bundles where it is hard to attribute causality.
- Clinical utility
- Impact on management: Does the test change decisions beyond standard of care risk tools. For example, did adding the biomarker reclassify patients correctly into statin or GLP-1 therapy in a prospective protocol.
- Impact on outcomes: Are there trials or well designed pragmatic studies showing that acting on the test improves surrogate endpoints, quality of life, or hard outcomes. Absent that, is there a coverage with evidence development plan.
CLIA directly enforces the first layer. The second and third layers require publication, professional guidance, payer assessment, and responsible clinic policies.
Consumer safety in a CLIA-only world
When FDA is not reviewing claims, marketing guardrails rely on other mechanisms. That is not a reason to avoid testing. It is a reason to apply basic safety filters:
- Physician oversight: Prefer labs that require an order by a licensed clinician who will review results with you. Some states require it, and it reduces the risk of misinterpretation.
- Clear intended use: The report should state what the test measures and what it does not. A biological age score should not be labeled as a diagnostic for any disease.
- Transparent methods: Look for a methods section that describes sample handling, platform, bioinformatic pipeline, drift correction, and quality metrics. If it reads like an advertisement, treat the result accordingly.
- Conservative recommendations: Reports should suggest follow-up testing or lifestyle steps that align with consensus guidelines. Any drug suggestions should be routed through your physician and anchored in existing indications.
- Data privacy: Confirm data use policies for your omics data, including whether de-identified data are shared with third parties and whether you can opt out.
- Retesting cadence: Avoid monthly retesting. For most people, a six to twelve month interval is reasonable, unless you are in a targeted intervention study with explicit protocols.
What payers are likely to do next
Coverage will hinge on clinical utility. Payers already reimburse for many risk markers that guide therapy, such as LDL-C or lipoprotein(a), because acting on the results is linked to outcome improvements. Longevity biomarkers will be judged by the same standard. Expect several patterns:
- Wellness positioning in employer plans: Some proteomic or methylation age panels may be offered as optional wellness benefits, where the goal is engagement rather than medical decision making, often outside the core medical benefit.
- Coverage with evidence development: Health systems may negotiate pilot coverage if the lab runs a prospective outcomes registry with predefined endpoints and transparent data sharing.
- Narrow indications first: If a biomarker can improve the identification of rapidly aging phenotypes in a specific high-risk group, for example adults with HIV or survivors of cancer therapy, payers may consider targeted coverage sooner.
- Coding and payment levels: Without FDA clearance, many tests will be billed under miscellaneous or PLA codes with variable payment. That is tolerable for boutique clinics and self-pay markets, but it is not a scale strategy. Expect labs to build economic models that assume limited coverage for now, with subscription-like bundles that include testing and longitudinal coaching.
How responsible clinics will use these tests now
A reasonable clinical workflow in the CLIA-only environment looks like this:
- Baseline assessment: Comprehensive history, lifestyle, medication review, vitals, and standard labs, including fasting lipids, A1c, renal and liver function, high sensitivity CRP if indicated, and body composition where feasible.
- Biomarker selection: Choose one aging biomarker modality that fits the question being asked. For cardiometabolic focus, a proteomic score that captures inflammatory and metabolic pathways may add more value. For life course risk or research-oriented patients, a methylation age with multiple derived clocks can be informative.
- Preanalytical controls: Use phlebotomy or sample kits that the lab specifies, with attention to shipping windows and temperature. Document any deviations.
- Counseling at result delivery: Frame the biomarker as a risk signal, not a diagnosis. Use the result to personalize but not to replace evidence-based interventions. If the test suggests elevated cardiometabolic burden, the next steps should still start with established therapies and lifestyle changes.
- Follow-up interval: Recheck no sooner than six months unless there is a protocolized reason. Do not chase small changes that fall within the assay’s test-retest variation.
- Registry participation: Encourage patients to consent to contribute de-identified outcomes data. This is how the field will advance beyond correlations.
Practical checklist for evaluating a biological age test and its claims
Use this list before you order, adopt, or pay for a test:
- Intended use: Is it clearly stated and limited to risk assessment.
- Analytical validation: Is there a white paper with precision, accuracy, reportable range, and control procedures. Are there third party comparisons or external quality assessments.
- Preanalytical robustness: Does the lab disclose sample stability windows, acceptable shipping times, and effects of common interferents like biotin or hemolysis.
- Model transparency: Is the algorithm described in enough detail to understand inputs and outputs. Are there peer-reviewed publications, not just posters, validating performance in real-world cohorts.
- Subgroup performance: Are error rates disclosed by age, sex, BMI category, ancestral background, and comorbidity burden.
- Clinical utility claim: Does the company claim its test changes decisions or outcomes. If so, is there prospective evidence or is it an extrapolation from association studies.
- Report design: Are recommendations aligned with major guidelines. Do they suggest off-label medications or unproven supplements.
- Data use and retention: Can you delete your raw data. Is data sharing opt-in or opt-out.
- Cost clarity: What is the total price, including phlebotomy and follow-up consultation. Are there refunds for failed samples or out-of-spec results.
- Retest policy: What interval is recommended and why. Is it based on biological reasoning and assay variability, or on revenue targets.
The near future of biomarker-driven longevity care
The rescission will accelerate innovation. More labs will enter, models will iterate faster, and clinics will have choices. That also means more noise. The field can avoid past mistakes if it focuses on three moves:
- Raise the bar on analytical transparency: Publish control charts, make batch correction strategies explicit, and participate in inter-laboratory comparisons.
- Build outcomes registries: When a clinic orders an aging biomarker, capture downstream decisions and outcomes. Even observational data, collected carefully, can inform utility.
- Seek narrow, high-yield indications: Instead of broad claims like better aging, pursue patient groups where the biomarker is most likely to change care, for example tailoring intensity of cardiometabolic therapy in people with discordant traditional risk markers.
Regulation will not stand still. States with their own clinical lab evaluation programs can tighten expectations. Professional bodies can issue guidance that distinguishes between markers suitable for lifestyle programs and those appropriate for clinical decision making. Congress could revisit comprehensive diagnostics legislation. Regardless, the center of gravity has shifted back to laboratories and clinicians to prove value.
Bottom line
The 2025 rollback ends, for now, a decade-long tug of war over FDA’s role in LDT oversight. It does not end the need for rigor. Epigenetic and proteomic age tests can be powerful lenses on physiology when they are analytically tight, clinically grounded, and used to complement, not replace, standard risk tools. If you are bringing these assays into a clinic, demand clarity on what is measured, how stable the measurement is over time, and what actionable steps follow. If you are a consumer, treat biological age as a compass, not a verdict. The promise of biomarker-driven longevity care is real, but only if we align enthusiasm with evidence and keep patient safety at the center.