Midlife Shock: Arteries Emerge as Aging’s Command Hub
A new human proteomic atlas points to a sharp midlife inflection and puts arteries at the center of systemic aging. Here is a practical, 12 to 18 month roadmap to test vascular-first diagnostics and repurposed drugs.
The news: a midlife bend and a vascular command center
Every few years aging research gets a map that changes how we navigate the field. In late July 2025, a Cell paper dropped a proteomic atlas of human organ aging and two findings jumped off the page. First, aging is not a steady glide. There is a marked inflection in midlife, roughly ages 45 to 55, when molecular change accelerates across multiple tissues. Second, the vasculature is not just another passenger. Arteries look like a system-level hub that broadcasts aging signals throughout the body. The authors also surfaced a set of vascular-derived senoproteins, with growth arrest specific 6, better known as GAS6, identified as a candidate driver of vascular and systemic aging. The atlas is worth reading in full; its abstract captures the midlife bend and the vascular signal broadcast clearly in the Cell proteomic atlas of human aging.
If that holds up, it is a pivot point. A field that often pursues organ-by-organ fixes would need to move vascular-first. The practical consequence is straightforward: prioritize interventions that modulate arterial senoproteins and their receptors; validate midlife diagnostic panels that read vascular signaling from blood; and embed low-cost digital endpoints that give real-time vascular age from wearables. For context on how clinical biomarkers are re-entering practice, see how aging clocks return to the clinic.
Why arteries moved to the front of the line
Think of the vasculature as both highway and intercom. Endothelial and smooth muscle cells line every route in the body. They constantly sense, secrete, and respond. When these cells adopt a senescent program, they do not just retire. They talk. The secreted proteins in their senescence-associated mix are not noise. They are messages other organs hear.
The Cell atlas points to arteries as an early and vulnerable tissue, then highlights a handful of senoproteins with plausible mechanisms of action:
- GAS6: a vitamin K dependent ligand for the TAM receptor family AXL, MERTK, and TYRO3, positioned to rewire survival and inflammatory signaling in vascular cells.
- GPNMB: a glycoprotein that rises in stressed tissues and macrophages, tied to senescence programs and matrix remodeling.
- HTRA1: a secreted serine protease implicated in microvascular disease of the retina and brain, capable of reshaping the extracellular environment by clipping key substrates.
- IGFBP7: an insulin-like growth factor binding protein that recurs in senescence studies and as a clinical biomarker in kidney stress; it can push healthy cells toward a senescent state in vitro.
A hub makes testable predictions. If arteries set the tempo, then plasma should echo arterial secretions; midlife cohorts should show step-changes in vascular-derived proteins; and interventions that quiet these proteins or their receptors should register system-wide benefits out of proportion to the local action.
The intervention pivot: vascular-first and senoprotein-aware
The immediate opportunity is not science fiction. It is repurposing. Several drug classes already touch the pathways above and have human safety data.
- AXL and the broader TAM pathway. Selective AXL inhibitors and multi-kinase inhibitors with AXL activity have been tested in oncology and fibrosis. That provides pharmacokinetics, target engagement biomarkers, and dose ranges to start proof-of-mechanism studies outside cancer. Small molecules can be titrated to avoid overshooting immune homeostasis, since TAM receptors modulate inflammation and efferocytosis.
- Anti-GAS6 strategies. Decoy receptors and antibodies have advanced in cancer. A vascular-aging program would aim not to obliterate signaling but to normalize it in midlife subjects with a high vascular age gap.
- HTRA1 modulators. An anti-HTRA1 antibody fragment has shown pharmacodynamic effects in the eye in geographic atrophy, with substrate cleavage biomarkers like DKK3 tracking target engagement. That is a ready blueprint for systemic assays and dose finding in vascular disease biology, even if the route and exposure will differ from intravitreal dosing. For translational momentum from eye to aging, see our report on senolytic eye trial progress.
- IGFBP7 neutralization. Antibodies and binding proteins have circulated in preclinical pipelines, and clinical labs already quantify IGFBP7 in Critical Care. That combination of mechanism and measurement lowers the barrier to a first-in-human vascular aging study.
- GPNMB targeting. Antibodies and antibody drug conjugates against GPNMB reached human trials in oncology. Toxic payloads are not the goal here, but the targeting knowledge is useful for designing neutralizing or ligand-trap approaches aimed at senescence signaling without cytotoxicity.
The playbook is to move quickly but precisely: soft landings on dose, rich biomarker readouts, and digital endpoints that make trials scalable.
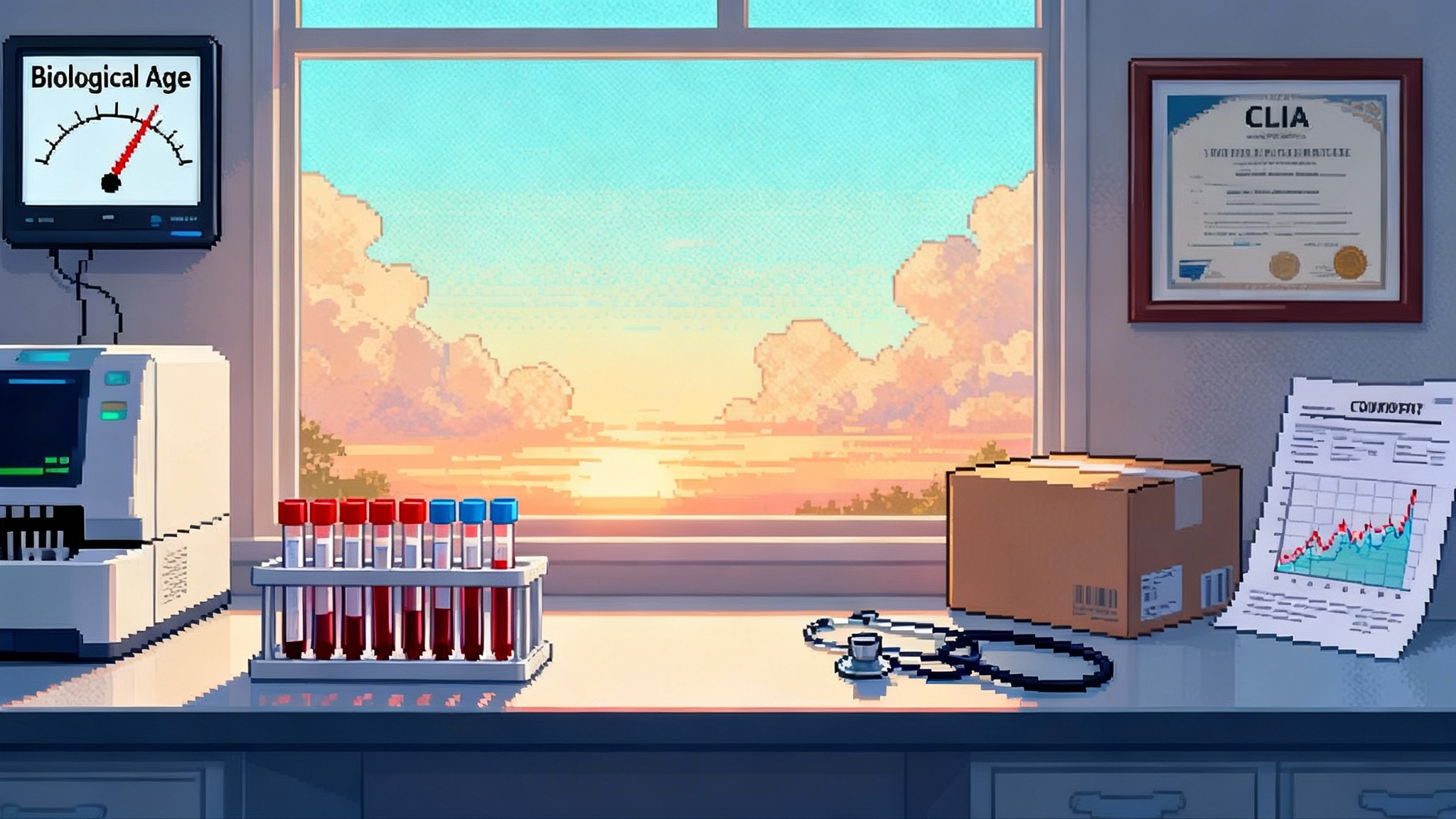
The diagnostic backbone: blood plus a wrist
A vascular-first strategy needs a diagnostic spine that is just as fast as the repurposing program. That spine has two vertebrae.
-
Plasma proteomics tuned to the arterial secretome. Start with a compact panel centered on GAS6, IGFBP7, HTRA1, and GPNMB, then add a small number of co-regulated proteins from the atlas. Run it on platforms available in most translational labs. Calibrate the panel against age and risk factors, but anchor it to outcomes and physiology, not just birthdays.
-
A low-cost digital endpoint for vascular age. Photoplethysmography, the optical pulse signal in watches and rings, now supports deep learning estimates of vascular age at population scale. A 2025 analysis trained on United Kingdom Biobank wrist data reported that a large vascular age gap, the difference between model-predicted vascular age and calendar age, tracked future major cardiovascular events and mortality. It is not perfect, but it is deployable at home and improves whenever the model retrains. If you need a single reference to the state of the art, start with the AI vascular age from PPG study.
The benefit of this backbone is practical. It keeps recruitment and follow-up within reach for mid-size teams and budgets. It also allows you to frame the whole program as a systems question: do we see a coherent shift in plasma senoproteins and in AI vascular age when we modulate a single pathway like AXL or HTRA1.
A 12 to 18 month roadmap from atlas to action
Below is a pragmatic timeline that a focused consortium can execute. It assumes access to a CLIA lab partner, a wearable partner or off-the-shelf devices, and one repurposing asset with a clean safety record.
Months 0 to 3: data lock and panel build
- Curate the minimal proteomic panel. GAS6, IGFBP7, HTRA1, GPNMB plus three to five atlas-linked co-factors that improve discrimination in cross-validation.
- Stand up assays. Use validated immunoassays where available. Where not, develop sandwich assays with orthogonal mass spectrometry confirmation in a 50-sample pilot.
- Pretrain the digital endpoint. Fine-tune an open or licensed photoplethysmography vascular age model on a retrospective cohort with paired arterial stiffness measures and blood draws. Define a preregistered algorithm lock and a plan for drift monitoring.
Months 3 to 6: midlife screen and phenotyping
- Recruit 500 adults ages 40 to 55. Oversample for cardiometabolic risk and family history. Exclude uncontrolled hypertension and active inflammatory disease to avoid confounding.
- Measure the panel and compute a vascular age gap for each participant. Define strata: high gap, neutral, low gap. Collect reference physiology: pulse wave velocity, flow-mediated dilation, heart rate recovery, and a short three-minute step test with photoplethysmography to stress the system.
- Predefine a composite vascular aging score. Weight plasma senoproteins and the digital age gap to map individuals to a continuous risk axis.
Months 6 to 12: proof-of-mechanism randomized studies
- Study A: AXL pathway modulation. Randomize 80 midlife participants with a high vascular age gap to low-dose AXL inhibition or placebo for 12 weeks. Primary endpoint: change in composite vascular aging score. Key secondaries: individual senoproteins, resting and exertional pulse wave velocity, safety labs, and an immune panel to monitor infections and wound healing signals.
- Study B: HTRA1 modulation. If a systemic HTRA1-targeting agent is not available, use an ex vivo paradigm. Treat collected plasma with a selective HTRA1 inhibitor in vitro and quantify changes in endothelial cell senescence markers and matrix substrate cleavage. In parallel, run a small first-in-human microdose study if feasible under exploratory Investigational New Drug rules, using substrate cleavage biomarkers to confirm target engagement.
- Study C: IGFBP7 neutralization. A short crossover design in 30 midlife adults compares a single dose of an IGFBP7 binder versus placebo on post-exercise endothelial function and next-day plasma senoproteins.
Months 12 to 18: selection and scale-up
- Rank assets by effect size on the composite score and by safety margin. Advance the top program to a 6 month Phase 2a focused on durability and dose response.
- Lock the diagnostic. Convert the proteomic panel to a laboratory developed test with clear reporting of the composite score and its drivers. Publish the algorithmic specification and predefine how updates will be versioned.
- Share the digital endpoint. Release a reference implementation and a validation report so other teams can replicate and extend in different populations and devices.
Trial design details that keep costs down and learning high
- Population. Focus on ages 40 to 55 to catch the inflection window. Enrich for individuals with a vascular age gap of 9 years or more and for elevated baseline senoproteins.
- Size. Start small but informative. For a 0.4 to 0.5 standard deviation shift in the composite score, 40 per arm gives a credible read with repeated measures and mixed models.
- Endpoints. Define a single composite and commit to it. Pre-specify how each senoprotein and the digital age gap contribute. Keep classical physiology endpoints secondary but do collect them.
- Biomarkers. Include a simple panel of coagulation and innate immunity markers. The TAM axis and HTRA1 touch hemostasis and extracellular matrix; you want early warning of drift.
- Safety. Midlife research participants will tolerate little risk. Use the lowest active doses, short exposures, and stepwise stopping rules. Include an independent monitor empowered to pause after any cluster of adverse events.
How network medicine speeds repurposing
Repurposing is faster when you treat biology as a graph problem. The vascular hub hypothesis gives you a set of nodes, like AXL and HTRA1, and measurable outputs, like GAS6 and IGFBP7 in plasma. The network medicine playbook then does three things well:
- Module detection. Project senoproteins onto a high-confidence interactome and identify the smallest set of candidates that control the module’s state.
- Drug proximity. Map approved and investigational drugs to the module and compute a proximity score. Prioritize assets with close targets, good safety, and oral dosing.
- Real-world checks. Use longitudinal biobanks and claims data to ask whether people already taking a given class show the predicted plasma or digital signature. This is not causal proof, but it is a strong triage step.
Run that loop quarterly and you will keep finding opportunities that the field overlooks when it chases single targets. Cardiovascular partners aligned with prevention programs, including those advancing Lp(a) therapies go mainstream, are well positioned to help.
What could go wrong and how to design around it
- Over-suppression of TAM signaling. AXL and its relatives help tune immune clearance of dying cells. Blunt them too much and infections or poor wound healing could creep up. Solution: aim for normalization, not flatline, and include immune monitoring.
- HTRA1 as a double-edged protease. Proteases have many substrates. The ocular precedent helps, but systemic dosing could surface surprises in vessels or cartilage. Solution: couple dosing to substrate cleavage biomarkers and escalate slowly.
- Digital endpoint drift. Wearable optical signals vary by skin tone, motion, and device model. Solution: lock models before trials, prospectively monitor drift, and keep a small gold-standard subset with tonometry and echotracking.
- Hype outpacing evidence. The atlas is a starting line, not a finish line. Solution: preregister analyses, share negative results, and publish full assay performance, including failures.
Who can move first
- Academic proteomics centers with clinical assay capability can build the initial panels in weeks, not months.
- Biotechs with AXL, protease, or growth factor binding programs can deliver low-dose, biomarker-rich studies quickly because their chemistry and toxicology are mature.
- Wearable companies and digital biomarker groups can provide validated photoplethysmography pipelines, enable home data collection, and reduce site costs.
- Payers and employers that already sponsor midlife health programs can underwrite trials because the endpoints are continuous and meaningful and the interventions are oral and short.
The bottom line for 2026
The 2025 atlas reframes the question of longevity. If arteries are the senescence intercom, then midlife medicine should listen to the intercom and learn how to turn the volume down. That calls for a vascular-first agenda built on three legs: a compact plasma panel anchored in arterial senoproteins, a practical digital endpoint that reports vascular age from the wrist, and a set of fast-follow repurposing studies that modulate AXL and HTRA1 with biomarker discipline.
The reward is outsized. If you can shift the composite vascular aging score in a few months without safety tradeoffs, you have a lever that touches brain, kidney, muscle, and immune aging through a single system. In a field that loves big promises, this is a rare case where the map points to a road we can actually drive. The detour is over. The fastest way to slow whole-body aging may start in the arteries and it can start now.