Pig organs enter the clinic: kidneys and livers in 2025
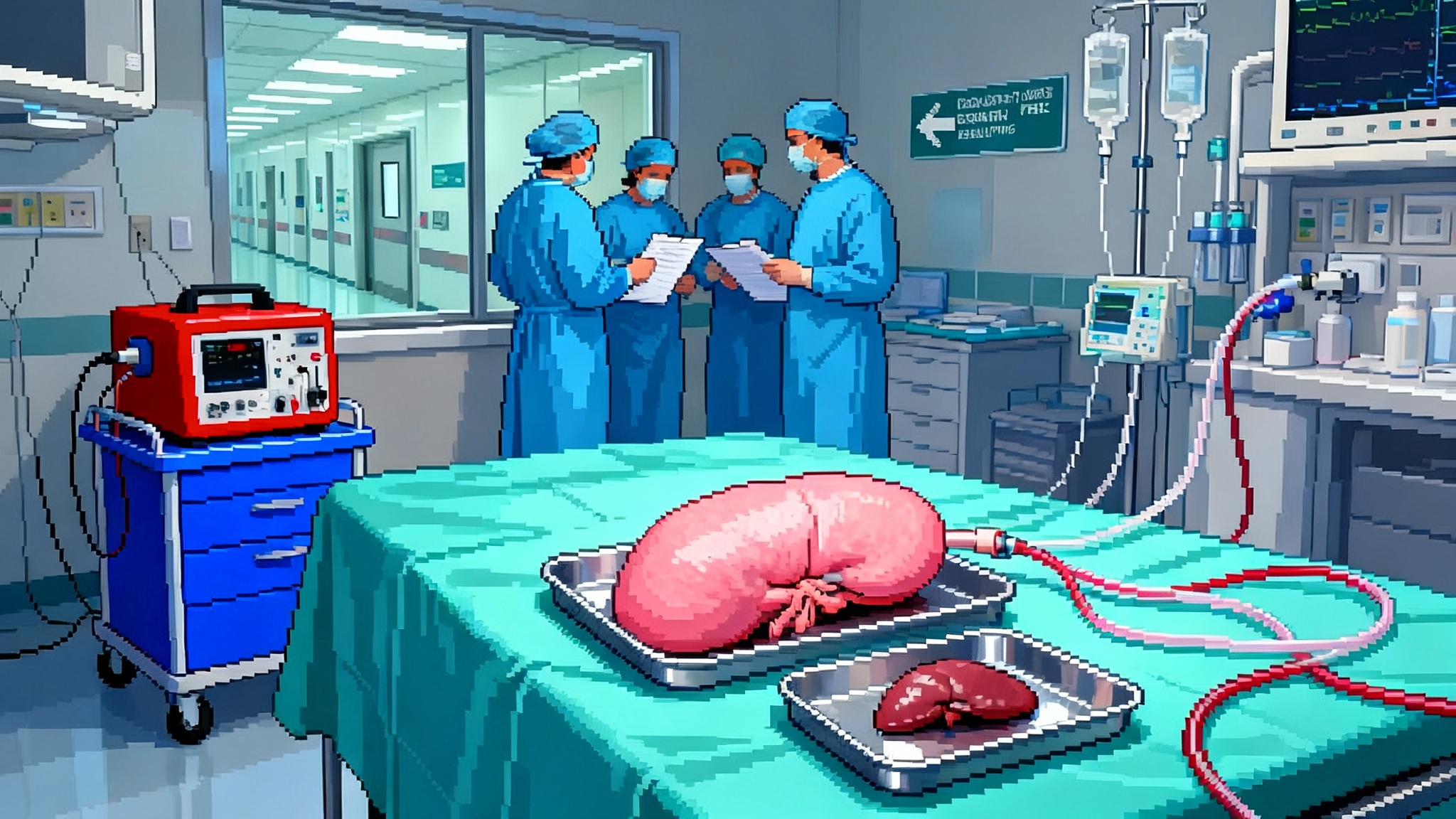
In 2025, gene-edited pig kidneys and livers supported function in living patients. On January 25, 2025, Mass General implanted a second gene-edited pig kidney into a living recipient. On October 9, 2025, a peer-reviewed case reported an auxiliary pig liver sustaining function for 38 days. Organ failure is turning into an engineering problem.
The week organ failure became an engineering problem
On January 25, 2025, a surgical team at Massachusetts General Hospital transplanted a gene-edited pig kidney into 66-year-old Tim Andrews and discharged him a week later, off dialysis and walking out of the hospital. The program leads detailed 69 genomic edits to the donor pig and credited new immune control drugs from partners Apellis and Eledon. Read the primary source capturing this tipping point in Mass General’s January 25 transplant announcement.
Nine months later, hepatologists opened a new chapter. On October 9, 2025, the Journal of Hepatology published the first report of a genetically edited pig liver supporting function inside a living human. The graft was an auxiliary liver placed alongside the patient’s native organ; it produced bile, synthesized clotting factors, and sustained key functions for more than a month before removal on day 38 due to a clotting complication. The patient survived for 171 days. See the peer-reviewed account in the Journal of Hepatology case report.
If 2024 was the proof-of-concept year, 2025 is when xenotransplantation entered the clinic with intent. The kidney case shows durable function in a living recipient with a plan, not only a permission slip. The liver case shows that pig tissue can carry human metabolic load inside a patient, not just on an external perfusion machine. The common thread is deliberate engineering, from DNA to bedside logistics.
From miracle to method
Think of xenotransplantation as replacing a machine, not as borrowing a miracle. To make a pig organ run safely in a human body, teams must solve a few engineering jobs at once.
-
Change the hardware. Engineers edit the pig genome so its cells look less foreign. Classic edits delete three sugar-making genes that humans attack, while adding human proteins that calm the immune and clotting systems. In the Mass General kidney, the donor pig carried 69 edits, which included removal of porcine endogenous retroviruses and addition of human complement and coagulation guards. In the liver study, the team used a pig with 10 well-chosen edits. The exact mix may differ by organ, but the principle is constant: tune the surface and the signaling so human blood does not see an alarm.
-
Quiet the software. Even a well-edited organ can trigger a storm. That is why the clinical teams layered targeted immune control. Costimulation blockade, which interferes with T cell activation at the CD40 and CD154 handshake, acts like removing the ignition key from immune cells. Complement inhibitors temper an ancient protein cascade that otherwise coats foreign tissue and drills holes in cell membranes. In the kidney case, Mass General credited Apellis and Eledon for the immunosuppressive backbone. In the liver case, when a microvascular clotting syndrome flared, the team treated with plasma exchange in 2025 trials and a complement inhibitor, then removed the auxiliary graft. For context on immune-system tuning beyond transplantation, see thymus reboot in 2025.
-
Stabilize the plumbing. Pigs and people have different rheology and clotting balance. The most feared early failure in xenografts is a chain reaction at the capillary wall, part immune, part coagulation, that locks up the microcirculation. Clinicians call this xenotransplant-associated thrombotic microangiopathy, or xTMA. Good edits and complement control reduce its odds. Clear perioperative plans for heparin, platelet thresholds, and transfusion support are the practical part of the solution.
-
Manage the biosafety envelope. Every organ carries microbes and viral fragments from its donor. The field has a conservative answer. Breed animals in clean facilities, screen them like blood products, and silence embedded pig retroviruses in the genome. The goal is redundancy, not a single barrier.
This is not magic. It is systems engineering under sterile lights.
Why 2025 marks an inflection
The kidney and liver anchors shift the story in three ways.
-
Living recipients, not only decedents. Transplants into people who are awake and recovering create real-world data about function, adherence, and quality of life. When Tim Andrews describes energy returning, it reads like a device turning on. That matters because more than 500,000 Americans live on dialysis today, and dialysis trades time for time, often at a heavy cost in energy and work.
-
Defined playbooks, not heroic exceptions. Mass General’s release lists the gene edits, the companies behind the immunotherapies, and the United States Food and Drug Administration pathway, Expanded Access followed by trials. The Journal of Hepatology paper documents complications, treatments, and autopsy findings. These are templates, not headlines.
-
Organ-specific learning. Kidneys are filters, livers are factories. The kidney is a simpler immunologic target and has shown the first durable wins. The liver makes proteins, detoxifies blood, and controls clotting. The auxiliary graft model lets a team add support without removing the native organ, which is ideal for bridging a patient to transplant or recovery. In both organs, the bottleneck is no longer biology alone. It is standardization, supply, and perioperative control.
A simple map of the biology
-
Hyperacute rejection: minutes to hours. Driven by natural antibodies and complement. Modern edits remove the pig sugars that trigger this, and human proteins like CD46 and thrombomodulin create a local ceasefire.
-
Acute cellular rejection: days to weeks. Driven by T cells. Costimulation blockade short-circuits the activation handshake. That is the point of new agents from companies like Eledon.
-
Clotting and xTMA: days to weeks. Part immune, part endothelial injury, part hemodynamics. Complement inhibitors and careful heparin management help. Human thrombomodulin transgenes and endothelial protein C receptor transgenes are edits designed to keep blood flowing.
-
Infection risk: always. Use designated pathogen-free herds, test animals and organs like blood products, and silence endogenous retroviruses. The kidney program explicitly notes inactivation of porcine endogenous retroviruses, which removes a theoretical infection route.
None of these items require a breakthrough in basic science. They require consistency and checklists.
The near-term roadmap, 2026 to 2027
- Standardize the edit sets
- What to do: Converge on organ-specific gene edit menus that balance immune calm and healthy organ physiology. For kidneys, a high edit count may be fine. For livers, fewer edits with tight coagulation control may be better.
- Why: Regulators and payers adopt what they can audit. A small number of edit recipes per organ will let centers coordinate supply and trials.
- How: Multi-center consortia can pre-agree on two or three edit sets per organ, matched to drug regimens. Publish the bill of materials. Publish the manufacturing quality controls. Share adverse events in near real time.
- Manage xTMA and coagulation
- What to do: Build standardized anticoagulation and complement pathways into care. Use early biomarkers like fragment Bb and D-dimer as triggers, as highlighted in SenNet’s 2025 biomarker atlas.
- Why: The liver report shows how quickly a microvascular problem can force graft removal. The kidney cases show how complement control seems to extend the calm period after surgery.
- How: Preprint and adopt center-level xTMA bundles, similar to sepsis bundles, with ordersets, nurse checklists, and digital early warning scores. Share one-page graphs of the first 21 days for every patient, so a complication line is visible and actionable.
- PERV and pathogen safeguards
- What to do: Keep using pigs with retrovirus inactivation. Treat donor animals like blood donors. Add wastewater testing and environmental sequencing around farms and operating rooms as a belt and suspenders.
- Why: The risk is small but public trust is fragile. The stronger the biosafety envelope, the faster the field can move.
- How: Create a national registry that pairs each xenotransplant with a pathogen audit trail from pig birth to human discharge. Keep results public unless patient privacy prevents it.
- Machine perfusion and organ banking
- What to do: Extend preservation windows with hypothermic and normothermic perfusion. Use perfusion as a testbed for functional assays. For livers, consider a planned auxiliary approach in which the pig graft supports the native liver for weeks while the patient clears a crisis.
- Why: Longer windows let the supply chain behave like a real supply chain. Surgeons can plan, not rush. Payers can authorize care before the organ arrives.
- How: Co-locate edited pig herds, slaughter facilities, and perfusion labs near transplant centers. Use identical perfusion carts for pigs and humans to reduce training time. Validate simple release criteria, bile production for livers and creatinine clearance for kidneys.
- Equitable access and cost
- What to do: Set early price caps and risk-sharing contracts between manufacturers and payers. Tie payment to functional days gained in the first 90 days. Reserve a proportion of organs for safety-net hospitals.
- Why: Without guardrails, first-in-class therapies widen disparities. With them, they can bend mortality curves where the burden is highest.
- How: Medicare and large plans can pilot coverage-with-evidence frameworks that require outcomes reporting and equity metrics. States can fund patient navigation for dialysis centers that refer patients to xenotransplant trials, with incentives for rural and low-income clinics.
A realistic accelerationist view
Off-the-shelf pig organs will not erase transplant waiting lists overnight. They can, with tight bioengineering and perioperative discipline, start shifting years lost to years regained within this decade.
-
First as bridges. Auxiliary pig livers can buy time for a failing native liver to recover or for a human organ to arrive. Pig kidneys can carry a patient off dialysis and into a stronger state for a later human transplant.
-
Then as durable replacements. If kidneys keep working beyond twelve months in several living patients, the field will gain the confidence to offer long-term replacements to carefully selected groups, for example older patients with few other options, or highly sensitized patients who face years of waiting for a human match.
-
With data that compounds. Every edited organ yields a phenotype. Every perioperative bundle produces a safety curve. When centers share both quickly, learning compounds like interest.
What this means for people who measure their lives in dialysis sessions
-
Patients: Ask your nephrologist whether your center participates in xenotransplant trials and registries. If you have O blood type, understand that wait times are longer, which makes you a candidate for bridge strategies.
-
Clinicians: Build a standing order set for potential xenotransplant referrals. Assign a nurse and a coordinator who can move a patient from dialysis to surgical workup in under two weeks. Practice the xTMA bundle on simulated cases before you need it.
-
Hospital leaders: Stand up a small cross-functional unit that owns xenotransplant readiness, from infection control to pharmacy stocking to ethics consults. Budget for complement inhibitors and for perfusion carts. Treat this like the launch of a new service line with outcome dashboards, not a one-off.
-
Policymakers and payers: Require shared data, not perfect data. Pay for functional days gained and for avoided hospitalizations. Tie early coverage to transparent reporting of complications and to equity rules that prevent wealth from deciding access in the first wave.
The hard problems that still matter
-
Chronic rejection is a marathon. Weeks are no longer the limit. Years will bring new immune puzzles. Costimulation blockade looks promising, yet long-term safety and infection risk need careful watch.
-
Coagulation biology is organ-specific. The auxiliary liver case shows how close function and failure can sit. The right transgenes and perioperative anticoagulation may tip the balance, but the field needs large, comparable cohorts.
-
Manufacturing scale and quality will define the curve. Editing animals and raising them in clean facilities is expensive. Costs fall when the edit recipes stabilize and when batches are larger. That argues for coordination across centers and regulators now.
-
Trust will govern speed. Public confidence rises when programs publish what went right and what did not. Naming complications and the steps taken creates room for progress without hype.
A closing picture
A kidney that wakes a person up with energy. A liver that carries a human through weeks of danger. The pieces are concrete now: gene edits, complement control, costimulation blockade, perfusion carts, audit trails. Put together with discipline, they move organ failure from a binary fate to a controllable state. The next two years decide how fast this shifts from one hospital and one journal to many hospitals and many lives. If the field keeps treating organs like engineered systems, the mortality curve can start to bend, first as a bridge, then as a route.