Semaglutide’s 2025 Clock Signal and the Gerotherapy Question
A 2025 randomized-trial analysis reports semaglutide nudged several DNA methylation clocks toward a younger profile. Here is what that does and does not prove, and how to translate a weight-loss wave into real healthspan gains.
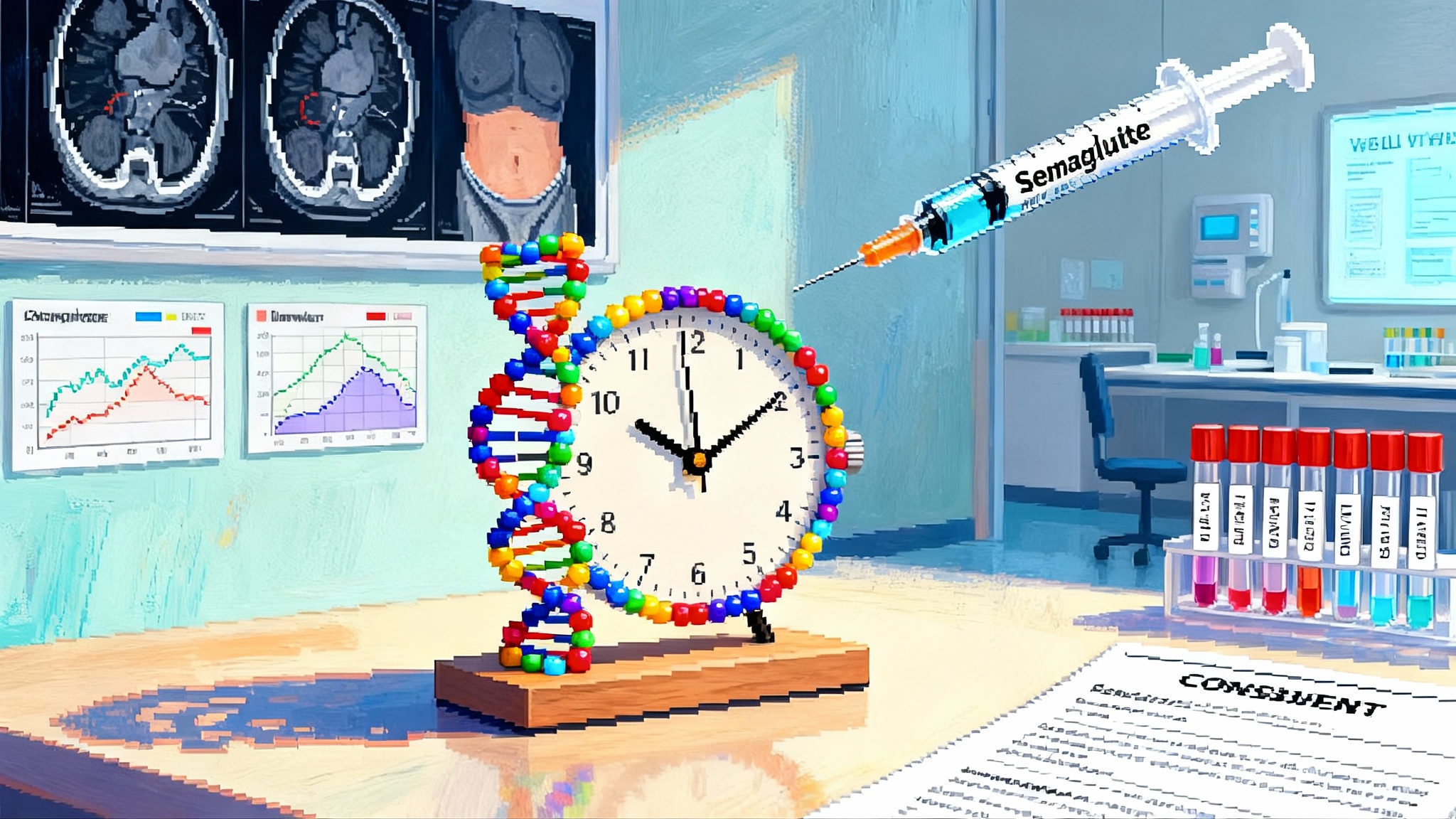
The news: a clock signal worth attention
In July 2025, researchers published a secondary analysis of a randomized, double-blind, placebo-controlled trial of semaglutide in people with HIV-associated lipohypertrophy. Over 32 weeks, the semaglutide group showed consistent improvements on several DNA methylation epigenetic clocks. Depending on the clock, the estimated biological age shifted younger by roughly 1 to 5 years, and the pace of aging slowed by about 9 percent. The work is a preprint, not yet peer reviewed, but it is the first randomized-trial-based signal that a glucagon-like peptide 1 drug might bend validated aging biomarkers in humans. See the study via this 2025 semaglutide epigenetic clock analysis.
Two details matter for interpreting this signal. First, the epigenetic analysis is post hoc. The original trial tested semaglutide to reduce visceral fat in a specific population and the methylation work came later on stored samples. Second, the trial used a weekly 1.0 milligram dose and included 45 semaglutide and 39 placebo participants in the epigenetic subset, which is modest in size. Even with those caveats, the directionality and consistency across multiple clocks make this result notable and worth stress testing.
What an epigenetic clock win means
Epigenetic clocks estimate biological age from patterns of DNA methylation in blood or other tissues. Think of methylation sites as tiny sticky notes on DNA that influence whether genes are read loudly or quietly. With age, the pattern of these sticky notes drifts. Clocks capture that drift and turn it into a number that correlates with health risks such as mortality, cardiovascular events, and frailty. For the broader biomarker context, see SenNet’s 2025 biomarker atlas.
In the new analysis, semaglutide improved several widely used measures:
- GrimAge and PhenoAge moved younger in the treatment group.
- DunedinPACE slowed by about 0.09 units, translating to roughly a 9 percent slower pace of aging.
- A multi-omic clock and a transposable-element-focused clock also shifted younger.
- An Intrinsic Capacity clock did not change, a useful boundary on the effect and a reminder that not all aging dimensions move together.
If clocks are like a dashboard, these readings say the engine ran cooler with semaglutide during the trial period. That is encouraging because these biomarkers have been linked to outcomes we care about. It also aligns with other signals tied to glucagon-like peptide 1 drugs, such as reductions in inflammation markers and shifts in body composition that reduce visceral fat. For comparison with other inflammation-directed strategies, see necroptosis blockers and inflammaging.
What it does not prove
Clocks are surrogates. A younger-looking methylation pattern is not the same as a longer life or more healthy years. This result does not prove that semaglutide extends lifespan, prevents dementia, or compresses morbidity. Key cautions include:
- Post hoc analysis. The methylation work was not a pre-specified primary endpoint. That invites bias and demands replication in trials that declare aging biomarkers ahead of time.
- Specific population. These were adults with HIV-associated lipohypertrophy, a group with distinctive inflammatory and metabolic profiles. Results could differ in the general population.
- Weight loss as mediator. Semaglutide reliably reduces visceral fat. Weight loss and the resulting drop in chronic inflammation can shift methylation patterns. The mechanistic question remains whether changes are downstream of fat loss or reflect more direct glucagon-like peptide 1 signaling.
- Tissue and depth. The clocks were measured in blood. Aging is a whole-body process, and different organs age at different tempos.
- Preprint status. Peer review could adjust the analysis or interpretation.
The case for GLP-1s as mass gerotherapeutics
Gerotherapeutics target the biology of aging itself, not just one disease. One reason to take glucagon-like peptide 1 drugs seriously is that they already deliver hard outcomes beyond weight.
In 2023 the SELECT trial showed that weekly semaglutide 2.4 milligrams reduced major adverse cardiovascular events by about 20 percent in people with established cardiovascular disease who did not have diabetes. This is a gold-standard endpoint and was published in a top journal: see the SELECT cardiovascular outcomes trial. Cardiovascular aging also intersects with clonal hematopoiesis; for a primer, see CHIP clones and heart risk.
Put simply, semaglutide helps people avoid heart attacks and strokes. If aging biomarkers move in the same direction in randomized settings, it becomes credible to ask whether therapy is nudging the biology of aging in a way that tracks with real-world benefits.
What validation should look like now
To turn an epigenetic clock win into healthspan gains, three lanes of evidence should advance together.
- Hard outcomes that are aging relevant
- Time to first cardiovascular event and to recurrent events
- Renal function decline and progression to end-stage kidney disease
- Disability-adjusted life years, hospitalization days, and days at home
- Cognitive decline measured by standardized batteries and incident dementia
- All-cause mortality, acknowledging that long follow-up is needed
- Multimodal biomarker panels that triangulate biology
- DNA methylation clocks in blood and, where safe, in tissues such as adipose and muscle
- Proteomic aging signatures and glycan age scores
- Inflammation markers such as high-sensitivity C-reactive protein, interleukin 6, soluble CD163 and CD14, paired with monocyte and T cell phenotyping
- Wearable-derived physiology such as resting heart rate, heart rate variability, and cardiorespiratory fitness inferred from free-living data
- Imaging of visceral and ectopic fat by magnetic resonance imaging or low-dose computed tomography, plus dual-energy X-ray absorptiometry for lean mass
- Functional endpoints that people feel
- Six-minute walk distance, grip strength, and stair-climb time
- Patient-reported vitality and fatigue scales
- Falls, fractures, and independence in activities of daily living
A useful rule is this: a true gerotherapeutic should generate converging improvements across biomarkers, functions, and outcomes, and those improvements should outlast short-term weight loss alone.
How to design the next wave of trials
Speed matters, but so does design. Here is a practical blueprint for getting answers quickly without sacrificing rigor.
- Prospective registration of aging endpoints. Declare DNA methylation clocks, proteomic clocks, and functional tests as primary or key secondary endpoints before the first dose. Pre-specify how to adjust for weight change to separate weight-mediated from weight-independent effects.
- Factorial combination studies. Randomize participants to semaglutide and exercise in a two-by-two design. Exercise is the most reliable intervention for preserving lean mass and improving fitness. This tests whether the combination is additive or synergistic for aging biomarkers and function. A similar design could test low-dose rapalogs or acarbose, with careful safety monitoring.
- Dose sequencing and maintenance arms. Many people reach a weight plateau after 6 to 12 months. Compare continued full dose with maintenance dosing and with guided tapering, and include a planned discontinuation sub-study to see whether biomarker gains persist or fade when the drug stops.
- Tissue sub-studies. In a subset willing to undergo procedures, collect adipose and muscle biopsies to measure methylation, proteomics, and mitochondrial function directly in tissues that drive metabolic health. Pair with brain imaging and cognitive testing to evaluate neurobiological effects.
- Inclusive recruitment. Enroll across age, sex, ancestry, and income. Include groups at higher risk of lean mass loss, such as older adults, and those with limited access to exercise resources.
- Pragmatic yet precise. Run pragmatic trials in health systems and employer clinics so that results generalize, but anchor them with a deep phenotyping core in a subset for mechanism.
What payers can do to accelerate real healthspan gains
Payers have levers that research alone does not. They can transform a weight-loss wave into healthspan gains by reshaping incentives.
- Value-based contracts with aging-relevant outcomes. Tie a portion of payment for glucagon-like peptide 1 drugs to improvements in composite outcomes such as days at home, reduced cardiovascular events, and preserved kidney function over two to three years. Require a biomarker panel at baseline and at one year to build a learning system without penalizing individual clinicians.
- Cover muscle preservation as standard of care. Reimburse supervised resistance training, protein counseling, and creatine where appropriate. Pay for dual-energy X-ray absorptiometry at baseline and 12 months in high-risk members to track lean mass, not just weight.
- Fund combination programs, not pills alone. Bundle semaglutide with validated exercise and behavioral coaching and with digital tools that nudge activity and sleep. Cover the time of exercise professionals and dietitians.
- Mandate follow-up after discontinuation. Since many members will stop due to cost or side effects, pay for three to six months of structured off-ramp care to minimize weight regain and deconditioning.
- Encourage employer and Medicare Advantage pilots. These settings can randomize benefits at the plan level, test coverage models head to head, and publish outcomes.
For clinicians and patients now
Today’s takeaway is both optimistic and grounded.
- If a patient qualifies for semaglutide based on obesity or cardiometabolic disease, the decision can be anchored in hard outcomes such as cardiovascular risk reduction. That is independent of any anti-aging promise.
- The early epigenetic signal is a reason to measure more, not to market more. If you are using glucagon-like peptide 1 drugs in eligible patients, aim for comprehensive care: resistance training two to three times per week, adequate dietary protein, sleep support, and early management of gastrointestinal side effects.
- Track what matters. When possible, add waist circumference, grip strength, a simple step test, and a few blood markers of inflammation at baseline and six to twelve months. These are inexpensive and informative.
- Be clear about limits. No clock change means guaranteed extra years. The goal is to align lifestyle, medication, and monitoring so that biological risk and lived function move in the same direction.
What could go wrong if we get the story wrong
- Overgeneralization from a specific cohort. Results in people with HIV-associated lipohypertrophy may not extend to everyone.
- Lean mass loss. Calorie deficit and appetite suppression can reduce muscle if not actively countered, especially in older adults.
- Access and adherence. High costs, supply constraints, and side effects can drive mid-course abandonment.
- Surrogate misfire. If methylation clocks move but hard outcomes do not, we are chasing the wrong target.
A playbook to turn a weight-loss wave into healthspan gains
- Researchers: pre-register aging endpoints, measure across tissues, and analyze both weight-mediated and weight-independent effects.
- Health systems: build pragmatic combination programs that pair semaglutide with exercise and nutrition, and publish outcomes.
- Payers: fund resistance training and off-ramp care, and tie payments to days at home and preserved function.
- Companies: sponsor factorial trials with exercise and with carefully chosen pathway modulators such as rapalogs, and report tissue effects.
- Regulators: support qualification of composite aging biomarker panels as secondary endpoints and encourage post-marketing evidence plans that include function.
- Employers: pilot benefit designs that pay for performance on mobility, not just weight.
- Patients: if you are eligible and choose to start, add strength training, protein, and sleep to your weekly routine and talk with your clinician about a maintenance plan.
The bottom line
The 2025 clock result is a real signal, not a final verdict. We have a medicine that reduces heart attacks and strokes and now appears to nudge multiple aging biomarkers. That combination makes semaglutide a leading candidate to become the first mass-market gerotherapeutic. Whether it earns that title will depend on what we do next. If researchers declare aging endpoints up front, if trials test smart combinations with exercise and targeted pathway modulators, and if payers fund muscle preservation and persistence, we can turn biomarker movement into extra good years lived in better health. The clocks have started to move. Our job is to make sure life moves with them.