Necroptosis Blockers Enter Trials to Tame Inflammaging
A Financial Times scoop on LinkGevity’s necrosis‑blocking combo just put regulated necrosis on the geroscience map. Here is why stopping injury‑triggered cell death could cool inflammaging, where first wins may arrive, and how to measure them fast.
Breaking: regulated necrosis steps onto the geroscience stage
Last week’s Financial Times coverage of LinkGevity’s plan to test a necrosis‑blocking drug combination made a quiet biology term feel like a market signal. The piece framed a potent idea: if you can stop cells from dying in the most inflammatory way possible, you can cool chronic smoldering inflammation as we age. In other words, target regulated necrosis to blunt inflammaging. That report, start‑up takes aim at ageing, marked a shift from preclinical promise to human trials.
The target is the necroptosis pathway. Think of a fire alarm that, when pulled, shatters the windows and sprays burning embers into the street. That is necroptosis. When certain death signals hit a cell that cannot execute clean apoptosis, a kinase relay involving receptor‑interacting protein kinase 1, receptor‑interacting protein kinase 3, and mixed lineage kinase domain‑like protein, abbreviated RIPK1, RIPK3, and MLKL, triggers a dramatic end. MLKL punches holes in the membrane, the cell bursts, and its contents spill out as danger signals. Those danger signals invite immune cells to the scene and raise local cytokines. Good for clearing infections or dead tissue in an acute injury. Bad when it loops for months and years, seeding inflammaging across many organs.
Geroscience has chased many upstream causes of aging. Necroptosis sits closer to the sparks that ignite sterile inflammation each time tissue is nicked by ischemia, toxins, mechanical stress, or misfolded proteins. That is why trialists are taking it seriously. Block the shattering end of cell death and you may prevent repeated surges of damage signals that reset immunity to angry.
What exactly are we trying to block?
The necroptosis sequence looks like this. Under certain stress signals, RIPK1 forms a complex with RIPK3. They phosphorylate each other, creating a platform that phosphorylates MLKL. Phosphorylated MLKL migrates to the membrane and forms pores. The cell swells and ruptures. This is regulated necrosis. It is not the tidy packaging of apoptosis. It is a loud, pro‑inflammatory exit.
Drug developers can intervene at three places. Inhibit RIPK1 to stop the first switch. Inhibit RIPK3 to short the relay. Inhibit MLKL to prevent pore formation. So far, small molecules that inhibit RIPK1 have the most human data. That matters because geroscience needs near‑term tools that are already de‑risked in people.
From bench to bedside: what the current human data already say
Multiple companies have run first‑in‑human and early patient studies of oral RIPK1 inhibitors. GlaxoSmithKline took GSK2982772 into healthy volunteers and several inflammatory indications. In the first‑in‑human study, the drug showed high target engagement of RIPK1 in blood at doses that were generally well tolerated, providing the core safety and pharmacology package that enables experimental medicine trials. Those data established that an oral small molecule can safely and reliably hit RIPK1 in humans, a prerequisite for mechanistic trials in aging‑related disease. See safety, dose response, and target occupancy details, which exceeded 90 percent at higher doses, in the GSK2982772 first‑in‑human report.
Denali Therapeutics and Sanofi followed with two complementary molecules. SAR443820, also known as DNL788, was designed to cross the blood brain barrier and has been tested in neurodegeneration. SAR443122, also known as DNL758 or eclitasertib, is peripherally restricted and has been tested in cutaneous lupus erythematosus and ulcerative colitis. Results have been mixed on efficacy in mid‑stage trials of neurodegeneration, which tells us two things. First, pathway biology is likely valid, because pharmacology and safety have held up across programs. Second, indication choice and endpoint selection will determine whether necroptosis blockers look like meaningful anti‑inflammaging medicines or just interesting tools.
Add Eli Lilly’s collaboration with Rigel on ocadusertib, previously R552, now in Phase 2a in rheumatoid arthritis, and you have a small but real portfolio of clinical‑stage RIPK1 inhibitors. This matters for geroscience not because rheumatoid arthritis is an aging disease, but because it gives a ready‑to‑repurpose list of molecules with human safety, dose, and biomarker playbooks. For context on biomarker strategy, see our aging biomarkers playbook.
Why stopping the burst could cool inflammaging across organs
Every time a tissue is injured, some cells die neatly and others die messily. The messy exits pour out damage‑associated molecular patterns, often abbreviated as DAMPs, that act like flares. This is useful once or twice. With age, micro‑injuries accumulate and repair becomes slower. The repeated flares keep innate immunity primed. Cytokines trickle upward. Senescent cells receive danger signals and secrete more pro‑inflammatory factors. The loop does not need an external pathogen. It is self‑fueling.
Block the necroptosis switch and three good things can happen.
- Fewer DAMPs are released at each injury event, so local cytokines fall.
- Neighboring cells see less danger signaling and are less likely to become dysfunctional or senescent.
- Tissue‑resident immune cells spend more time in surveillance and less in alarm, which preserves function.
You can think of RIPK1 inhibitors as surge protectors. They do not prevent every cause of damage, but they stop the worst spikes from frying the circuitry. This complements our vascular first longevity playbook.
Trial‑ready indications that can read out in 12 to 18 months
The fastest path to show benefit pairs a high‑burden condition where regulated necrosis is prominent with biomarkers that move quickly. Three stand out.
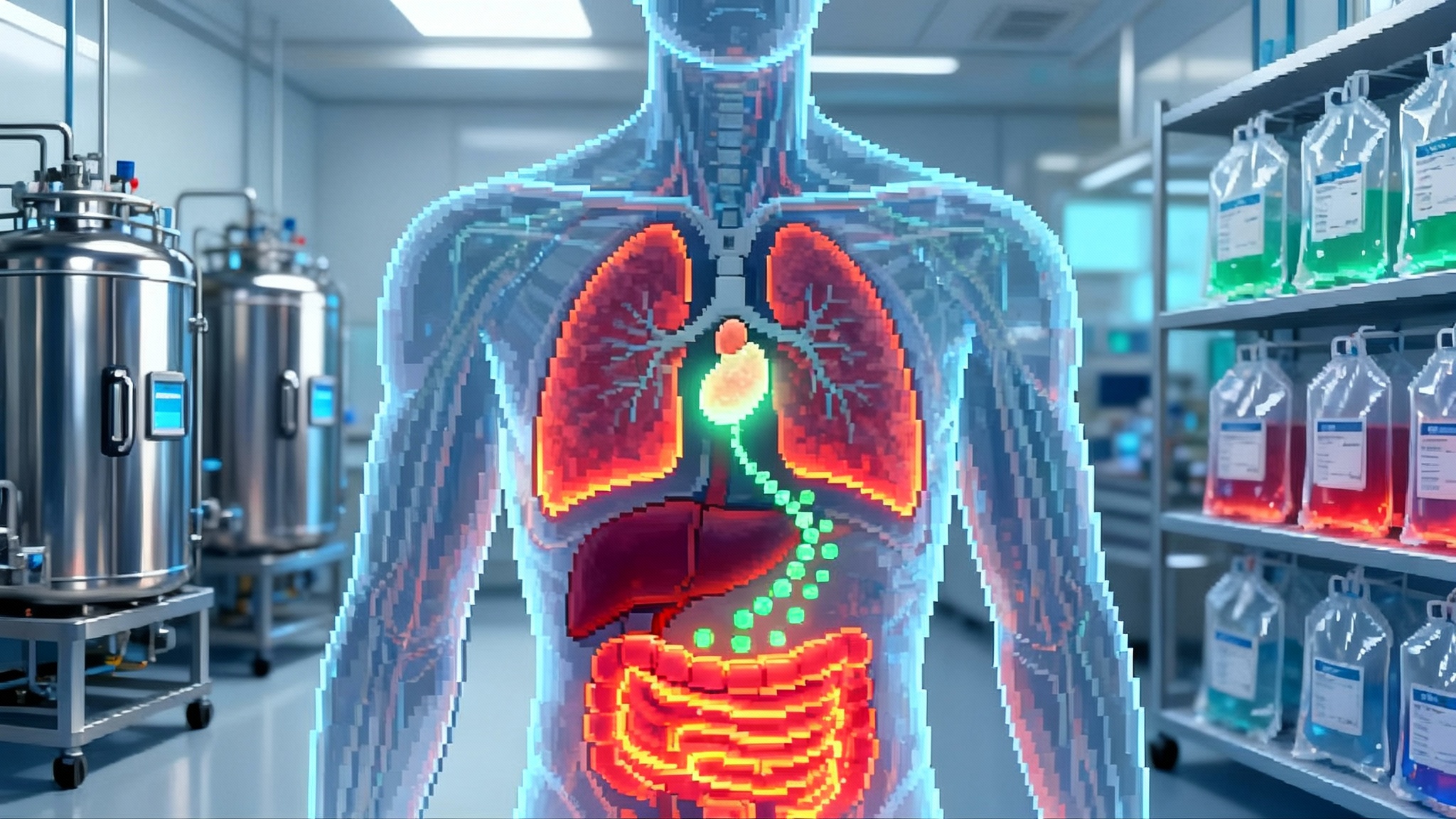
- Metabolic dysfunction associated steatotic liver disease, often shortened to MASLD, and its inflammatory stage, steatohepatitis.
- Rationale: Hepatocyte injury and ballooning are tightly linked to cell death and sterile inflammation. Necroptosis is activated in experimental models of steatohepatitis, and blocking RIPK1 reduces inflammatory signaling and fibrosis progression.
- Trial design: Twelve to eighteen months, oral peripherally restricted RIPK1 inhibitor. Enrich for patients with high baseline alanine aminotransferase and aspartate aminotransferase, elevated extracellular matrix biomarkers such as PRO‑C3, and transient elastography or magnetic resonance elastography evidence of fibrosis stages F2 to F3. Avoid rapidly progressing cirrhosis where other pathologies dominate.
- Endpoints and early signals: Quick signals at 12 to 24 weeks in alanine aminotransferase and aspartate aminotransferase. Structural signals at 6 to 12 months in magnetic resonance proton density fat fraction and magnetic resonance elastography. Fibrosis biology via Enhanced Liver Fibrosis score and hyaluronic acid. Mechanistic signal via phosphorylated MLKL staining in optional biopsies and circulating cytokeratin‑18 M65, a cell death marker.
- Neurodegeneration in subgroups with high inflammatory tone, such as early amyotrophic lateral sclerosis or transdiagnostic cohorts with elevated plasma neurofilament light chain.
- Rationale: RIPK1 activity is implicated in microglial activation and neuron‑glia cross talk. Brain‑penetrant RIPK1 inhibitors can test whether blunting necroptosis and inflammatory signaling lowers axonal injury.
- Trial design: Twelve months, central nervous system penetrant inhibitor in a biomarker‑rich cohort that allows smaller sample sizes. Enrich for high baseline neurofilament light chain and evidence of neuroinflammation on fluid biomarkers. Combine with digital function measures to increase sensitivity.
- Endpoints and early signals: Plasma and serum neurofilament light chain decline within 3 to 6 months. Slower decline on function scales is supportive but may require larger samples. Optional cerebrospinal fluid biomarkers of inflammation add depth.
- Frailty and acute‑on‑chronic injury recovery in older adults.
- Rationale: Frailty amplifies the hit from routine injuries. A fall or hospitalization can trigger a cascade of muscle loss, immune dysfunction, and slow recovery. Regulated necrosis likely contributes to the inflammatory surge after tissue damage.
- Trial design: Twelve months in older adults with recent hospitalization for a noninfectious injury or surgery. Pair drug with standardized rehabilitation.
- Endpoints and early signals: Four‑meter gait speed, grip strength, and the Short Physical Performance Battery at 3 and 6 months. Falls, readmissions, and patient‑reported recovery. Inflammation panels, including interleukin‑6 and C‑reactive protein, to test whether the drug blunts the post‑injury inflammatory rise.
Biomarkers that can show benefit fast
Aging programs live or die on whether they can show change inside a funding cycle. Necroptosis blockers have several measurable, mechanistic readouts. For assay selection and validation, our aging biomarkers playbook outlines practical choices.
- Direct pathway markers: Phosphorylated MLKL in tissue biopsies or immunoassays of circulating MLKL‑containing vesicles. Phosphorylation state changes within weeks if the pathway is blocked.
- Cell death surrogates: Cytokeratin‑18 fragments in liver disease. Cell‑free DNA with necrotic signatures in acute injury settings.
- Axonal injury: Neurofilament light chain in plasma or serum for neurodegeneration.
- Systemic inflammation: Interleukin‑6 and C‑reactive protein for frailty and recovery trials.
- Organ function: Alanine aminotransferase, aspartate aminotransferase, and Enhanced Liver Fibrosis score for liver. Quantitative imaging by magnetic resonance proton density fat fraction and magnetic resonance elastography for steatosis and stiffness.
The combination of a mechanistic signal plus an organ function improvement is the right standard. A drop in phosphorylated MLKL without liver benefit is interesting biology. A drop in alanine aminotransferase without a necroptosis marker risks being off target. The pair is convincing.
A repurposing pipeline you can run now
Investors and translational groups do not need to wait for bespoke geroscience molecules. A practical playbook looks like this.
- Peripheral RIPK1 inhibitors. Candidates with clean safety and dose ranges can be redeployed in MASLD or inflammatory recovery studies. Peripherally restricted molecules avoid brain side effects and fit liver or frailty settings.
- Central nervous system penetrant RIPK1 inhibitors. Despite mixed mid‑stage readouts in diseases like amyotrophic lateral sclerosis and multiple sclerosis, the biomarker data and safety experience support targeted, mechanistic trials in neuroinflammation with enrichment and shorter endpoints.
- Additional mechanism pairs. Some injuries activate both apoptosis and necroptosis. Combination regimens that pair a necroptosis blocker with a senolytic in a staggered design could test whether preventing new inflammatory surges while clearing pro‑inflammatory senescent cells yields additive benefits. Start small with safety and biomarker cohorts.
On the company map, the current cast includes LinkGevity pushing a necrosis‑blocking combination, Sanofi and Denali with central and peripheral RIPK1 programs, GlaxoSmithKline with the earliest human target‑engagement package, and Eli Lilly with Rigel’s ocadusertib in Phase 2a. That is enough diversity to design multiple proof‑of‑concept trials in parallel.
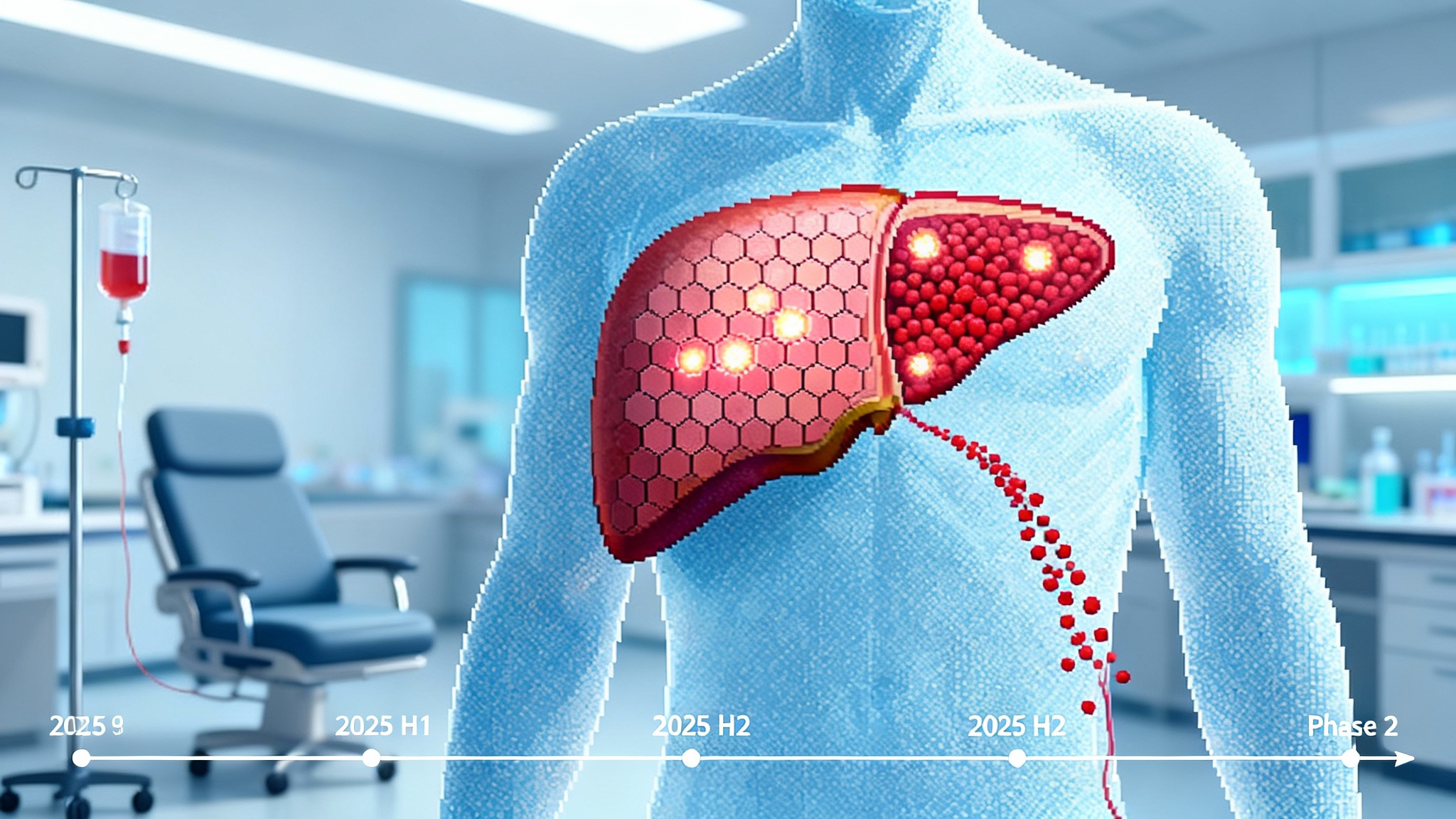
What would positive readouts in 2026 look like?
By mid‑2026, a credible success pattern would include three elements.
- Liver inflammaging: A randomized Phase 2a in MASLD showing a meaningful alanine aminotransferase and aspartate aminotransferase drop by 12 weeks that persists to 24 weeks, a clear improvement in Enhanced Liver Fibrosis score by 6 to 12 months, and concordant decreases in cytokeratin‑18 M65 and phosphorylated MLKL staining in optional biopsies. Imaging by magnetic resonance proton density fat fraction would strengthen the case by showing less liver fat, even if fibrosis change is still early.
- Neuroinflammation: A biomarker‑enriched cohort with a sustained 15 to 25 percent reduction in plasma neurofilament light chain over 6 to 12 months versus placebo, plus signs of slower decline on a functional scale appropriate to the disease. Safety must look clean and consistent with prior studies.
- Frailty recovery: Faster rebound in gait speed and grip strength at 3 and 6 months after injury or surgery, fewer readmissions, and lower interleukin‑6 peaks after the initial insult.
Regulators will not approve on these alone, but this pattern would unlock larger confirmatory trials and make necroptosis blockade a serious complement to mainstream anti‑inflammatory strategies.
Complement, not competitor, to senolytics
Senolytics aim to remove senescent cells that secrete pro‑inflammatory factors. Necroptosis blockers aim to prevent inflammatory surges that can create and feed senescence. They are different tools. In practice, necroptosis blockers could make senolytics safer and more durable by reducing the new waves of tissue damage that repopulate the senescent pool after each injury. In settings like MASLD, a period of necroptosis blockade around weight loss or metabolic interventions could prevent rebound inflammation while the organ resets. This sits alongside immune recalibration strategies such as engineered Tregs for immunity.
For trialists, the action is straightforward. Do not test necroptosis blockers as universal anti‑aging pills. Pair them with high‑risk windows where injury is frequent and measurable, and layer them with lifestyle or disease‑modifying therapies where the biology is complementary.
Risks and how to derisk early
- Efficacy heterogeneity. Not every inflammatory disease is driven by necroptosis. Use pathway markers, like phosphorylated MLKL, to confirm that your cohort is on target before randomization.
- Infection risk. Any anti‑inflammatory strategy can blunt host defense. Start with populations where the benefit of dampening injury‑triggered inflammation is highest and monitor infections rigorously.
- Endpoint sensitivity. Function scales in neurodegeneration are slow and noisy. Lead with neurofilament light chain and digital measures while you accumulate power for clinical endpoints.
- Redundancy in cell death. Cells can switch between apoptosis and necroptosis. Predefine rescue analyses that account for compensatory pathways, and consider sequential combination designs in later studies.
The near‑term opportunity
Geroscience needs pragmatic wins. Necroptosis blockade offers a path that is mechanistically crisp, clinically measurable within a year, and already supported by human pharmacology. The Financial Times story put a name and a near‑term plan to the idea. The rest is execution. Pick indications where injury is frequent and the readouts are fast. Pair mechanistic biomarkers with organ function metrics. Treat necroptosis blockers as surge protectors that complement, not replace, other aging interventions.
If 2026 arrives with convincing biomarker‑plus‑function stories in liver disease, neuroinflammation, and frailty recovery, necroptosis blockers will have earned a place in the anti‑inflammaging toolkit. Not a silver bullet. A new class with a clear job: stop the worst cellular exits so tissues can heal cleanly and age more slowly.