The CMV Vaccine That Could Rewire How We Age in 2025
Moderna's pivotal cytomegalovirus vaccine readout in 2025 could do more than protect babies. If it works, it may slow immune aging, improve responses to other shots, and open a path to longevity vaccines against latent viruses.
Breaking: the first pivotal test for longevity vaccines
A quiet but consequential milestone is coming in 2025. Moderna expects pivotal efficacy data from its Phase 3 cytomegalovirus vaccine, mRNA-1647, a study now fully enrolled and continuing to accrue cases in women of childbearing age. The company has said it remains blinded and anticipates final efficacy results in 2025. That single readout will not only decide the fate of the first modern cytomegalovirus vaccine; it will also test a simple but powerful idea. If you block or blunt a ubiquitous, lifelong viral passenger, can you slow immune aging and improve how the body responds to every other vaccine it sees? See the company’s overview in this Moderna 2025 pipeline update.
The near-term win is obvious. Preventing primary cytomegalovirus infection in women before pregnancy could reduce congenital infection and its consequences. The long game is bolder. It imagines a new category of interventions, sometimes called longevity vaccines, aimed at chronic, latent viruses that never truly leave the body. In that vision, cytomegalovirus comes first, followed by Epstein-Barr virus and herpes simplex virus. Together they shape immunity for decades. If we can manage them, we may be able to add resilience to the immune system itself.
CMV 101: why this quiet passenger matters
Cytomegalovirus is everywhere. Most infections are silent, then the virus sets up lifelong residence in immune cells and tissues. It reactivates periodically, usually without symptoms. CMV matters for newborns because primary infection during pregnancy can transmit to the fetus and cause a range of problems, most notably hearing loss. In the United States, about one in 200 babies is born with congenital CMV and about one in five of those children will have long-term health issues. These are the baseline facts public health agencies use today. You can confirm them in the CDC congenital CMV facts.
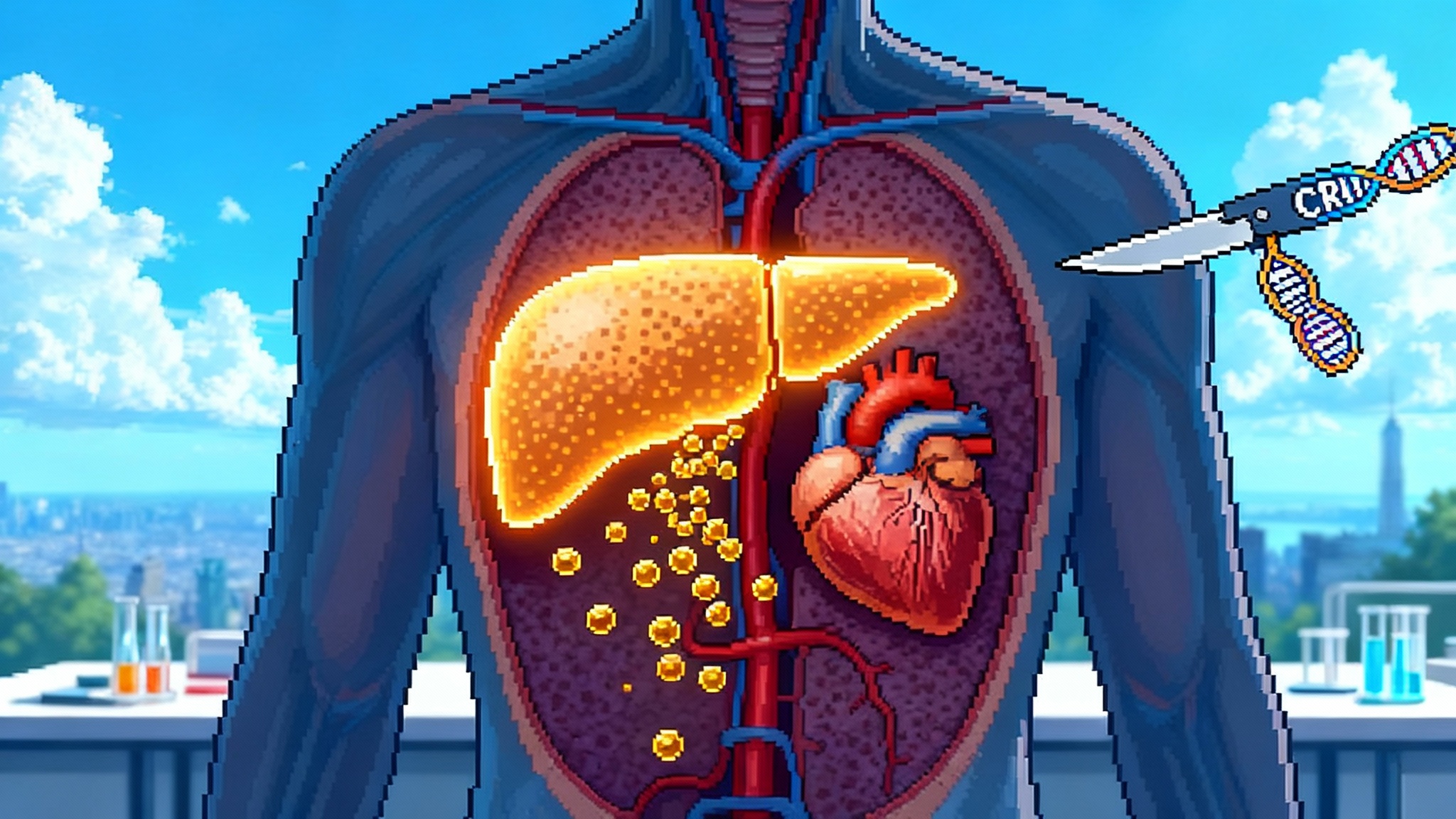
That maternal and newborn story is compelling on its own. But CMV is also relevant for adult health. Decades of research show that CMV steadily shapes T cells, the workhorse cells that coordinate immune responses. Some people develop large armies of CMV-specific T cells that expand and stick around. This expanding footprint is sometimes called memory inflation. As the years pass, those cells can occupy significant space in the immune repertoire. The question is whether that crowding meaningfully reduces the ability to respond to new threats or vaccines. The answer is nuanced, but the pattern points in one direction: CMV often pushes the immune system toward an older profile.
How CMV ages the immune system, in plain terms
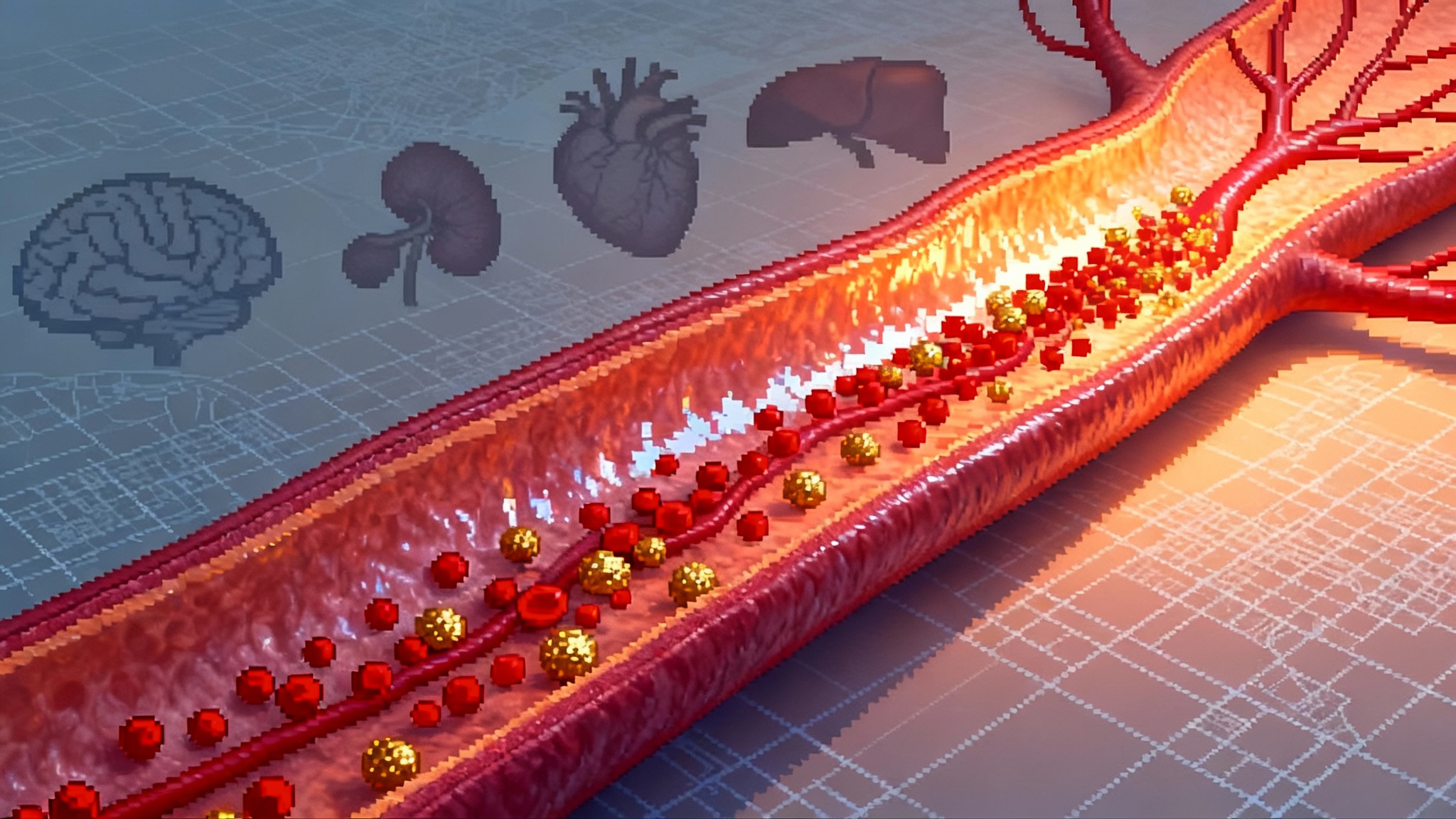
Think of the immune system as a city with a limited number of trained responders. You want a healthy mix of rookies ready to learn new threats and veterans with years of experience. Over time, CMV recruits so many veterans to patrol a single neighborhood that the city starts to look unbalanced. The rookie class shrinks, and the same crews handle the same routes day after day. The city still functions, but it reacts more slowly to new emergencies.
Here is what that looks like biologically:
- Memory inflation: CMV-specific T cells expand massively and occupy a larger share of the total T cell pool. Many are highly differentiated and less flexible.
- Ratio shifts: Older adults with CMV positivity often show altered CD4 to CD8 ratios and more late-stage effector cells. This profile, sometimes part of an immune risk signature, correlates with frailty and worse outcomes in some cohorts.
- Repertoire crowding: The immune system seems to accommodate large CMV-specific clones. Even when total diversity is preserved, a disproportionate share of attention remains fixed on CMV antigens.
- Vaccine response drag: Studies in older adults have found that CMV serostatus can be associated with weaker responses to some vaccines in some settings, though results are mixed. Mechanistic work suggests the effect depends on age, preexisting immunity, and the type of vaccine.
This is not a doom story. Many CMV-positive people live long and healthy lives. The point is probabilistic. Over decades, CMV can push the immune system toward a less adaptable state, and that can matter in the presence of other stressors like aging, chronic disease, or chemotherapy. If a vaccine could prevent or limit CMV in adolescence or adulthood, we would have a lever to test whether that drift can be slowed.
What a positive Phase 3 would mean, beyond maternal health
The pivotal CMV trial evaluates prevention of primary infection in women of childbearing age. If efficacy is robust and safety is clean, the immediate impact will be maternal and newborn health. But success opens a bigger door. Regulators and advisory groups could consider the following expansions:
- Preconception immunization: Integrate CMV vaccination into routine care for adolescents and young adults, particularly those with frequent contact with toddlers, who shed virus at high levels. This mirrors how some health systems approach immunization for rubella or varicella before pregnancy.
- Occupational risk programs: Offer CMV vaccination to childcare workers, neonatal staff, and others with high exposure risk. Clear employer programs can drive uptake.
- Transplant and oncology pathways: Evaluate vaccination in CMV-negative recipients on immunosuppressive regimens. This is a different risk profile and would need dedicated trials, but the logic is strong.
- Adult immunization schedule: If the vaccine shows durable protection and favorable cost effectiveness, the Advisory Committee on Immunization Practices could one day review broader adult use beyond maternal indications. That would take more data, including real-world effectiveness and duration of protection.
Three scenarios if the efficacy hits
- High efficacy with clean safety
- What it looks like: Vaccine efficacy at or above the level typically needed to change behavior, coupled with favorable safety data and a clear manufacturing plan.
- Policy implications: Rapid push for preconception and occupational programs. Expect payer coverage within months of recommendation. Hospital systems could bundle CMV with routine visits for young adults.
- Longevity angle: Immediate interest in adult trials that track immune aging markers over time. Expect partnerships between vaccine makers, academic immunologists, and health systems to launch these cohorts.
- Moderate efficacy or short-lived protection
- What it looks like: Meaningful but partial protection, or protection that wanes within a couple of years.
- Policy implications: Still valuable for maternal health, potentially paired with behavior guidance for pregnancy. Booster strategies would be explored.
- Longevity angle: Adult immunization might focus on those with high exposure or medical risk. Research programs would test whether even partial control modifies immune aging metrics.
- Low efficacy or safety signal
- What it looks like: Effect seen only in subgroups, or safety imbalances that limit broad use.
- Policy implications: Indication narrows. Investment shifts to next-generation antigens or adjuvants.
- Longevity angle: The broader concept survives, but the path shifts toward other latent viruses or combination strategies.
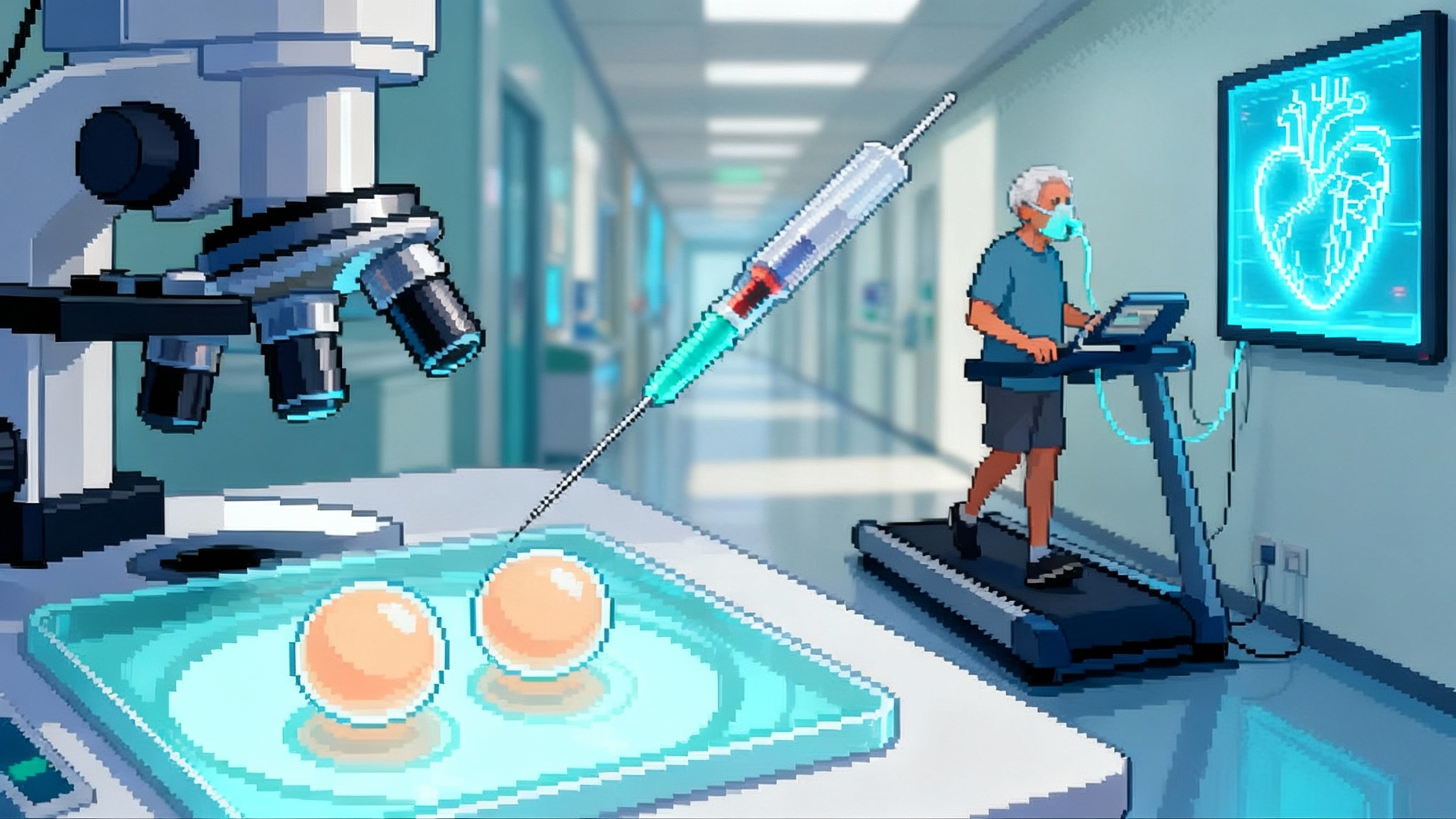
How blocking CMV could enhance other vaccines
If CMV occupies immune bandwidth, reducing its load could move the needle on responses to unrelated vaccines. The practical test is simple. Enroll adults, vaccinate against CMV or give placebo, then administer a standard vaccine such as influenza, shingles, or COVID after a fixed interval. Measure antibody titers and, crucially, T cell responses; follow people for real outcomes like respiratory hospitalizations over winter. Layer on digital cohorts to track sick-day rates and symptom duration. For broader context on restoring immune tone, see how engineered Tregs are being explored in our piece on engineered Tregs for immune rejuvenation.
Signals to look for:
- Higher seroconversion rates or neutralization titers after seasonal vaccines.
- Broader T cell responses, with more targets recognized and more cytokine production in vitro.
- Fewer breakthrough infections or shorter illness duration during a surveillance season.
- More favorable immune age markers, such as a higher naive T cell fraction or a healthier CD4 to CD8 balance.
If any of these move in the right direction, the field will have a quantitative case that CMV control is not just about one disease. It is about raising the floor for the immune system.
The CMV to EBV to HSV pipeline: from pregnancy to prevention of chronic disease
Cytomegalovirus is first in line, but it will not be alone for long. Epstein-Barr virus is linked to infectious mononucleosis and to lifelong risks that include certain cancers and autoimmune conditions. Vaccine programs are already in human trials, both industry and government. Herpes simplex virus type 2 drives recurrent genital lesions and increases the risk of human immunodeficiency virus acquisition. Prophylactic and therapeutic vaccines are progressing in early clinical studies.
Why line them up in this order? Two reasons. First, clinical endpoints are clear. For CMV, it is primary infection and congenital outcomes. For Epstein-Barr virus, it is prevention of mononucleosis and reduction in viral load; over years, researchers can track whether incidence of multiple sclerosis or certain cancers shifts in vaccinated populations. For herpes simplex virus, it is fewer outbreaks, less shedding, and better quality of life. Second, the biology is shared. All are herpesviruses that establish latency, reactivate under stress, and shape immune tone over time. Managing their reactivation and transmission could have compounding benefits.
A near-term policy checklist if CMV hits in 2025
- Clinical guidance: Create a preconception immunization pathway that integrates CMV with routine adolescent and young adult care. Include clear recommendations for those who work with toddlers.
- Coverage: Encourage payers to cover vaccine plus screening visits with zero cost sharing in the approved population.
- Communication: Update patient-facing materials in obstetrics, pediatrics, and primary care. People should understand that CMV is common, often silent, and preventable.
- Data: Stand up pragmatic trials inside health systems to measure impacts on immunization responses and real outcomes. Use standardized labs and shared protocols.
- State action: Pair vaccination with growing newborn screening programs for congenital CMV where feasible, and invest in follow-up services like early hearing checks.
Measuring healthspan gains, not just infection rates
A longevity vaccine needs longevity endpoints. We cannot wait 30 years for mortality curves to separate. Instead, build a battery of near-term markers and outcomes that together reflect immune resiliency. For methods, see our trial-grade biomarker playbook.
- Immune profiling: Track naive and memory T cell proportions, CD4 to CD8 ratios, T cell receptor diversity, and exhaustion markers. Standardize panels across sites.
- Vaccine challenge: Use influenza, shingles, and COVID boosters as functional challenges. Compare humoral and cellular responses in vaccinated versus control groups.
- Clinical events: Monitor respiratory hospitalizations, shingles cases, and days of work or school missed.
- Inflammation scores: Follow markers like high-sensitivity C-reactive protein and interleukin-6 over time.
- Frailty and function: Add short physical performance batteries and patient-reported outcomes to trials.
This mixed battery lets teams see movement within 6 to 24 months. If the composite trends are positive and durable, that is a credible early signal that healthspan has shifted.
A five-year roadmap to turn latent-virus control into policy
Year 1
- If the Phase 3 readout is positive, move quickly to publish the full dataset. Launch preconception and occupational programs in pilot health systems. Begin immune-profiling cohorts in adults.
Year 2
- Expand payer coverage and integrate reminders into electronic health records. Coadminister CMV with other routine vaccines where safe. Launch head-to-head studies of vaccine response in CMV-vaccinated versus unvaccinated adults.
Year 3
- Publish pooled immune-aging results and real-world effectiveness for maternal outcomes. If signals are strong, seek review for broader adult recommendations.
Years 4 to 5
- If durability wanes, implement boosters with data behind timing. Fold in Epstein-Barr virus vaccine trials that use similar immune-age endpoints. Begin combination strategies that address multiple latent viruses.
What could go wrong, and how to handle it
- Uncertain effect on immune aging: It is possible that preventing CMV in adulthood will not noticeably improve responses to other vaccines in the near term. Plan trials with enough power to detect small but meaningful changes, and preregister composite endpoints.
- Durability questions: If protection wanes quickly, consider booster strategies and test them prospectively.
- Equity gaps: Young adults who would benefit most may be least likely to access care. Partner with employers, colleges, and community clinics to deliver vaccination where people are.
- Risk communication: CMV is common and usually silent, which can lead to complacency. Use clear, specific messaging that focuses on newborn protection and potential immune benefits for adults, without overclaiming.
How health systems and companies can act now
- Health systems: Identify CMV-related touchpoints in primary care, obstetrics, pediatrics, and employee health. Build order sets that combine counseling, vaccination when eligible, and scheduling for follow-up shots.
- Employers and schools: Offer vaccination at orientation for staff in childcare, education, and healthcare. Pair with education about hygiene that reduces CMV spread.
- Payers: Preapprove coverage for the indicated populations and set up claims logic to minimize denials. Support outcomes research that ties vaccination to reduced downstream costs.
- Researchers: Harmonize immune-aging panels and share protocols. Register multi-site studies that look the same across cities so results can be pooled. For a template on converting enthusiasm into rigorous trials, see our piece on turning plasma exchange into testable biology.
- Vaccine makers: Publish immunogenicity detail, especially cell-mediated responses, and share durability data early. If efficacy is moderate, explore adjuvants, antigen mixes, or schedules that enhance breadth.
The bigger picture: aging as an infectious-burden problem
Longevity has many levers, from exercise to blood pressure control. Infectious burden is one we can now address with precision. If CMV vaccination reduces congenital disease and nudges adult immunity toward a younger profile, it reframes vaccination as infrastructure for healthy aging. Epstein-Barr virus and herpes simplex virus would extend that infrastructure, first by preventing their own harms, and then possibly by lowering the chronic viral load that shapes immunity over time.
The 2025 CMV readout will not settle the entire debate. But it will give us the first real chance to test a hopeful hypothesis with modern tools and clear endpoints. If the data are strong, the next step is not to declare victory. It is to build the measurement scaffolding that proves the immune system itself can age more slowly when latent viruses are held in check. That is a worthy experiment for the decade ahead.