Turning Plasma Exchange Hype Into Testable Human Biology
A rigorous 2025 randomized trial reported multi-omics shifts and aging-clock improvements after therapeutic plasma exchange, especially with IVIG. Here is what that signal means for safety, cadence, costs, and how clinics can test it without hype.
The breakthrough signal that changed the conversation
For years, plasma exchange circled the fringes of longevity culture, buoyed by rodent parabiosis studies and sunk by the hype of young plasma transfusions. In May 2025, a small but high-quality human trial changed the tone. In a single-blind, randomized, placebo-controlled study of adults over 50, investigators compared several schedules of therapeutic plasma exchange, with and without intravenous immunoglobulin, and tracked thousands of molecular features across the epigenome, proteome, metabolome, glycome, and immune cell composition. The headline result was simple and provocative: treatment arms showed statistically significant shifts on multiple biological aging clocks, with the biweekly plasma exchange plus immunoglobulin arm producing the largest effect sizes while maintaining an acceptable safety profile. See the peer-reviewed report in Aging Cell: May 2025 TPE multi-omics trial.
This is not proof that plasma exchange extends lifespan. It is an early human signal that a clinical apheresis procedure can reproducibly nudge composite aging biomarkers in the direction of youthfulness. The trial’s size was modest, which increases uncertainty, and the follow-up window was limited. Yet in the world of longevity therapeutics, where many claims rest on uncontrolled case series or animal data, the presence of randomization, a placebo control, and multi-omic readouts is a meaningful step forward.
From parabiosis imagery to human biology
Heterochronic parabiosis in mice attached the bloodstreams of young and old animals and produced striking tissue changes. That picture created a cultural shortcut: youthful blood must be a tonic. In reality, the human translation leans less on adding something mystical and more on removing and replacing some of what accumulates.
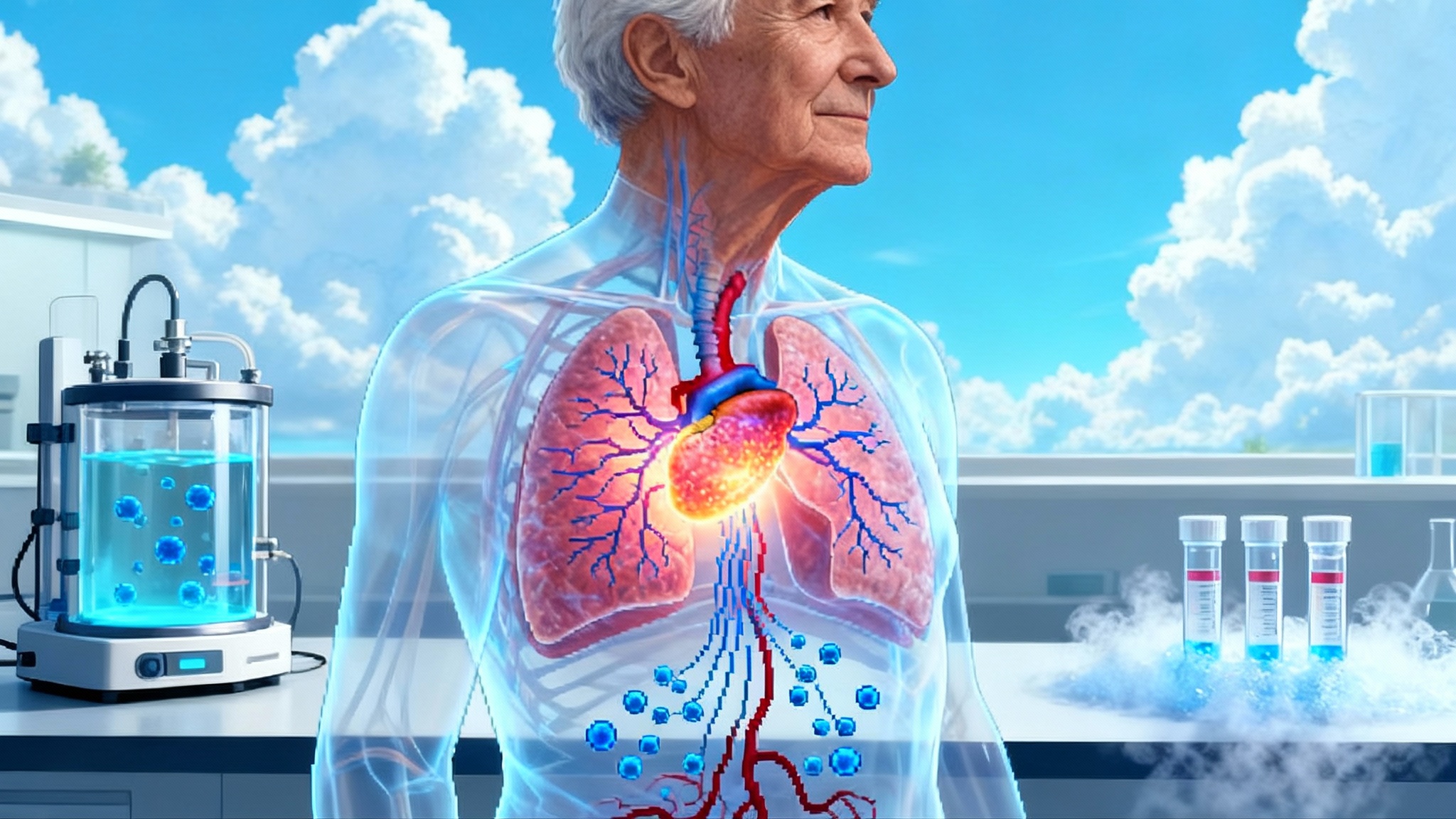
Therapeutic plasma exchange separates and discards a portion of circulating plasma, then returns cells suspended in a replacement fluid, typically albumin. Think of the bloodstream as a busy harbor. Over decades, debris accumulates in the water: inflammatory proteins, autoantibodies, senescence-associated factors, oxidized lipids, and protein fragments. TPE is the harbor’s dredging and refilling. You lower the concentration of pro-inflammatory cargo, you reduce pathological autoantibodies, and you restore binding capacity with fresh albumin that can mop up toxins and altered metabolites. When intravenous immunoglobulin is added, you also introduce a standardized stock of antibodies that can neutralize pathogens and modulate immune signaling. These immune shifts echo the case for naive T cells as longevity's edge.
In the 2025 trial, this shows up as a coordinated pattern across molecular layers. Pro-inflammatory proteins drop, epigenetic clocks recalibrate, immune cell proportions shift toward a profile seen in younger cohorts, and senescence-linked signatures soften. The mechanism is not a single switch but a network effect created by dilution plus replacement.
What TPE is and is not
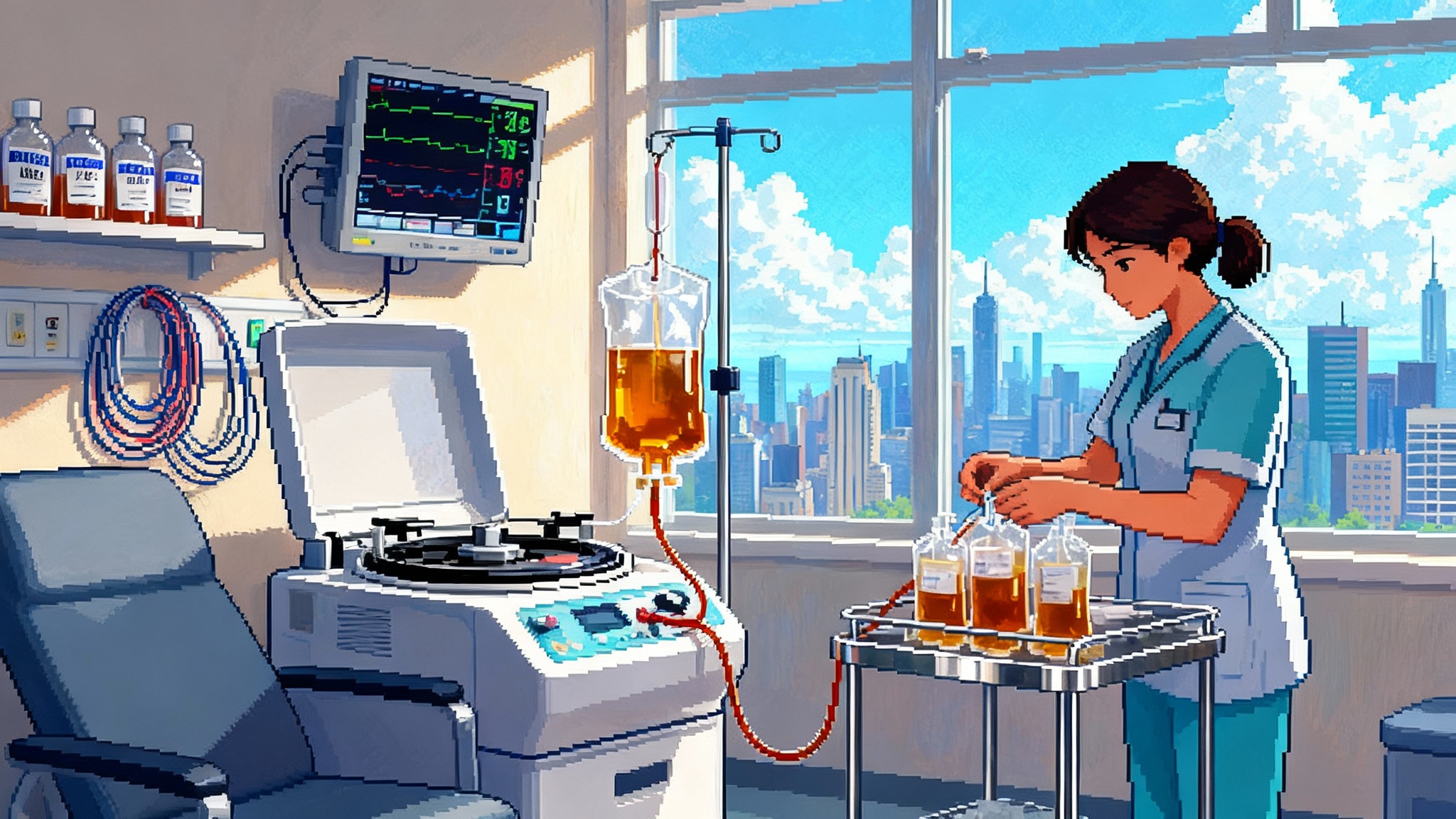
TPE is a regulated medical procedure. A nurse or physician places an intravenous line, often in a peripheral vein but sometimes through a central line if access is difficult. An apheresis device cycles blood through a separator that diverts plasma into a collection bag while returning red cells and other cellular components with replacement fluid. Each session typically processes one to one and a half times the patient’s plasma volume. The procedure takes about two hours in outpatient settings.
It is not the same as routine plasma donation. It is not a young-plasma transfusion. It is not a stem cell treatment. The most apt comparison is to a system reset by removing a fraction of the circulating milieu and replacing it with a clean buffer.
A second anchor: disease outcomes in Alzheimer’s
If longevity biomarkers sound abstract, consider clinical outcomes. The AMBAR program tested plasma exchange with albumin, and in some arms alternating with immunoglobulin, in patients with mild to moderate Alzheimer’s disease. The phase 2b or 3 randomized trial reported less decline on functional and cognitive measures over 14 months in treated groups, with the largest benefit seen in moderate disease. This is not a cure and the effect sizes are moderate, but it is disease-relevant evidence that repeated plasma exchange can translate into measurable clinical trajectories. See details of design, endpoints, and subgroup effects: AMBAR randomized Alzheimer's trial.
Why mention Alzheimer’s in a longevity story? Because the path from biomarker to meaningful healthspan runs through disease endpoints. If plasma exchange slows disability in a neurodegenerative condition when delivered on a structured schedule, that triangulates the biology and informs cadence in other age-linked conditions.
How the procedure likely works, in plain language
- Proteome dilution: Many age-associated molecules act like crowd noise that never stops. Lower the volume, and cells can hear regulatory signals again. TPE turns down that noise by physically removing a portion of the circulating proteins that drive chronic inflammation and tissue stress.
- Albumin replacement: Albumin is a sponge and a shuttle. Fresh albumin binds fatty acids, toxins, and oxidized metabolites, and it helps normalize oncotic pressure. By swapping in new albumin, TPE refreshes the bloodstream’s sponge and shuttle system.
- Immune recalibration: IVIG is a curated library of antibodies from many donors. It can neutralize infectious antigens, dampen autoantibody activity, and modulate Fc receptor signaling on immune cells. In practice, that can stabilize the transient hypogammaglobulinemia that follows TPE and steer the immune network toward a less inflamed set point.
- Senescence-associated factors: Senescent cells secrete a stew known as the senescence-associated secretory phenotype. While TPE does not delete senescent cells, it dilutes the circulating components of that stew and may lower the systemic inflammatory tone that sustains senescent cell activity. That aligns with work on targeted senescence strategies such as in vivo CAR-T for senescence.
These mechanisms are additive. Dilution lowers harmful inputs. Replacement adds binding and buffering capacity. Immunoglobulin adds immune modulation. The net effect is a short window where homeostatic systems can reset.
Practical cadence: what a reasonable schedule might look like
Trial arms in 2025 tested both biweekly and monthly sessions, with the combination of biweekly exchange and immunoglobulin showing the strongest multi-omics changes during the active phase. The AMBAR program in Alzheimer’s used an intensive period of weekly exchange, followed by monthly maintenance for a year. Taken together, a practical starting framework for longevity clinics and research programs looks like this:
- Induction: Three to six sessions over 6 to 10 weeks. This is enough to meaningfully lower circulating inflammatory and autoimmune factors and to push multi-omics markers in the right direction without overcommitting.
- Reassessment: Recheck a predefined biomarker panel at 4 to 6 weeks after the final induction session. Look for movement in proteomic inflammation scores, immune cell distribution, and a small set of pre-specified epigenetic clocks. Avoid testing dozens of clocks. Pick two or three that have shown sensitivity in interventional studies and have good technical reproducibility, such as those responsive in rapamycin’s first human longevity trial.
- Maintenance: If biomarkers and symptoms improved, schedule one session every 6 to 12 weeks for 6 months, then reassess. The principle is to space treatments to the longest interval that preserves gains, not to stack them as often as possible.
- Combination rules: If a patient starts with low immunoglobulin levels or is at higher risk for infections, consider adding immunoglobulin at least for induction. If immunoglobulin levels recover and infections are not an issue, many patients may continue with albumin alone for maintenance.
Safety in real clinics, not just in papers
Most sessions are uncomplicated. Common issues include transient drops in blood pressure, lightheadedness, and tingling around the mouth or hands related to citrate anticoagulation. These are managed by adjusting the machine’s settings and giving calcium during the session. It is routine to see temporary changes in laboratory values right after exchange: lower fibrinogen and immunoglobulins, lower albumin before replacement, and shifts in platelets and calcium that settle in the following days.
Real risks exist. Central lines increase the chance of infection and thrombosis, so skilled peripheral access is preferred when possible. Repeated exchanges without immunoglobulin can leave some people vulnerable to infections until levels rebound, especially if they start out low. Bleeding risk is small but present if coagulation factors dip. Careful screening, on-session monitoring, and day-after follow-up calls reduce these risks. The 2025 trial reported acceptable safety with few discontinuations, and larger disease trials such as AMBAR describe an overall manageable safety profile when procedures are done by experienced teams.
What this means operationally: pick high-volume outpatient apheresis centers with modern devices such as Spectra Optia from Terumo BCT or Fresenius COM.TEC, insist on protocols for calcium management and immunoglobulin monitoring, and track adverse events in a shared registry so that clinics can learn from one another in near real time.
Cost, coverage, and realistic budgets
Prices vary widely by region and setting. In the United States in 2025, a typical outpatient plasma exchange session is often billed in the low thousands of dollars per treatment for the device, nursing time, and disposables. Albumin replacement adds several hundred dollars per session. Immunoglobulin is the major cost driver. Depending on dose and payer contracts, a single immunoglobulin infusion can add several thousand dollars to well over ten thousand dollars.
For a patient paying cash in a boutique setting, a three-session induction with albumin alone might run from the mid four figures to the low five figures. The same induction with immunoglobulin can cost a multiple of that. Insurance coverage is usually confined to approved indications like certain autoimmune neurological disorders. Longevity-focused use sits outside those categories today, which is why the field needs stronger evidence and smarter payment models.
Clinics can make programs more affordable by standardizing dosing, using peripheral access to avoid line placements, batching lab draws, and using maintenance sessions sparingly and guided by biomarkers rather than by the calendar.
Who seems to benefit most so far
The 2025 multi-omics study reported a pattern seen in many interventions that target chronic inflammation. Individuals with worse baseline health signals showed the largest improvements. Higher baseline bilirubin or glucose, signs of liver stress, and pro-inflammatory proteomic profiles predicted bigger shifts in aging biomarkers after induction. Healthy older adults did show favorable movement, but effect sizes were smaller. This suggests two practical use cases: a restorative protocol for people with high inflammatory burden or auto-immunity, and a lighter maintenance protocol for healthier adults who want to keep low-grade inflammation in check.
What to measure, and how to measure it well
Longevity clinics often fall into the trap of measuring everything. That dilutes statistical power and drains budgets. A better approach is to pre-register a small panel and stick to it. For plasma exchange, a rational panel includes:
- Proteomic inflammation score built from a short list of cytokines and complement factors.
- A senescence-associated subset that is analytically reliable.
- Two epigenetic clocks with published interventional sensitivity and good test-retest reliability.
- Immune cell composition by flow cytometry, focusing on naive versus memory T cells and myeloid subsets.
- Safety labs such as immunoglobulin levels, fibrinogen, albumin, calcium, and a standard chemistry panel.
Collect at baseline, mid-induction, four to six weeks after induction, and then every three to four months if maintenance is used. Use the same lab methods, at the same time of day, with the same fasting state, to minimize noise.
The acceleration roadmap
This is how plasma exchange moves from boutique to credible healthspan therapy.
- Biomarker qualification with clinical anchoring.
- Predefine a core composite endpoint that integrates an epigenetic clock, a proteomic inflammation score, and an immune age metric. Pre-register the endpoint and lock the analysis plan before enrollment.
- Cross-validate the composite against clinical anchors that matter in aging: gait speed, grip strength, balance, and validated symptom scales for fatigue and cognitive complaints. The goal is not only a younger clock but a stronger, steadier person.
- Standardize timing: collect on a common schedule relative to exchanges to avoid artifacts from acute shifts.
- Adaptive randomized controlled trials.
- Use multi-arm, multi-stage designs that compare albumin-only versus albumin-plus-immunoglobulin, and biweekly versus monthly cadence, with response-adaptive randomization. If one arm clearly underperforms at interim analysis, drop it and reallocate.
- Stratify by baseline inflammatory burden and immunoglobulin level since these features predict response. This avoids washing out an effect by mixing high-burden and low-burden participants.
- Bridge biomarkers to endpoints. Keep objective measures like six-minute walk test, short physical performance battery, and patient-reported outcomes in the platform so you can detect clinically meaningful change, not just molecular drift.
- Real-world registries with common data elements.
- Build a simple, vendor-agnostic registry that every apheresis center can use in parallel with routine care. Capture demographics, indications, access route, exchange volume, replacement fluid, adverse events, and the biomarker panel described above.
- Implement automated data quality checks and consent workflows. Use standard coding so that health systems can contribute data without bespoke engineering.
- Publish rolling safety summaries and quarterly effectiveness snapshots. That transparency will curb hype, surface risks early, and help payers evaluate coverage pilots for high-risk groups.
What clinics can do now without overpromising
- Start with a pilot protocol anchored to the evidence: three to six induction exchanges over two months, albumin replacement for all, immunoglobulin added if baseline levels are low or infection risk is high, followed by a data-driven decision on maintenance.
- Use a predefined biomarker panel and track a small set of physical performance measures. Show patients their trajectory on a single page rather than a stack of dashboards.
- Join or help seed a registry. Even a small center can contribute valuable insights if data are standardized and shared.
- Be honest about cost and uncertainty. For many people, the marginal benefit will not justify the price until stronger outcome data arrive. That is not a failure. It is how careful medicine advances.
The bottom line
The longevity world has needed a way to move from rodent metaphors to human mechanisms. The 2025 multi-omics trial provides that first rung, showing that therapeutic plasma exchange, particularly when combined with immunoglobulin, can push multiple biological aging markers in the right direction in a controlled setting. Alzheimer’s data show that sustained schedules can influence clinical trajectories in at least one age-linked disease. The science is still early, the costs are material, and safety needs disciplined protocols. Yet the path forward is clear. Define what success looks like. Test cadence and components with adaptive trials. Build transparent registries that make every session count twice, once for a patient and once for the field. That is how plasma exchange moves from boutique procedure to a credible tool for extending healthspan, one measured step at a time.