The Thymus Revival: Naive T Cells as Longevity's Edge
The overlooked thymus is taking center stage. In 2025, fresh data, a pediatric approval, and government funding converged to make naive T cell restoration a credible strategy to harden immunity, improve vaccine responses, and extend healthy years.
A quiet organ steps into the spotlight
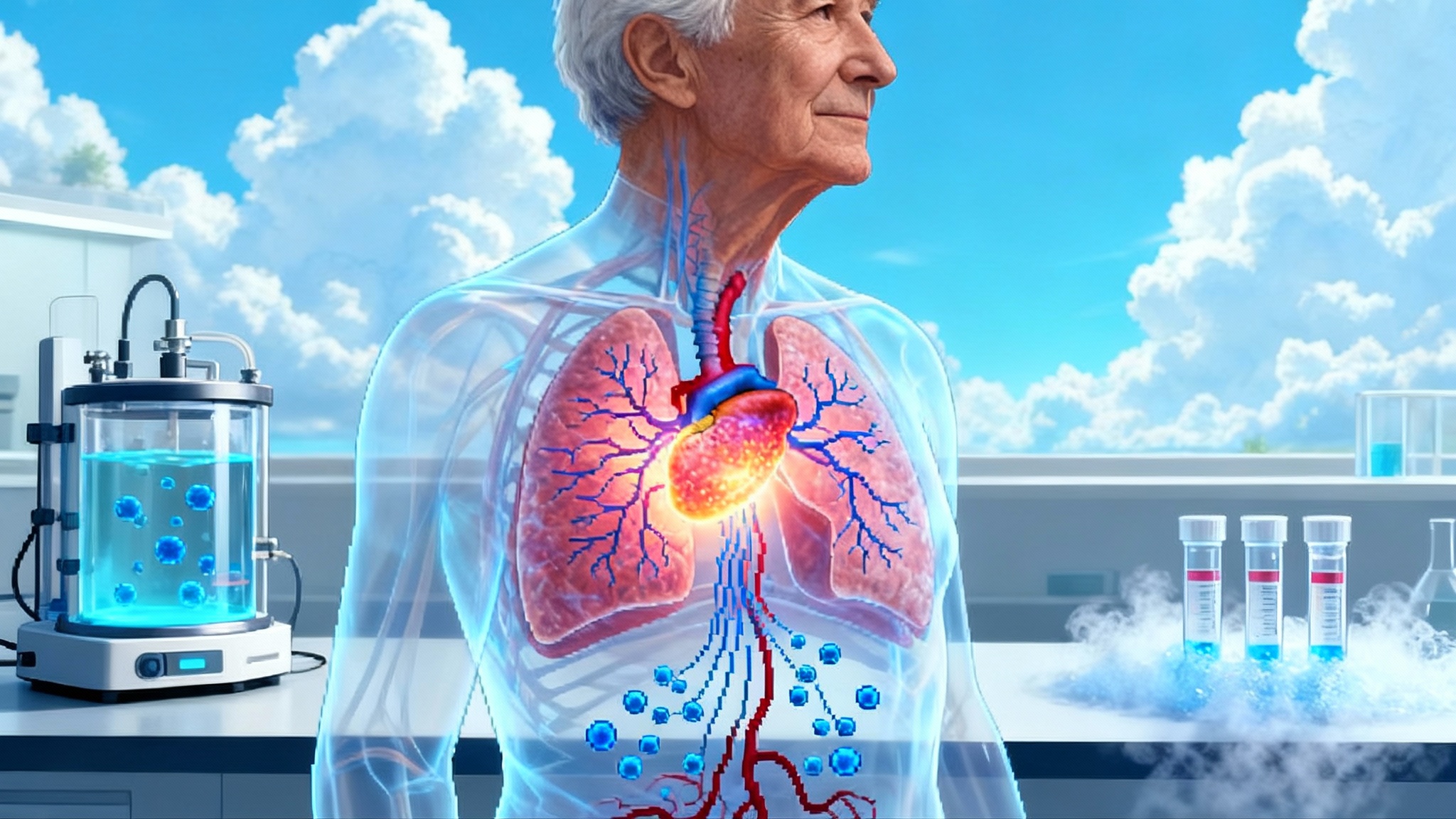
The thymus has spent decades as the wallflower of human biology. It is small, hidden behind the breastbone, and steadily shrinks with age. Yet it trains fresh T cells that recognize new pathogens and respond to vaccines. When thymic output dwindles, we lean on memory cells from earlier in life, which is why older adults often respond poorly to novel infections and boosters. If you want to improve immune resilience at scale, you target the factory for new recruits, not just the veterans.
That idea is no longer theoretical. In 2025, a run of milestones has repositioned thymus repair and regeneration as a high return on investment strategy for longevity and immune health. Four signals make this year different:
- TRIIM-X, the follow-on to the small 2019 thymus regeneration study, is slated to complete primary endpoints by December 2025.
- City of Hope researchers mapped a regenerative circuit in which recirculating regulatory T cells deliver amphiregulin signals that repair damaged thymus tissue in preclinical models.
- Smart Immune announced ProTcell presentations at ThymUS and the International Society for Cell and Gene Therapy, highlighting how ex vivo T cell progenitors can rearm immunity via the patient’s own thymus.
- The United States government has committed money and attention. The Food and Drug Administration created a precedent by approving RETHYMIC, a cultured thymus tissue for children with congenital athymia, and the Advanced Research Projects Agency for Health is funding iPSC-derived thymic cell programs aimed at scalable adult therapies.
Together, these threads suggest a practical outcome: a path from rare pediatric surgery to off-the-shelf cells and shots on goal for adults.
Why naive T cells are the keystone
Think of your immune system as a city’s fire department. Memory T cells are seasoned crews who know familiar addresses. Naive T cells are new recruits who can handle fires the city has never seen. With age, the academy closes its doors. Fewer recruits graduate, and response times suffer. Infectious disease risks rise, vaccine responses wobble, and surveillance against early tumor cells weakens.
Restoring naive output does three things that matter clinically and economically:
-
It improves responsiveness to first encounters. That reduces severe infections and hospital days in older adults and in patients recovering from chemotherapy, transplantation, or chronic viral infections.
-
It supports broader T cell receptor diversity. Diversity is a hedge against pathogen evolution and a complement to antibody-focused strategies.
-
It enables safer and more durable cell therapies. Progenitors trained inside a patient’s thymus are less likely to exhaust or misfire than mature cells pushed ex vivo to the edge of their capabilities.
Regulatory ground is already broken
In 2021, the U.S. Food and Drug Administration approved RETHYMIC, a one-time implant of cultured thymus tissue for children born without a thymus. It is a surgical product with strict controls, but it established how regulators evaluate a therapy whose job is to generate new naive T cells in humans. The approval dossier clarifies what counts as success and what to monitor for risk, including slow time to immune protection and the potential for graft-versus-host disease. It is the first proof that rebuilding thymic function can be judged, regulated, and reimbursed at all. FDA approval of RETHYMIC.
Why this matters now: a pediatric precedent lowers the friction for adult programs that use very different modalities. RETHYMIC relies on donor tissue and surgery. The emerging wave aims for scalable cells or drugs that activate the body’s own regenerative programs. Regulators have a conceptual template for endpoints and risk, and companies have a reference case to design around.
The 2025 turn: four signals that changed the risk calculus
1) TRIIM-X approaches its readout
TRIIM-X extends the original TRIIM study that combined growth hormone with metformin and dehydroepiandrosterone in midlife adults. The original trial reported signals of thymic fat loss, rising naive T cell markers, and a shift in epigenetic clocks. TRIIM-X, a randomized study launched in 2020, is listed to complete primary endpoints by late 2025. That timing matters. Positive data, even if incremental, would validate therapeutic levers that do not require cell therapy or surgery. Negative data would sharpen focus on engineered cells and organoid approaches. Either outcome tightens strategy.
What to look for in TRIIM-X: not just imaging, but hard immune outputs like T cell receptor excision circles, shifts in naive-to-memory ratios, and functional vaccine responses.
2) City of Hope uncovers a regeneration switch
A team led by scientists affiliated with City of Hope, Memorial Sloan Kettering, and international collaborators reported in Immunity that a subset of regulatory T cells can home back to the thymus after damage and drive repair via amphiregulin. Two features elevate this beyond an interesting mouse story. First, adoptive transfer of these cells accelerated regeneration in both young and aged animals. Second, an analogous population appears in human thymus, pointing to a translational path.
Why this is actionable: amphiregulin signaling and the recirculating regulatory T cell population are specific targets. You can imagine therapies that expand these cells, deliver amphiregulin locally, or mimic the signal with a biologic, all without permanent genetic modification.
3) Progenitor T cells meet the clinic’s front door
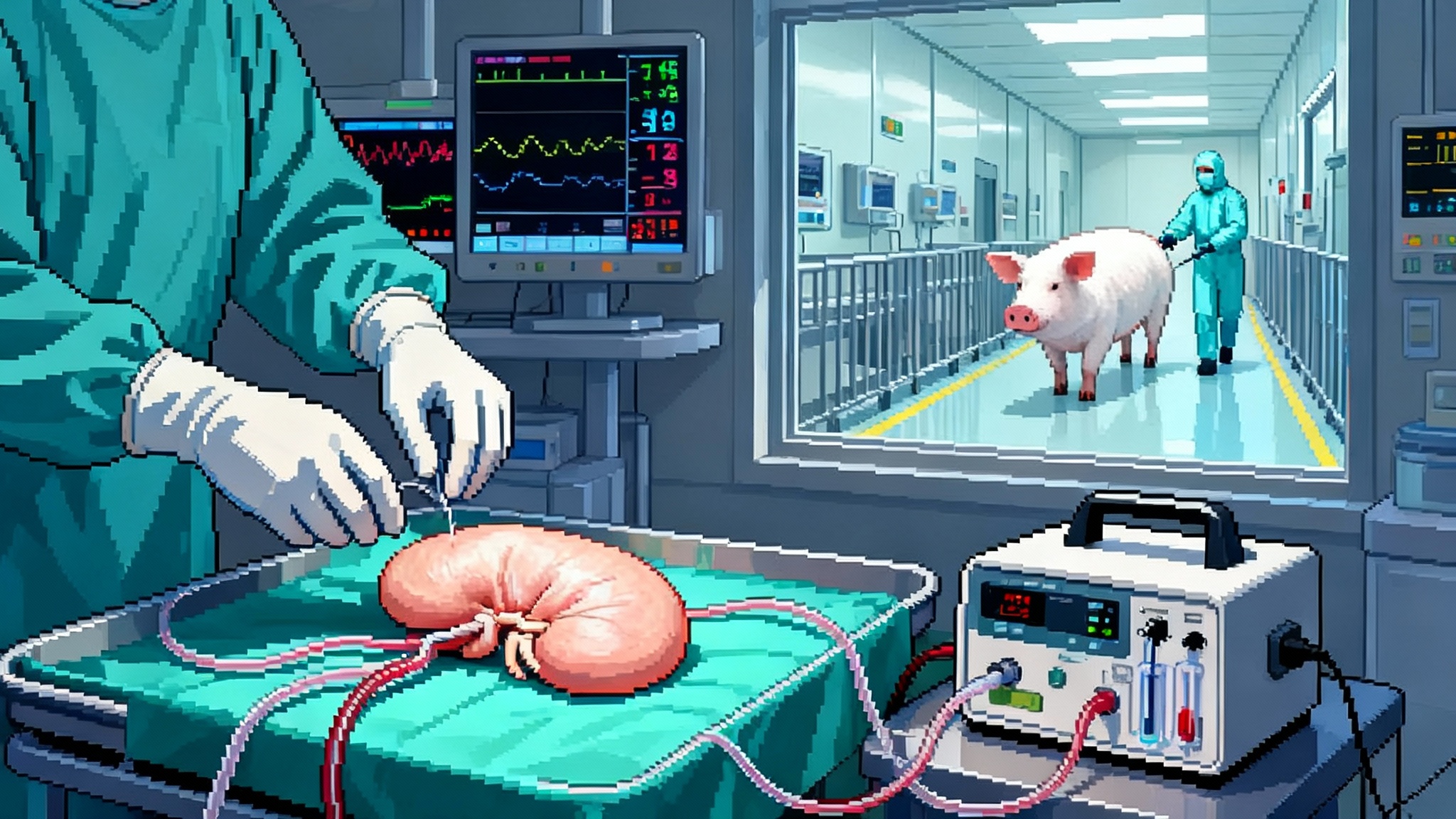
Smart Immune’s ProTcell concept is simple and practical. Instead of infusing fully formed T cells that may exhaust or mispair, deliver T cell progenitors that will complete development inside the patient’s thymus. Clinical teams then measure how quickly a durable, diverse naive repertoire appears. In transplant recipients and immune-depleted patients, that is the difference between lingering vulnerability and a return to normal life.
At this year’s ThymUS meeting and at ISCT, Smart Immune and its collaborators highlighted preclinical and early clinical data centered on faster thymic reconstitution and improved infection control after allogeneic stem cell transplantation. For a field that has long prized elegant mouse rescue experiments, seeing a standardized manufacturing platform, release criteria, and immune monitoring plan in a human therapeutic context is a meaningful step. Those playbooks echo lessons from in vivo CAR-T goes clinical.
4) Government bets on iPSC-derived thymic cells
ARPA-H, the U.S. program built to take on audacious biomedical bets, awarded up to 37 million dollars to a Thymus Rejuvenation project led by Thymmune Therapeutics. The mandate is blunt: industrialize the production of induced pluripotent stem cell derived thymic epithelial cells and show they can restore T cell development in animals, then scale toward clinical readiness. This is not a small grant to explore a niche. It is an instruction to compress timelines and solve manufacturing and potency testing early. ARPA-H funding for thymus rejuvenation.
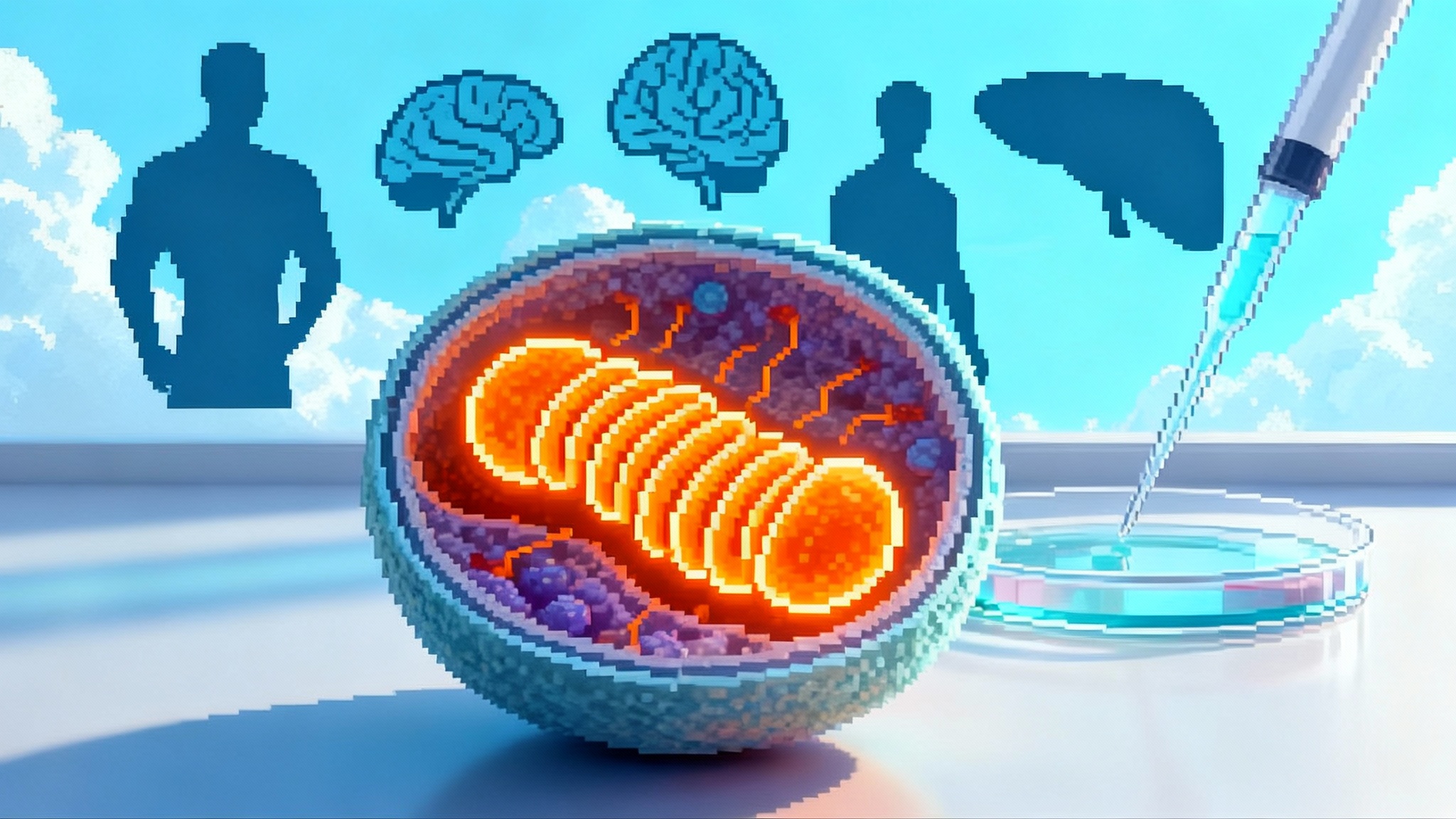
In parallel, academic groups published recipes for generating human thymic epithelial lineages from induced pluripotent stem cells and for building thymic organoids that support T cell development in vitro. These are the blueprints industry needs to convert into good manufacturing practice workflows and potency assays.
From rare pediatric surgery to scalable adult therapies
Moving from a handful of pediatric thymus implants to adult-scale immune rejuvenation hinges on three shifts:
-
Tissue to cells: donor tissue works for a rare disease but cannot scale. iPSC-derived thymic epithelial cells and ex vivo generated T cell progenitors can be expanded in bioreactors, frozen, shipped, and dosed repeatedly.
-
Episodic surgery to repeatable dosing: adults will likely need less invasive options. Two viable formats are an outpatient infusion of T cell progenitors and a minimally invasive delivery of thymic epithelial cells into a vascularized muscle or lymph node. Both must fit into oncology and infectious disease clinics.
-
Case reports to measurable population outcomes: a company cannot build a business on anecdotes. Adult programs need trials that tie thymic repair to fewer hospitalizations, better vaccine responses, and faster recovery after standard cancer regimens.
Endpoints that decide winners
If you are a regulator, payer, or investor, the following readouts separate real rejuvenation from laboratory glow:
-
TREC kinetics: T cell receptor excision circles are DNA byproducts created when T cells rearrange their receptors in the thymus. Rising signal indicates fresh thymic output. Look for increases in signal joint TRECs and favorable sj-to-DJ ratios, which reflect active recombination rather than peripheral expansion.
-
Naive T cell counts and recent thymic emigrants: track CD45RA positive, CCR7 positive naive pools, and the CD31 positive subset of naive CD4 cells that mark recent thymic emigrants.
-
TCR diversity: next generation sequencing of T cell receptor beta chains can quantify clonotype richness and evenness. Expect a broader baseline repertoire and less clonal skewing after effective therapy.
-
Functional immunity: vaccine challenge responses, controlled exposure studies when ethical, or validated correlates of protection. In oncology settings, watch rates of severe infections, time to viral clearance, and length of hospitalization.
-
Thymic structure and perfusion: imaging that shows reappearance of cortical and medullary zones is helpful but should not stand alone.
Standardizing these readouts dovetails with the broader aging biomarker race.
Manufacturing at adult scale
Immune rejuvenation will live or die on practical manufacturing. Ask these questions of any program:
-
What is the unit operation at scale? For iPSC-derived thymic epithelial cells, does the process use stirred tank bioreactors with closed harvest steps, or labor intensive plates. Closed systems and consistent shear profiles matter for cost and quality.
-
How is identity and potency defined. For thymic epithelial cells, identity should include FOXN1 and cell surface markers that distinguish cortical and medullary subsets. Potency should move beyond gene expression into functional co-culture assays that generate naive T cells and induce central tolerance markers like AIRE dependent tissue restricted antigens.
-
What is the shelf life and logistics plan. If the product cannot handle 72 hours in a shipper with dry vapor nitrogen, or if it requires bespoke on-site manipulation, it will not integrate smoothly into clinical practice.
-
For T cell progenitors, how is mispairing risk minimized and how is the maturation state controlled. Release criteria must ensure cells are committed but still competent to undergo positive and negative selection in the host thymus.
Safety as the field scales
Safety is not one concern. It is a checklist:
-
Autoimmunity: an immature or skewed thymic epithelium could impair negative selection and increase autoreactive clones. Adult programs should prospectively monitor autoantibody panels and T cell reactivity against self antigens.
-
Graft versus host disease: RETHYMIC taught us that grafted tissue and allogeneic cells can create risk. Progenitors that mature in the patient’s thymus should have lower risk than infusing allogeneic mature T cells, but monitoring and intervention plans are still essential.
-
Malignancy: any cell therapy brings a theoretical risk of transformation. Long term registries and integration site analyses are part of the cost of doing business.
-
Infection window: naive output rises over months. Programs must plan for antimicrobial prophylaxis and immunoglobulin replacement during the ramp period, just as the pediatric precedent requires.
-
Ectopic engraftment and organoid physiology: if thymic epithelial cells take root in muscle or lymph nodes, teams must track local effects on tissue architecture, perfusion, and nerve supply.
Where each approach fits
-
Small molecule and endocrine modulation: protocols that combine growth hormone, metformin, and dehydroepiandrosterone could be the fastest to deploy if TRIIM-X confirms benefit and safety. They may serve as bridge therapies or adjuncts to cell approaches, especially in midlife adults, and they rhyme with lessons from rapamycin’s first human longevity trial.
-
T cell progenitors: ProTcell style products are natural fits for post transplant settings, chronic infections that have battered T cell pools, and older adults at high risk of severe respiratory infections. Their success depends on manufacturing reliability and the health of the patient’s thymic stroma.
-
iPSC-derived thymic epithelial cells: the most scalable way to rebuild the organ’s teaching staff. Early human studies will likely focus on severe thymic deficiency and then expand into aging cohorts that show objective evidence of low thymic output and high infection burden.
What to watch next
-
TRIIM-X primary endpoint timing in late 2025. Watch for prespecified immune endpoints and not just imaging findings.
-
ThymUS and conference follow through. Presentations this spring set the table. The key is how many programs translate posters into regulated manufacturing runs and controlled trials over the next 12 months.
-
ARPA-H and NIH milestones. Expect press notes on preclinical performance thresholds for iPSC-derived thymic epithelial cells and on process scale up. A clear potency assay aligned with regulators would be a quiet breakthrough in its own right.
-
Early ProTcell clinical readouts. For hematology indications, look for time to robust T cell reconstitution, rates of cytomegalovirus and other opportunistic infections, and the breadth of T cell receptor repertoires.
-
Pediatric-to-adult regulatory harmonization. RETHYMIC’s label centers on congenital athymia. Regulators will need to clarify evidentiary standards for age-related thymic involution and for adjuvant use alongside cancer therapy.
The investment and policy angle
A high return on investment play balances impact, timing, and scalability. Thymus targeted approaches score on all three if they meet their endpoints:
-
Impact: fewer severe infections, better vaccine responses, and faster recovery after cytotoxic regimens translate into hospital days avoided and lower mortality. Those are outcomes payers value.
-
Timing: first readouts arrive in the next 6 to 18 months. The field is not waiting for a distant scientific revolution.
-
Scalability: iPSC platforms and standardized progenitor manufacturing align with large patient populations. That moves immune rejuvenation from boutique medicine to public health.
For policymakers, there is a concrete to-do list: encourage standardized immune monitoring, support comparative trials against best available care, and fund long term registries that capture autoimmune, infectious, and oncologic signals across diverse populations. For hospital systems, pilot programs that pair thymus repair with vaccination campaigns or oncology pathways can test real world value quickly.
Bottom line
The thymus will never be a glamorous organ. But in 2025 it became a practical one. A pediatric approval proved regulators will judge a therapy that builds new naive T cells. A government bet funded the scale up that adult medicine requires. Academic labs mapped the repair signals. And companies moved progenitor cells from the bench to the bedside playbook. If you care about healthier aging and resilient immunity, follow the data that show the academy for new recruits is back in business. The next year will tell us which teams can turn that promise into routine care.