Taurine’s reality check: NIH study drops biomarker hype
An NIH analysis in Science on June 5, 2025 reports that circulating taurine does not consistently track aging in humans, monkeys, or mice. We explain biomarker versus endpoint, where human trials stand, and how to read longevity claims with discipline.
The news, the nuance, and the stakes
If taurine capsules have been crowding your feed, this week brought the most important signal yet about what they can and cannot tell you. NIH scientists reported in Science on June 5, 2025 that circulating taurine is not a dependable readout of aging across species. In longitudinal blood samples from people, rhesus monkeys, and mice, taurine levels often stayed the same or even increased with age, and within-person swings were larger than any slow drift tied to aging. Associations with health measures were inconsistent. In short, low taurine in blood is not a universal signature of getting older. You can read the primary report in the June 5 Science paper.
That is a reality check for a supplement cast as a longevity lever since 2023, when animal data suggested taurine supplementation extended lifespan in mice and improved health metrics in monkeys. The new NIH work does not say taurine has no biological effects. It says taurine in your blood is not a reliable biomarker of the aging process. Those are different questions.
Biomarker ≠ endpoint
A biomarker is a measurable indicator plausibly linked to biology. An endpoint is an outcome that matters to patients and public health: walking speed, independence, fewer falls, fewer hospitalizations, survival. Biomarkers can accelerate research, but only if they meet a higher bar.
- A good biomarker moves in the right direction when risk rises and in predictable ways across time within the same person.
- It remains informative after you adjust for confounders like sex, body composition, diet, medications, and activity.
- Shifting the biomarker through an intervention should forecast meaningful changes in clinical endpoints.
Taurine hit headlines because animal supplementation shifted diverse molecular hallmarks and, in mice, increased lifespan. That does not automatically make a single taurine blood measurement a dependable compass for biological age in humans.
For a sense of how the field is trying to tighten links between markers and outcomes, see our coverage of cross-organ PER data pivot and the plasma exchange human data.
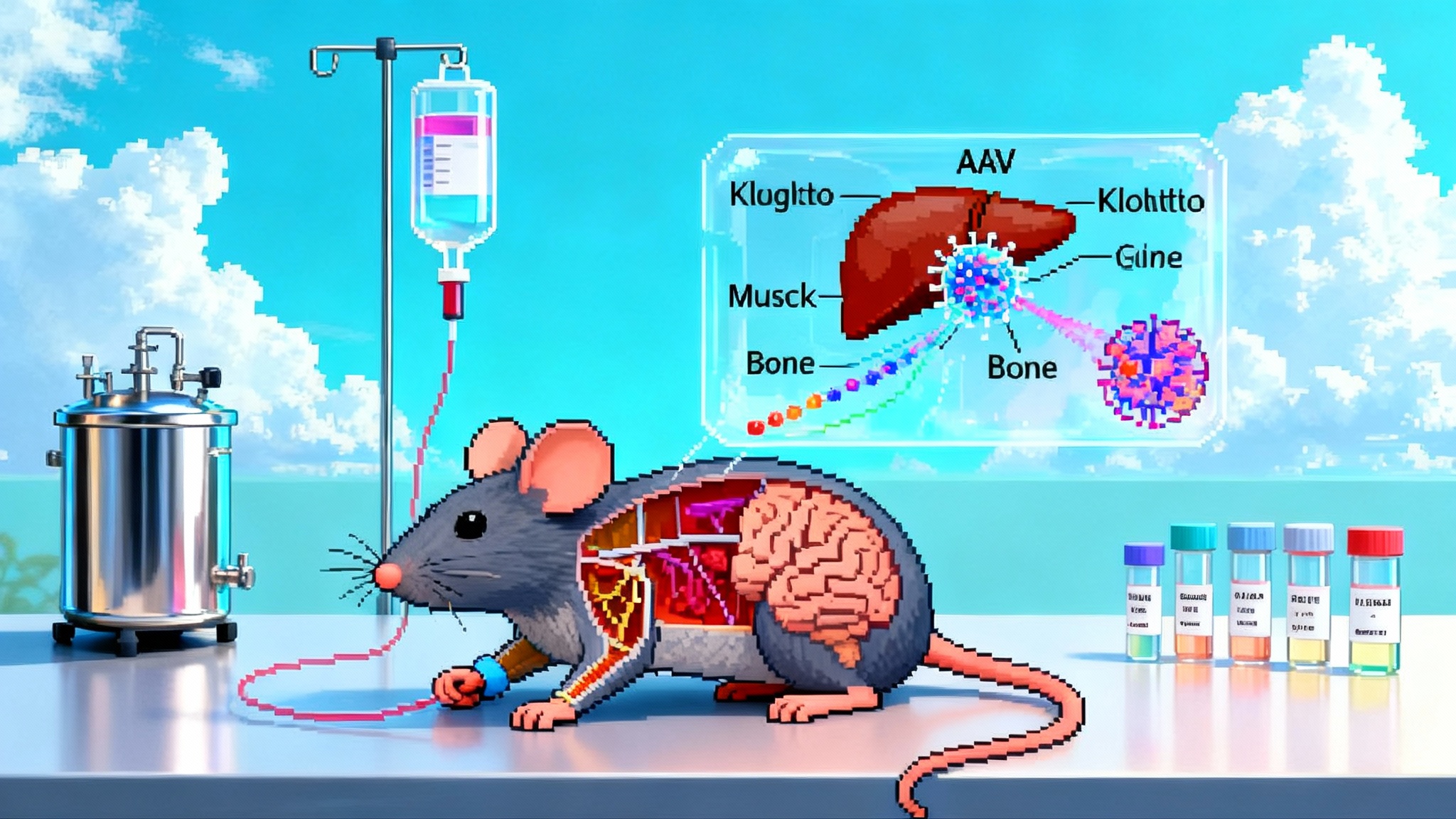
What the NIH study actually tested
- Designs: Cross-sectional snapshots and longitudinal trajectories, with repeated measures from the same individuals over years. Longitudinal data are the tougher test for a biomarker because they track within-person change.
- Species and cohorts: Humans from established cohorts including the Baltimore Longitudinal Study of Aging, plus rhesus monkeys and mice. Consistency across species and settings helps separate aging signals from lab or cohort quirks.
- Health correlates: Links between taurine and function, including measures of motor performance and body weight. Correlations were weak, mixed, or absent depending on sex, species, and cohort.
Key takeaways:
- No consistent age decline: Taurine levels tended to increase with age in several groups, remained flat in others, and did not show a consistent age-related drop.
- High within-person variability: Natural month-to-year swings often exceeded any gradual change attributable to aging.
- Thin links to function: Associations with strength or weight varied or disappeared, arguing against taurine as a robust readout of functional aging.
The conclusion is narrow and important. It does not rule out taurine having benefits under certain conditions. It tells us that the level of taurine in circulation is a weak compass for aging.
What this means for supplement claims
- Measuring taurine in blood will not reliably tell you how fast you are aging.
- If a brand markets taurine as a testable marker of biological age, that claim is now contradicted by multi-cohort, multi-species data.
- If a brand claims that raising taurine will slow aging in humans, the evidence must come from human trials with hard endpoints or validated surrogate endpoints, not from a single blood measurement. For context on trial rigor and pitfalls, revisit our rapamycin trial takeaways.
There is a broader point. Many supplement pitches hinge on a chain of inferences: a molecule changes with age in animals, manipulating it shifts other biomarkers, therefore supplementation must slow aging in you. Every link in that chain needs to hold under human testing.
Where human taurine trials stand now
Serious groups are testing taurine in humans with modern tools. The study to watch is a randomized, placebo-controlled trial in older adults in Munich, often called TauAge. It is registered as NCT06613542 and is assessing whether six months of 4 grams per day of taurine influences biological age estimates and functional measures in adults 55 to 75. See the TauAge trial overview.
What is being measured:
- Plasma proteomic age and organ-specific proteomic age estimates.
- DNA methylation clocks.
- Inflammatory and metabolic markers, including CRP, fasting glucose, insulin, lipids, and insulin resistance indices.
- Physical function, such as grip strength, leg strength, and submaximal cycling performance.
- Energy expenditure, heart rate variability, cognitive questionnaires, and quality of life.
Why this matters: if taurine changes validated aging clocks and improves function in a well-controlled trial, that is a stronger signal than cross-sectional correlations. If it does not, taurine shifts from longevity hope to niche physiology story.
What results would actually change practice
To move clinicians, payers, and regulators, taurine would need to clear all three hurdles:
- Safety at plausible doses in the target population
- No excess adverse events over six to twelve months in older adults. Particular attention to blood pressure, arrhythmias, fluid balance, and interactions with common drugs.
- Consistent, prespecified improvements in function
- Meaningful gains in objective performance: faster gait speed, stronger grip and leg power, better chair-stand or stair-climb times, greater distance on a six-minute walk. Effects should be clinically noticeable, not just statistically significant.
- Better patient-reported outcomes: fatigue, daily activity scores, and quality of life.
- Linkage between biomarker shifts and endpoints
- If proteomic or methylation clocks change, show that these shifts correlate with and help explain improvements in function in the same individuals.
- Replicate in a second trial with a different team and cohort.
Nice to have but powerful: durability beyond the dosing period, dose-response data, and subgroup analyses that hold up after correction for multiple comparisons. Cost effectiveness matters too, measured against staples like exercise programs and nutrition counseling.
A simple framework to vet longevity biomarkers before they drive behavior
Use the CLUES checklist. It is a short filter you can apply to any new aging biomarker claim.
- Clinical relevance: Is the biomarker linked to outcomes that matter, like disability, hospitalization, or mortality, in prospective human studies? Not just associated with other lab values.
- Longitudinal behavior: Within the same people, does the marker change in a stable, directionally consistent way with aging, and does it show reasonable signal to noise over months and years?
- Unconfounded signal: Does the marker retain meaning after adjusting for sex, body size, diet, medications, and physical activity, and after accounting for measurement timing, fasting, and circadian effects?
- Experimental responsiveness: When you move the biomarker with an intervention, do clinical endpoints move with it, and are the changes reproducible in independent cohorts?
- Standardization: Are the preanalytic steps and lab methods harmonized so that a number from Lab A compares to Lab B, and can patients get the same result when retested?
If a new biomarker fails two or more items, it is not ready to steer your health decisions or your portfolio.
How to read aging studies without getting burned
- Separate discovery from validation: Exploratory, multi-omic screens are hypothesis generators. Validation needs prespecified outcomes, power calculations, and independent replication.
- Check the study design: Longitudinal cohort data usually trump cross-sectional snapshots for aging trajectories. Randomized controlled trials trump both when asking what to do.
- Mind the unit of analysis: Are results reported per individual over time, or as group averages across ages? The former tells you about trajectories you can act on.
- Look for preregistration and protocols: Trials should be registered, outcomes prespecified, and analysis plans made public. Deviations require clear justification.
- Do not overread surrogate wins: A change in a methylation clock or a proteomic signature is encouraging only if it maps to better function or lower clinical risk.
- Watch multiplicity: If dozens of endpoints are tested, adjust for multiple comparisons. A handful of p values under 0.05 in a sea of tests is expected by chance.
- Demand effect sizes and uncertainty: How big is the change, and what are the confidence intervals? Small, noisy effects rarely scale to meaningful benefit.
- Consider alternatives: Exercise, sleep, diet quality, and strength training have consistent effects on functional aging. Any new pill must beat or complement that playbook.
The bottom line on taurine right now
The NIH paper is a narrow and necessary correction. Taurine’s circulating level is not a dependable gauge of aging across humans, monkeys, and mice. That finding trims one branch of the taurine narrative without chopping down the tree. The supplementation question moves to human trials with functional outcomes.
For consumers, it means two practical things. First, do not order a taurine blood test expecting a read on your biological age. Second, if you use taurine, do it with modest expectations and a plan to track how you feel and perform, not just what your lab apps say.
For investors and operators, the lesson is discipline. Build products and theses on biomarkers that pass the CLUES filter and on trials that deliver endpoint wins. Marketing that outruns the data does not last.
As results from TauAge and other studies arrive, the field will get sharper. If taurine can move validated clocks and, more importantly, help people walk faster, climb stairs with less effort, and live independently longer, that will be obvious in well-run trials. If it cannot, the story will shift to where taurine does make a difference. Aging science is full of surprising turns. The right move is to let data, not headlines, set the pace.