Mitochondria’s Breakthrough Year: Rare Cures to Longevity
Summer 2025 delivered three milestones for mitochondrial medicine: births after mitochondrial donation in the UK, an FDA-cleared Phase II cell therapy for Pearson syndrome, and precise base edits in animals and patient cells. Here is what is real, what is risky, and how this momentum could shape healthspan.
The summer mitochondria went mainstream
If you wanted a single season when mitochondrial medicine stopped living only in specialist clinics and began to shape the broader conversation about healthy longevity, this summer was it. In July, the United Kingdom’s regulator said eight babies had been born after mitochondrial donation, a landmark for families at high risk of severe inherited disease. The authority’s statement was careful and measured, but the signal was unmistakable: the approach works in real clinics for real people. See the regulator’s confirmation that HFEA confirms eight births after donation.
Weeks earlier, the U.S. Food and Drug Administration cleared a Phase II study of a mitochondrial augmentation cell therapy for Pearson syndrome, a brutal pediatric condition driven by large deletions in mitochondrial DNA. The company, Minovia Therapeutics, enriches a child’s own stem cells with healthy donor mitochondria and returns them to the body, aiming to restore energy generation from the inside out. The firm announced the clearance in April and later reported additional designations, marking a step up in regulatory engagement for mitochondrial therapies. See the company’s release that the FDA clears Phase II Pearson trial.
Add to that fresh animal and patient cell results in mitochondrial DNA base editing. In January 2025, a Science Translational Medicine paper showed that targeted edits could correct a pathogenic mutation in a mouse model while also exposing dose dependent off target issues at high vector loads. In June, researchers used mitochondrial base editors to both build disease models in human organoids and repair a pathogenic mitochondrial DNA variant in patient derived cells, while exploring messenger RNA and lipid nanoparticle delivery. These are not clinic ready, but they are no longer hypothetical.
The combined effect is an inflection point. Mitochondria are moving from rare disease fixes toward a platform that can be tuned to prevent disease, stabilize decline, or even extend healthspan across tissues that fail with age.
Why these three milestones matter
Think of a city that keeps losing power in certain neighborhoods. One crew replaces the faulty transformer before new houses are connected to the grid. Another team outfits the city’s maintenance fleet with portable batteries to keep essential services running during outages. A third group rewires tight spots that have always been substandard. That is roughly what mitochondrial medicine is doing.
- Mitochondrial donation replaces a mother’s faulty mitochondria before a child is conceived, much like swapping a transformer so new homes never see brownouts. It prevents transmission of serious mitochondrial DNA defects.
- Mitochondrial augmentation therapy adds healthy mitochondria to a patient’s own stem cells, similar to giving maintenance crews extra batteries so they can ride through blackouts. It aims to stabilize function in a failing system.
- Base editing in mitochondrial DNA repairs single letter mutations at their source. That is the targeted rewiring project, and it is the newest tool, now moving from proof of concept to early translational planning.
Each milestone addresses a different time point in the life course. Together they suggest mitochondria can be managed proactively, not only in rare pediatric disorders but also in the chronic decline that defines aging tissues.
What is real today vs what is hype
Here is the ground truth as of September 2025.
What is real now
- Eight births after mitochondrial donation have been reported in the United Kingdom under the Human Fertilisation and Embryology Authority’s licensing system. The families were at very high risk of passing on severe mitochondrial disease. Clinical follow up is ongoing and necessary, but early development is normal. Australia legalized mitochondrial donation in 2022 and is setting up programs, but has not reported births as of this writing. The United States does not permit clinical use due to a congressional rider that blocks the Food and Drug Administration from even reviewing applications that involve heritable modification of embryos.
- The Food and Drug Administration cleared a Phase II trial of a mitochondrial augmentation therapy for Pearson syndrome. The trial uses objective growth measures and functional scales in children. This is not a speculative wellness play. It is a classic rare disease development path with defined endpoints.
- Mitochondrial DNA base editing has corrected disease relevant mutations in mice and in patient derived human cells. The mouse study delivered an edit to restore transfer RNA structure and metabolic readouts in heart and skeletal muscle. It also revealed severe mitochondrial off target edits at the highest vector doses, a bright red safety flag to guide dosing and delivery choices. In human cells, researchers demonstrated both the introduction and the repair of mitochondrial DNA changes across organoids and fibroblasts, with early evidence that messenger RNA and lipid nanoparticle formats may improve efficiency and cell viability.
Claims to treat with caution
- Generalized anti aging claims on the back of mitochondrial buzz. Supplements that adjust nicotinamide adenine dinucleotide or target mitophagy can improve some biomarkers in select populations, but effects are small to moderate and vary with dose, baseline status, and adherence. Exercise remains the strongest way to raise mitochondrial density and function in muscle. Any product that advertises mitochondrial rejuvenation without a clear target, mechanism, and clinically meaningful endpoint should face a strict burden of proof.
- One shot cures across patients, tissues, and mutations. Heteroplasmy, which is the mix of healthy and mutated mitochondria within cells, differs across tissues and over time. A therapy that moves the needle in bone marrow may not do the same in brain or muscle without tailored delivery.
- A clean safety slate for base editing. Nuclear off target edits have been seen with some editor designs, and mitochondrial off target edits have now been documented in vivo at high dose. Delivery vectors can stress the immune system and organs. Safety will be earned one indication and one vector at a time.
The safety flags a smart reader should watch
- Off target editing in mitochondria and nuclei. Mitochondrial base editors avoid guide RNA import problems by using programmable DNA binding proteins, but early versions caused off target changes in nuclear DNA. Newer designs reduce that risk but do not remove it. The recent mouse study adds a parallel risk inside mitochondria themselves at high dose. Regulators and sponsors will need sensitive assays to map edits across the entire mitochondrial and nuclear genomes, not just at target sites.
- Mitochondrial DNA carryover in donation. In pronuclear transfer, a trace amount of maternal mitochondria can be carried into the embryo. Early UK reports show low levels that should not cause disease, but the levels vary. Protocol refinements and long term follow up are essential to ensure those low levels do not expand in certain tissues.
- Immune reactions to donor mitochondria. Mitochondrial augmentation introduces mitochondria from a donor source into autologous stem cells. While mitochondrial proteins are highly conserved, mismatches exist. Monitoring for immune activation, allo responses, and durability of engraftment is essential.
- Vector dose and organ load. High doses of adeno associated viruses can cause liver stress and immune complications. Lipid nanoparticles have a different profile but still concentrate in certain organs. Dose finding and organ specific safety monitoring will be central to editing programs.
The US-UK regulatory split and why it matters
The United Kingdom created a specific licensing path for mitochondrial donation in 2015. The Human Fertilisation and Embryology Authority reviews each case, limits eligibility to the highest risk families, and tracks outcomes. Australia passed its own law in 2022 and is rolling out a two stage framework, with pilot programs under strict oversight.
In the United States, a rider in the annual appropriations bill for the Food and Drug Administration states that the agency cannot use its funds to review applications for clinical trials where a human embryo would be created or modified to include a heritable genetic modification. That blocks mitochondrial donation even if a child would otherwise face a near certainty of devastating disease. The rider has been renewed each year since 2016. The result is a clear split. UK regulators can approve and monitor carefully circumscribed use. U.S. regulators cannot even consider an application. Companies and clinicians will continue to do reproductive risk reduction in the UK and Australia while advancing nonheritable mitochondrial therapies, such as cell therapies and somatic gene editing, in the United States.
From rare disease to healthspan: a near term roadmap
The practical question is how to translate this momentum into broader benefits without losing scientific rigor. Here is a focused 24 month plan with milestones.
1) Build a common scorecard for evidence strength
- Use a three tier framework: Tier 1 clinical outcomes with randomized controlled or high quality single arm data; Tier 2 validated functional surrogates; Tier 3 mechanistic biomarkers.
- Examples by tier
- Tier 1: six minute walk distance in primary mitochondrial myopathy, growth z score and International Pediatric Mitochondrial Disease Scale in Pearson syndrome, patient reported functional scales with minimal clinically important differences defined.
- Tier 2: hand grip strength, chair rise time, gait speed, and composite physical function in sarcopenia; neurofilament light and standardized motor scales in neurodegeneration cohorts with mitochondrial signatures.
- Tier 3: mitochondrial DNA heteroplasmy and copy number, citrate synthase activity, oxygen consumption rate, growth differentiation factor 15, and imaging of mitochondrial membrane potential where feasible.
For biomarker standards, see how FDA’s LDT reversal on biomarkers is resetting validation expectations.
Actions this year: convene regulators, methodologists, and sponsors to pre agree on which biomarkers can support accelerated decisions in pediatric and adult mitochondrial indications. Publish the scorecard openly so future healthspan trials can align design and endpoints from the start.
2) Advance cell and gene programs through staged risk
- Cell therapy in hematopoietic compartments is most tractable now. Run the Phase II Pearson study with transparent interim safety reviews and consider a follow on in Kearns Sayre syndrome if early signals hold. In parallel, start natural history cohorts for adult mitochondrial cytopathies that could benefit from hematopoietic support.
- Somatic base editing should stay in animal models and ex vivo patient cell systems while delivery and off target risks are reduced. Focus on high value targets with clear genotype phenotype links and tissues accessible to safe delivery, for example liver or muscle. Do not leap to brain delivery until organ specific safety margins are strong.
Adaptive, add drop designs like those used as cross-organ PER data pivot to trials can speed early signals while protecting participants.
Milestones by quarter
- Q4 2025: publish shared analytic pipelines for off target detection across mitochondrial and nuclear genomes and run multi lab ring trials on reference samples.
- Q1 2026: complete dose ranging in at least two large animal models for an editor plus delivery system, with predefined stopping rules based on off target thresholds and organ toxicity.
- Q2 2026: open a first in disease ex vivo protocol that edits patient hematopoietic stem cells for a mitochondrial DNA deletion syndrome, with reinfusion only after exhaustive off target mapping and fitness assays.
3) Translate to neurodegeneration, sarcopenia, and metabolic aging with precision subgroups
Neurodegeneration
- Who: patients with Parkinson’s disease or amyotrophic lateral sclerosis who show mitochondrial dysfunction signatures, such as reduced complex I activity, elevated growth differentiation factor 15, and specific imaging or cerebrospinal fluid markers.
- What: combine a bioenergetics modulator with rigorous lifestyle and rehabilitation programs. Consider small molecule programs that restore mitochondrial transcription or polymerase function now in human testing, and prioritize subtypes with mitochondrial DNA maintenance defects or mitophagy impairment.
- How to measure: motor and cognitive scales plus quantitative gait, wearable based activity, and mitochondrial biomarkers. Power studies for disease modification signals over symptom control.
Sarcopenia
- Who: older adults with documented low muscle mass and strength, and laboratory evidence of impaired mitochondrial function in muscle biopsy or blood derived markers.
- What: evaluate mitochondrial targeted peptides or mitophagy activators alongside high quality resistance training. Use adaptive trial designs that drop ineffective combinations early.
- How to measure: gait speed, chair stand time, grip strength, muscle cross sectional area on imaging, and patient relevant function like stair climbing. Insist on durability at six and twelve months.
Metabolic aging
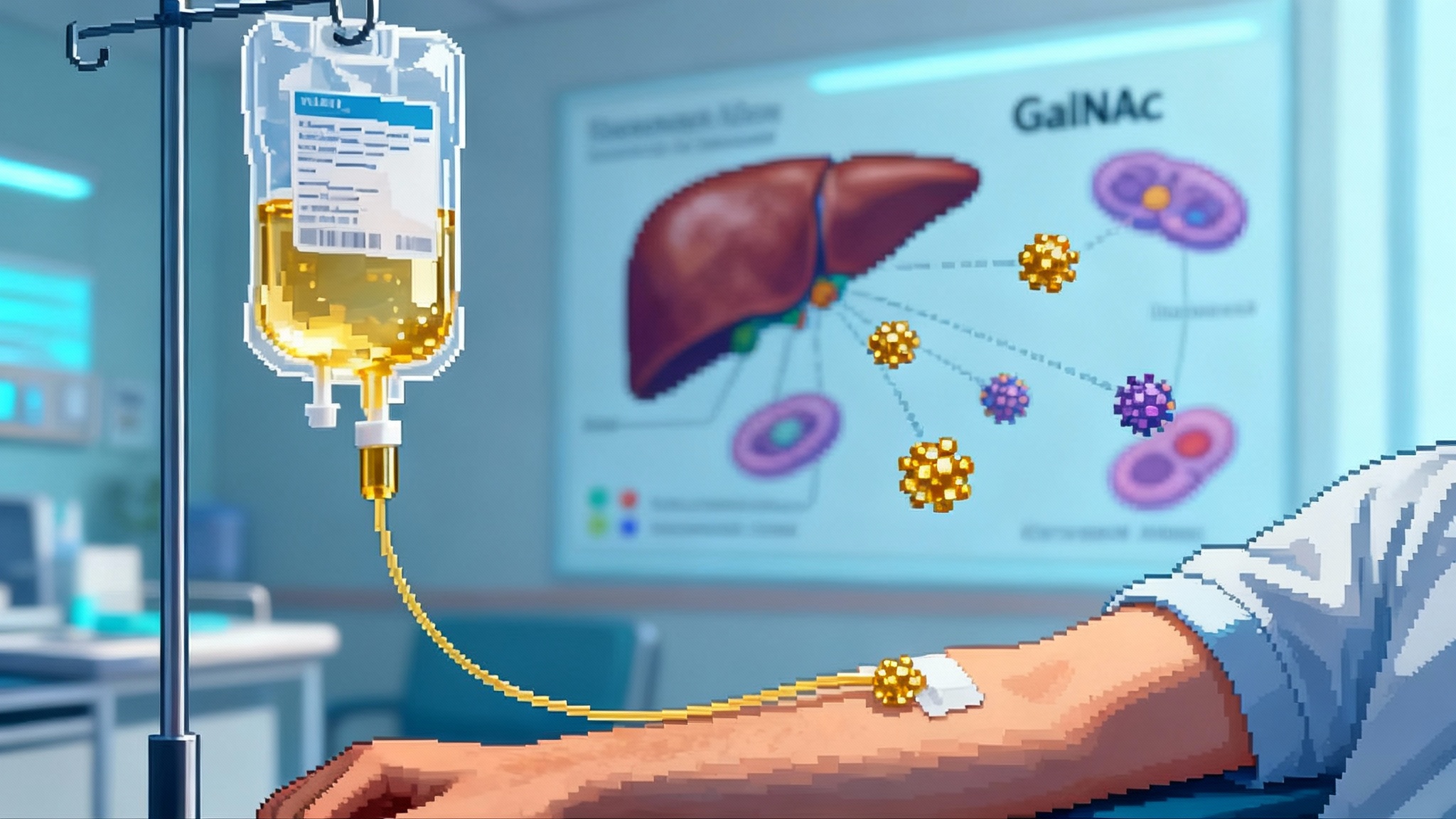
- Who: adults with fatty liver disease or insulin resistance where hepatic mitochondrial dysfunction is documented.
- What: test small molecules that improve mitochondrial transcription, replication, or substrate switching in the liver. Several programs have preclinical and early human data suggesting improved lipid handling with targeted modulation of mitochondrial gene expression or polymerase activity.
- How to measure: liver fat by magnetic resonance, insulin sensitivity, lipid flux, and safety labs. Use mechanistic endpoints such as mitochondrial DNA copy number in circulating cell free DNA as exploratory signals.
Milestones by quarter
- Q4 2025: launch two multicenter prospective registries that harmonize mitochondrial biomarkers across neurodegeneration and sarcopenia cohorts.
- Q1 2026: complete a platform trial design that allows mitochondrial agents to be added or removed based on interim functional and biomarker readouts.
- Q3 2026: read out the first adaptive stage and either expand promising arms or shut down those that fail predefined thresholds.
4) Industrialize the basics: manufacturing, analytics, and follow up
- Mitochondria as a product: standardize isolation, quality control, and release criteria for donor mitochondria used to augment autologous cells. Include assays for respiratory chain capacity, proteome integrity, and sterility that map to clinical potency.
- Analytics: publish validated pipelines for whole mitochondrial genome sequencing with heteroplasmy quantification down to 1 percent, and integrate with single cell readouts so tissue specific drift can be tracked.
- Long term follow up: commit to decade scale registries for people who receive mitochondrial donation, cell therapies, or in the future base edited interventions. Make consent forms broad enough to allow re contact when new safety assays emerge.
What the US-UK split means for builders and families
- Families in the UK with severe maternal mitochondrial DNA disease risk have a clinical path to avoid transmission. Those in the United States do not, unless they travel and coordinate care across borders. That increases inequity and complicates follow up.
- Companies should plan dual track regulatory strategies. Conduct reproductive risk reduction in jurisdictions with explicit frameworks. Pursue somatic therapies that do not touch the embryo in the United States, where the Food and Drug Administration can fully engage. Expect the rider to persist until Congress debates it directly.
How to separate durable progress from noise
A simple checklist helps:
- Target specificity: is the therapy aimed at a defined mitochondrial lesion or pathway with a plausible tissue match
- Delivery realism: can the agent reach the right cells at the right dose without unacceptable organ stress
- Measurable function: is there a predefined threshold for change on a scale that matters to patients
- Safety transparency: are off target and immune risks measured comprehensively and reported without euphemisms
- Durability: are follow ups long enough to capture heteroplasmy drift, tissue turnover, and vector persistence
Regulators increasingly want functional benefit; the dogs-first longevity FDA test shows how clearly defined endpoints can win.
The bottom line
In the span of a few months, mitochondrial medicine crossed three thresholds. Families at extreme risk have babies free of catastrophic mitochondrial disease. A cell therapy built on the logic of adding healthy power plants to a failing grid is entering a mid stage trial with clinically meaningful endpoints. Base editing is fixing mitochondrial DNA in animals and patient cells, while also surfacing the exact safety problems that must be solved.
This is how a real platform is born. Not through a single moonshot, but through a series of specific wins that line up across prevention, stabilization, and repair. The next two years will be about disciplined translation. If researchers keep dosing honest, if regulators keep follow up long, and if companies publish what does not work as clearly as what does, mitochondria will move from a rare disease backwater to a central tool for extending the years we can live with strength, clarity, and independence.