CMV’s 2025 readout could launch longevity vaccines
Moderna’s cytomegalovirus vaccine is nearing a pivotal 2025 efficacy readout that could recast prevention as a lever on immune aging. Here is what matters for regulators, payers, and anyone tracking the first real test of longevity vaccines.
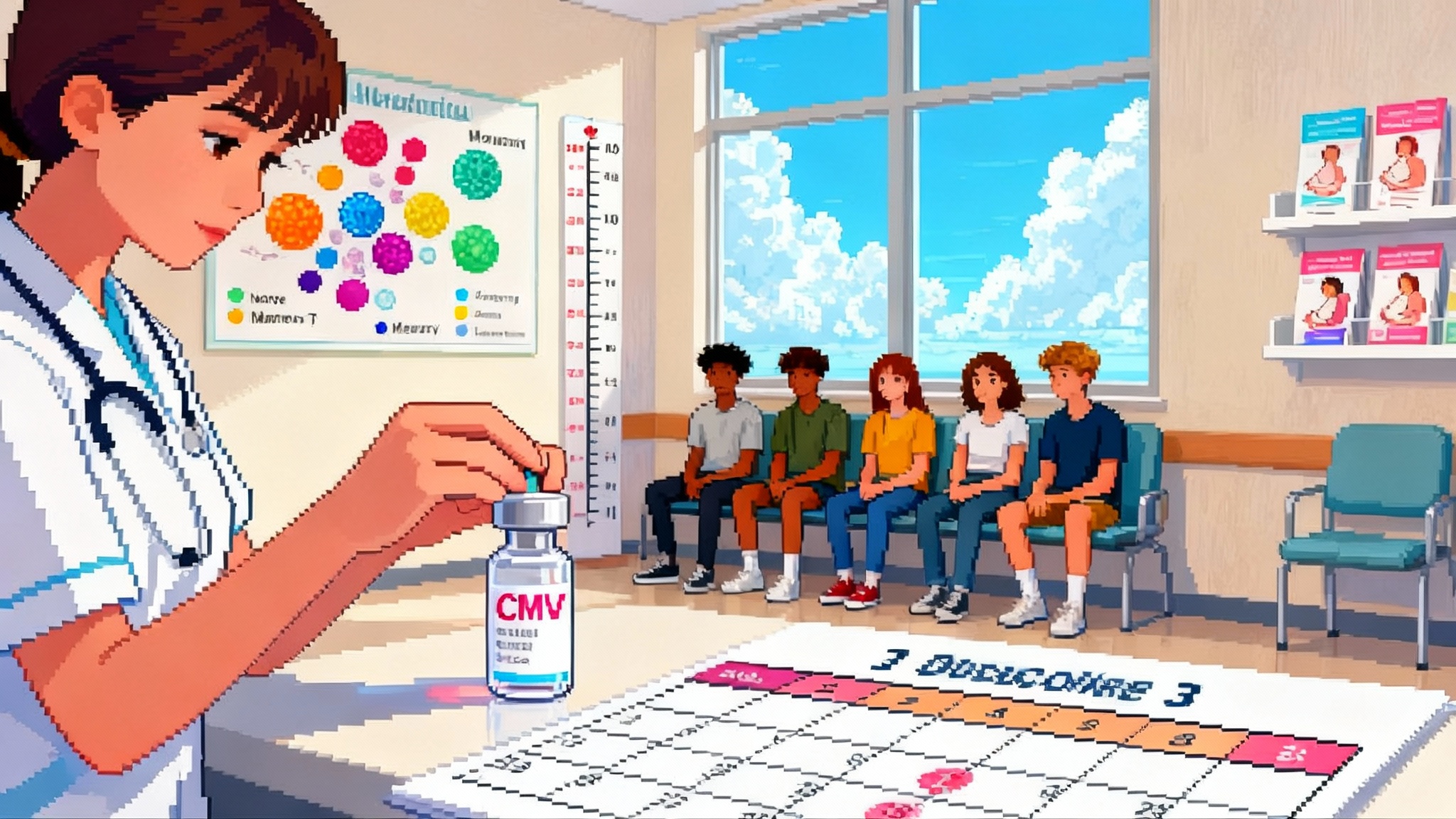
Breaking: the year longevity vaccines step into the mainstream
Moderna entered 2025 with its cytomegalovirus vaccine at a decisive moment. The company says its pivotal Phase 3 trial is fully enrolled, durability data from earlier studies were presented this spring, and the efficacy readout is expected this year. That timing makes cytomegalovirus the most advanced longevity vaccine in a space that aims to blunt the biology of aging by stopping the latent viruses that quietly wear down our immune systems. See Moderna’s January 2025 update.
This is not a niche scientific curiosity. If the study shows protection against primary infection in the target population, regulators, payers, and public health agencies will have a clear basis to act. It would be the first time a vaccine program is framed not only as preventing a specific disease, but as a lever on immune aging itself.
Why CMV sits at the center of immune aging
Cytomegalovirus is a herpesvirus that most people catch at some point in life and then carry forever. It usually causes no symptoms in healthy adults. The catch is what comes next. CMV keeps the immune system on a low simmer for decades. Over time, it coaxes armies of highly specialized T cells to park themselves on the same viral target again and again. Those veteran cells crowd the immune roster, leaving fewer naive recruits ready to respond to new threats. Researchers call the result immunosenescence and, when chronic inflammation is part of the picture, inflammaging. For a primer on restoring youthful immune capacity, see how naive T cells as longevity's edge fits into the broader strategy.
A simple metaphor helps. Imagine your phone storage filled with thousands of high resolution photos of a single event. The phone still works, but it is slower, you cannot take new photos when you need to, and background processes get glitchy. CMV is the photo hoarder. It fills memory with one theme and starves the system of flexible capacity.
What does that mean in real life? Across long follow ups, CMV seropositivity has been linked to changes in T cell balance and, in some cohorts, to higher mortality and cardiovascular risk later in life. The association size varies by study and population. A recent long run United States cohort analysis found a modest but statistically significant elevation in all cause mortality risk among CMV seropositive adults after adjustment for socioeconomics and health factors. See this long run U.S. cohort analysis.
Two things are simultaneously true. One, correlation is not causation. Two, CMV’s biology gives a very plausible mechanism by which lifelong carriage can reshape immune architecture. Preventing primary infection early in life is the cleanest test of the causal story.
The news hook: how Moderna’s trial is built to answer the question
The pivotal study is straightforward in concept. It enrolls women of childbearing age who are seronegative for CMV. Participants receive three doses at zero, two, and six months. The primary efficacy endpoint measures whether participants become infected during follow up, typically using seroconversion to CMV antigens not encoded by the vaccine and confirmed by virologic assays. Safety, reactogenicity, and immunogenicity round out the core dataset. The company disclosed that a 2024 interim analysis did not meet the threshold for early stopping, and that the independent monitoring board recommended continuation to the final readout in 2025.
Three design features matter for longevity:
- Primary prevention strategy. By vaccinating people before first exposure, the trial reads on the most consequential fork in the road. The immune system either never enters the CMV feedback loop or it does.
- Clean endpoint. Seroconversion gives a clear yes or no answer about infection, avoiding confounding from social or clinical factors.
- Durability follow up. Extended observation helps quantify how long protection and immune markers persist, which is central to any claim about effects on immune aging.
How much healthspan could this buy?
It is tempting to translate immunology into a neat number of years gained, but any honest estimate must be explicit about assumptions. Here is a simple two scenario frame to guide expectations, using public epidemiology and plausible adoption patterns.
- Scenario A: conservative. Assume a vaccine with moderate efficacy that delays or prevents CMV infection in half of vaccinated adolescents and young adults over a decade of exposure. Using cohort estimates that put the adjusted all cause mortality hazard difference near 10 percent for CMV seropositivity in mid to late life, and assuming only half that association is causal, the population level effect for those vaccinated might be a 2 to 3 percent reduction in later life mortality risk. That maps to a modest average gain in healthy years, on the order of months, with larger benefits concentrated in groups with high exposure risk.
- Scenario B: optimistic. Assume higher efficacy and earlier vaccination before the most intense exposure years. Combine that with a stronger causal component for cardiovascular outcomes in specific subgroups. In that case, the average gain could approach one year of healthy life for vaccinated individuals who would otherwise have acquired CMV in adolescence or early adulthood. Benefits would be amplified if durable protection reduces downstream risks like poor vaccine responses in old age.
These are scenarios, not promises. The final readout, followed by real world data, will tell us where the truth sits. The key takeaway is that even small percentage shifts, delivered at population scale and early in life, generate large cumulative gains in healthy person years.
From congenital disease to longevity: a regulatory path that can scale
Regulators will judge CMV on a classical vaccine endpoint: prevention of primary infection in seronegative women of childbearing age. That target alone has major public health value because primary infection during pregnancy can lead to congenital CMV, a leading infectious cause of birth defects and lifelong disability. Approval on this endpoint would justify near term adoption, independent of any later benefits on immune aging.
How does that translate into longevity? Two steps:
-
Evidence bridge. Post approval, sponsors and public health agencies can link initial infection prevention to long term immune markers. Examples include the CD4 to CD8 ratio, the frequency of terminally differentiated T cells, and vaccine responsiveness in older ages. If these markers remain more youthful in vaccinated cohorts, the causal case strengthens. For context on measurement frameworks and policy guardrails, see the ongoing aging biomarker race.
-
Outcomes registries. Longitudinal registries can track major outcomes in vaccinated versus unvaccinated individuals, such as cardiovascular events, pneumonia hospitalizations, and all cause mortality. Because these outcomes take years to unfold, regulators are unlikely to require them for initial approval, but payers and policy bodies will ask for them to refine recommendations and budgets.
The practical point: a CMV label based on prevention of primary infection unlocks a strong health economic case right away, thanks to congenital disease prevention. The longevity upside is the dividend on top.
Who should get it, and when
Assuming a positive readout and an advisory vote in favor of broad use, the rollout should follow four tracks.
- Adolescents before peak exposure. Middle school or early high school vaccination offers the cleanest path to block primary infection before dating, college, and childcare work increase exposure risk. School based programs and pediatric clinics can deliver scale at low incremental cost.
- Women of childbearing age. This is the core of the pivotal trial, and the most direct way to prevent congenital CMV. Obstetrics and gynecology practices can offer vaccination at preconception and postpartum visits. Insurers already cover many preventive vaccines in this age range.
- Catch up for seronegative adults. For healthcare, childcare, and eldercare workers, a simple serology plus vaccination pathway could reduce both personal risk and onward transmission in high contact settings. Employers may be willing to sponsor testing and vaccination as part of workforce health programs.
- High risk medical populations. Although outside the initial label, transplant programs and oncology centers already manage CMV aggressively. If data from indication expansion studies are positive, vaccinating seronegative candidates in these settings could reduce reactivation and severe disease.
Each track has a distinct value proposition. Adolescents maximize prevention and long horizon dividends. Women of childbearing age anchor congenital benefits. Occupational catch up protects services that society depends on. Medical high risk groups reduce extreme cases and costs.
EBV is close behind, with a different endpoint and narrative
A second latent herpesvirus, Epstein Barr virus, is advancing toward pivotal studies. Moderna’s prophylactic EBV vaccine candidate focuses first on preventing infectious mononucleosis in adolescents and young adults. That endpoint is visible within one to two seasons and can support a classic label. The longer arc is more ambitious. EBV infection is linked to multiple sclerosis and several cancers. If a preventive vaccine is safe, effective, and widely adopted, future registries could test whether early vaccination reduces those risks.
There are important differences between the CMV and EBV paths:
- Endpoint and timing. CMV aims to prevent primary infection to protect pregnancies now and immune architecture later. EBV aims to prevent mononucleosis first to build a label and adoption, while the field studies harder long term endpoints.
- Target populations. CMV starts with women of childbearing age, then pushes younger. EBV starts with adolescents and young adults of all genders and may eventually move younger.
- Regulatory milestones. CMV’s 2025 efficacy readout could support a near term filing if the effect is robust and safety is clean. EBV programs are likely to pursue pivotal trials with infectious mononucleosis reduction as the primary endpoint, with primary completion targeted later in the decade.
Taken together, CMV and EBV are the opening moves in a larger shift. They use familiar vaccine development rules to pursue unfamiliar, lifespan scale payoffs. For a contrast with drug centric approaches, see rapamycin's first human longevity trial.
What will regulators and payers look for next
As the CMV dataset matures, expect scrutiny in five areas:
-
Point estimate and confidence intervals. A clear reduction in primary infection with tight bounds is essential. Decision makers will want to see subgroup analyses by age, baseline exposure risk, and geography.
-
Safety and reactogenicity. The messenger ribonucleic acid platform has accumulated large safety datasets in respiratory vaccines, but latent virus vaccines involve multi dose schedules in younger people. Transparent reporting of adverse events, pregnancy outcomes, and any autoimmune signals will be critical.
-
Durability. If neutralizing antibodies and functional T cell responses remain elevated for several years, dosing schedules can stay simple. If immunity wanes quickly, modeling will need to show whether boosters are worth it.
-
Real world effectiveness. Case control studies in health systems and claims databases can validate trial efficacy and help tune recommendations.
-
Health economics. Even before formal longevity dividends are counted, preventing congenital CMV saves healthcare and special education costs. Models that factor in avoided disability plus possible later life benefits will drive payer enthusiasm.
Near term signals to watch in 2025
- The efficacy readout itself. Does the trial meet its primary endpoint of preventing primary infection in seronegative women of childbearing age, and what is the effect size?
- Durability data extensions. Look for follow up presentations that show antibody and T cell responses holding at 24 to 36 months in Phase 2 extension cohorts.
- Advisory committee scheduling. The timing of any regulatory meetings will signal the confidence and pace toward potential approval.
- Adolescent studies. Early immunogenicity and safety signals in adolescent cohorts will shape whether school age vaccination becomes the default path.
- EBV program waypoint. Watch for a definitive outline of pivotal design geared to infectious mononucleosis reduction, including seasonality considerations and assay plans.
What this means for longevity research and practice
Longevity science has spent two decades refining drugs that target age related damage once it has accumulated. Vaccines against latent viruses offer a different logic. They move the battle line to the start of the story and they scale. A three dose series delivered by pediatricians and obstetricians can reach most of the population at low marginal cost. The risk profile is familiar. The benefit, though, shifts from a single disease focus to systems level maintenance of immune flexibility.
If CMV prevention shows strong efficacy and clean safety this year, it will give health systems a new lever with three layers of value:
- Immediate. Fewer primary infections in women of childbearing age and fewer congenital CMV cases.
- Medium term. Smoother vaccine responses and fewer severe infections in adults who remain CMV seronegative longer.
- Long term. A measurable shift in immune aging markers and, if the registries bear it out, a reduction in age related morbidity and mortality.
That is what makes 2025 a hinge. CMV has a clear clinical endpoint that stands on its own and a plausible path to something bigger. EBV is a step or two behind on the timeline, but it may prove even more consequential if it bends risks for multiple sclerosis and certain cancers.
What to do now
- Public health planners. Prepare for a recommendation framework that starts with women of childbearing age and adolescents. Map serology plus vaccination workflows for high exposure occupations. Budget for registry infrastructure, since long horizon outcomes will be part of the value case.
- Clinicians. Build patient education that explains CMV’s silent load on the immune system in plain terms. Integrate vaccination into preconception care and adolescent well visits.
- Employers in healthcare and childcare. Pilot voluntary serology and vaccination programs. The cost is modest, and the upside spans reduced sick days, fewer exposures, and long term workforce health.
- Researchers. Pre register cohorts that can measure immune aging markers prospectively in vaccinated versus unvaccinated groups. Prioritize assays that are reproducible across labs so results can inform policy.
The bottom line
Vaccines have always been a longevity technology. We just did not label them that way. CMV’s 2025 readout is the first explicit test of a preventive strategy aimed at the biology of aging itself. If the data are there, the path from press release to policy looks navigable. And if we get it right, a teenager’s three clinic visits in 2026 could echo in their immune system for decades. That is how prevention becomes the new frontier of longevity.