From Eye to Brain: OSK Reprogramming Enters Trials
On September 25, 2025, FDA INTERACT feedback gave YouthBio a path to clinic for brain-targeted partial reprogramming. Life Biosciences is moving ER-100 toward first-in-human vision trials, making ophthalmology the launchpad for longevity tech.
The day aging science met the clinic
A field that once lived mostly in mouse papers has crossed into human plans. On September 25, 2025, YouthBio said the Food and Drug Administration gave positive INTERACT feedback on its brain-targeted partial cellular reprogramming candidate for Alzheimer’s disease, establishing a clear route to a first-in-human study. The company framed the meeting as a green light to proceed toward a pre-Investigational New Drug package and pilot toxicology, a key de-risking moment for a modality once considered science fiction. That news, paired with Life Biosciences’ push to bring its OSK vision therapy to patients, marks an inflection point. YouthBio’s update is public in a press release that summarizes the discussion and next steps for its program, YB002, in Alzheimer’s patients (YouthBio INTERACT announcement).
This turn to the clinic fits a broader pattern across longevity biotech, from Klotho’s first human trials to in vivo CAR-T senescence therapy.
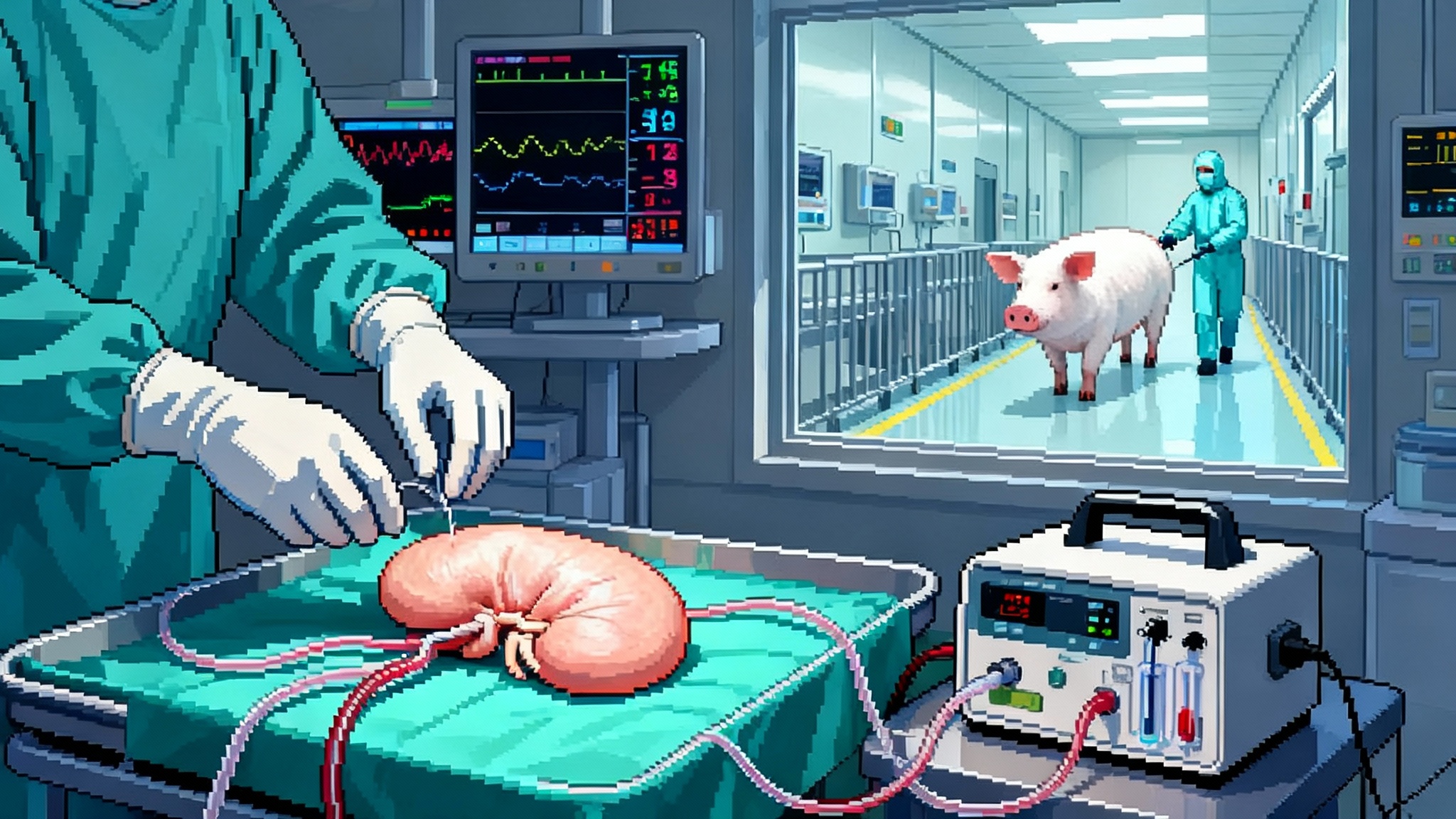
Life Biosciences has been building toward first-in-human studies of ER-100, a gene therapy that expresses three Yamanaka factors, Oct4, Sox2, and Klf4, in the eye. The company previously guided to second half of 2025 for its initial trials in two optic neuropathies, nonarteritic anterior ischemic optic neuropathy and primary open angle glaucoma. In an August 26, 2025 update from the Aging Research and Drug Discovery meeting, Life Biosciences reiterated readiness and indicated timing that narrows to early 2026. The direction of travel is the same: ophthalmology first, then the rest of the central nervous system. Those ARDD remarks and fresh preclinical data are summarized in the company’s post (Life Biosciences ARDD 2025 update).
Taken together, the signs point to a simple truth. Partial reprogramming has left the hypothesis stage. It is now marching toward the clinic, beginning where biology and regulation make the most sense: the eye.
Why ophthalmology is the beachhead for longevity tech
Drug developers start in the eye for reasons that are practical, measurable, and patient centered.
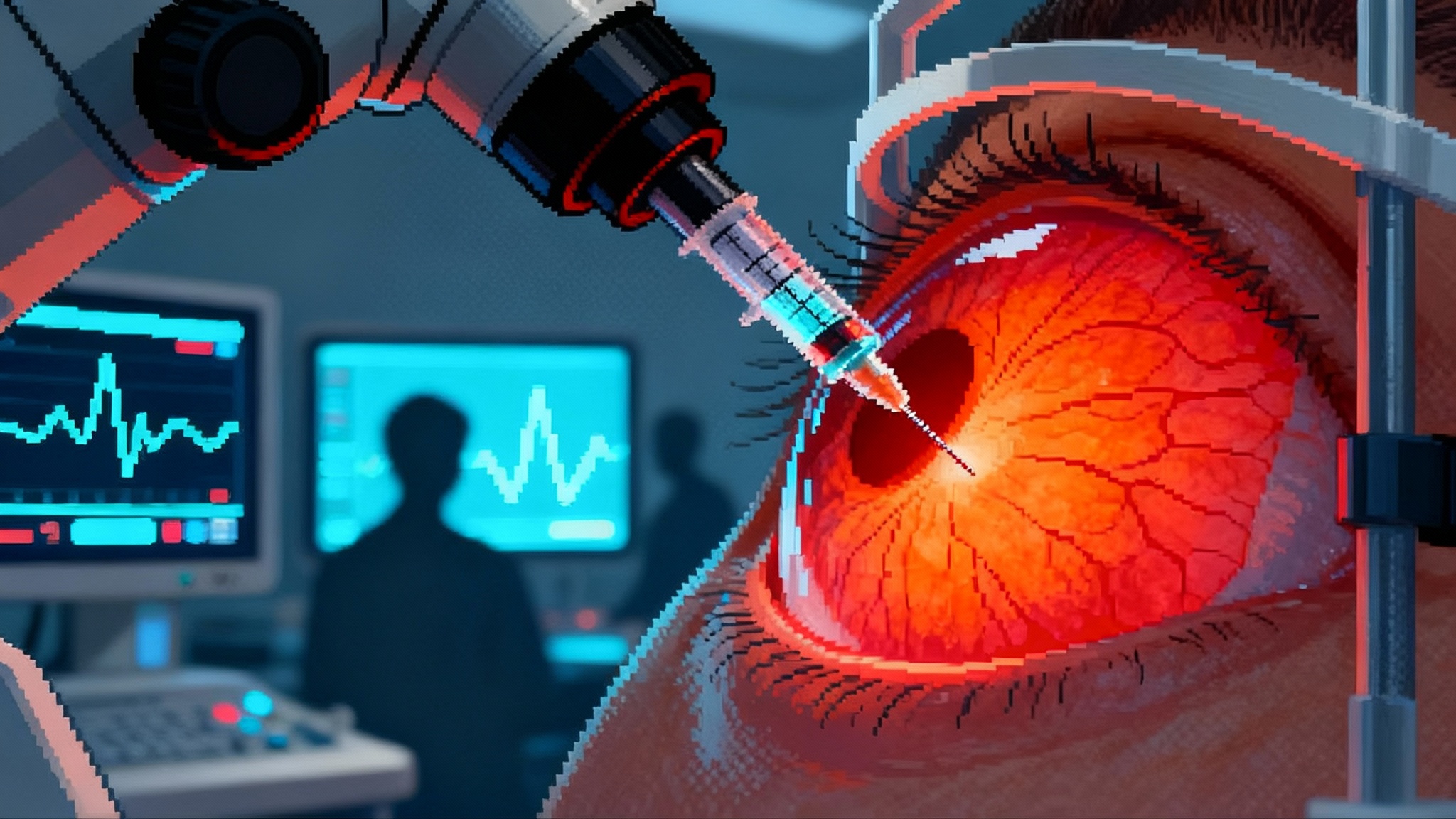
- Contained dosing. The eye is a small, closed compartment. A single intravitreal or subretinal injection can bathe the target cells in a controllable dose while keeping systemic exposure low. In a field that asks cells to temporarily express transcription factors, containment acts as a safety rail.
- Clear functional readouts. Vision gives you endpoints that matter to patients and regulators. Best corrected visual acuity reads how many letters a person can see on a chart. Pattern electroretinogram measures retinal ganglion cell function. Optical coherence tomography tracks retinal nerve fiber layer thickness, a structural correlate of axon health. Visual fields and contrast sensitivity add more layers. These are objective, repeatable, and interpretable.
- Built pathways. The eye has already hosted gene and cell therapies. Retina specialists, trial coordinators, and imaging infrastructure are in place. Surgical techniques for intravitreal, subretinal, and suprachoroidal delivery are standardized. That shrinks operational risk and timeline.
- Internal control. In many optic neuropathies, one eye can serve as a control for the other, tightening statistics without adding risk.
For longevity tools that aim to dial cell biology back toward a youthful state, the eye offers the ideal proving ground. If a therapy can protect or restore retinal ganglion cells in a disease like nonarteritic anterior ischemic optic neuropathy or slow the neurodegeneration of primary open angle glaucoma, the win will be both clinically meaningful and mechanistically clarifying.
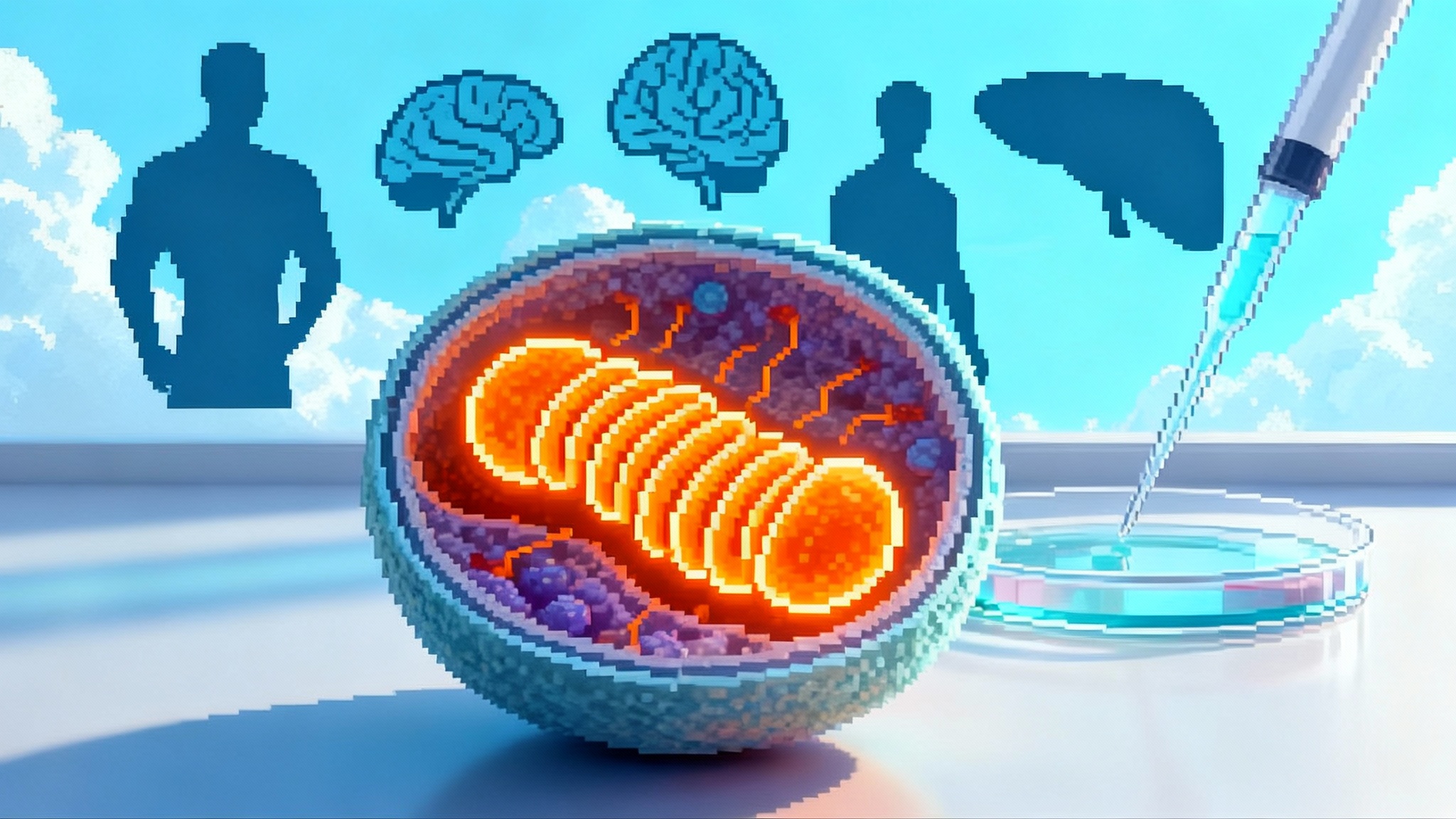
How partial reprogramming works, without magic words
Reprogramming is often described as “turning back the clock,” which is unsatisfying without detail. Think of a cell’s identity and performance as a symphony written in pencil on sheet music. Over time, the pencil marks smudge. The notes are still there, but they are harder to read and play. Epigenetic marks are the clean or smudged pencil strokes that govern which genes turn on or off. Partial reprogramming uses a measured dose of three transcription factors, Oct4, Sox2, and Klf4, to tidy the sheet without replacing the song. The goal is to restore youthful patterns of gene expression while preserving the cell’s identity as a neuron, photoreceptor, or retinal ganglion cell.
Two design choices matter. First is the vector that carries OSK into cells. Most ocular programs use adeno associated virus, often AAV2 or a close cousin, which has a track record in the retina and a cargo limit that fits OSK when paired with a compact promoter and a control switch. Second is the on-off control. Many groups use a doxycycline inducible system, sometimes called Tet-On, to make OSK expression tunable. The drug acts like a dimmer switch. Give nothing and expression is off. Give a little and expression rises to a planned level. This control is central to safety because too much or too long a dose of reprogramming factors could push cells to lose identity or divide when they should not.
In preclinical studies, periodic induction of OSK has been associated with improvements in electrophysiology and structure in models of optic nerve injury and age related decline. The premise is not to rebuild an organ from scratch. It is to give existing cells a carefully timed push to restore function.
Safety and delivery trade offs the first patients will test
The first generation of clinical trials will probe a handful of safety and delivery questions that translate directly into success or failure.
- Vector versus payload balance. AAV is familiar to retina surgeons and regulators. It can achieve long lasting expression after a single injection, which is convenient but raises questions about the duration of the off switch. If expression needs to stop completely and immediately, a regulated system plus careful promoter choice must be validated in humans. The benefit of AAV stability is fewer injections and steady distribution where you want it.
- Route of administration. Intravitreal injection is clinic friendly and targets retinal ganglion cells, the key population in glaucoma and nonarteritic anterior ischemic optic neuropathy. Subretinal injection reaches photoreceptors and retinal pigment epithelium but requires a surgical suite and is better suited to macular diseases. Suprachoroidal injections are emerging for certain targets with different distribution and immune profiles. Each route changes which cells see OSK and how much of the vector reaches them.
- Immune responses. Even in the eye, inflammation can occur. Mitigation strategies include steroid prophylaxis, vector engineering, and dose selection. Patients with preexisting antibodies to the chosen AAV capsid might be excluded or stratified. Long term, re-dosing questions loom, particularly if patients benefit and want a second course.
- Expression control. Tet-On systems introduce their own pharmacology. Doxycycline exposure has to be safe for the intended dosing windows, and the clinical team needs confidence that OSK truly turns down when doxycycline is withdrawn. That means building pharmacodynamic markers of expression into early trials, such as blood or aqueous humor sampling for vector-derived transcripts or proteins. For measuring change beyond the eye, expect greater reliance on validated biomarkers as the field matures, informed by FDA’s LDT reversal on biomarkers.
- Off target and identity risk. Excessive expression could, in principle, push mature neurons toward a less differentiated state. Developers will use neuron-specific promoters, carefully titrated induction, and limited expression windows to avoid that outcome. The eye’s compartmentalization helps, but the burden of proof is clinical.
None of these trade offs are theoretical concerns on a slide. They will be tested in the first cohorts.
The first indications and their readouts
Nonarteritic anterior ischemic optic neuropathy typically presents as sudden, painless vision loss due to impaired blood flow to the optic nerve head. Many patients experience permanent deficits in the affected eye. The clinical goal for a therapy like ER-100 is to preserve or restore retinal ganglion cell function after the ischemic insult. Trials will likely track pattern electroretinogram for function, optical coherence tomography for nerve fiber layer thickness, and visual acuity and fields for patient-centered outcomes. Because the event is acute, time to treatment and window of rescue matter.
Primary open angle glaucoma is chronic and progressive. It quietly erodes retinal ganglion cells over years even as intraocular pressure is managed. Here the bar is to slow or reverse functional decline independent of pressure control. Mean deviation on visual fields, changes in optical coherence tomography measures of ganglion cell complex thickness, and contrast sensitivity are practical. Longer studies may be needed, but early signals in electrophysiology can guide dose and schedule.
The importance of these choices is not academic. Demonstrating functional gains or strong neuroprotection in either disease will tell us whether partial epigenetic reprogramming can help neurons that are injured but not dead. That is the bridge to the brain.
What YouthBio’s and Life Biosciences’ moves reveal about timing
The calendar matters. On September 25, 2025, YouthBio disclosed that its Food and Drug Administration INTERACT meeting produced supportive feedback on preclinical bioactivity and a path to first-in-human evaluation in Alzheimer’s disease. That moves the discussion from “is this allowed” to “what exactly goes in the Investigational New Drug package.”
Life Biosciences spent 2024 and 2025 showing nonhuman primate data and refining dose and timing. The company had previously guided that first human studies would begin in the second half of 2025 for nonarteritic anterior ischemic optic neuropathy and primary open angle glaucoma. In its August 26, 2025 ARDD communication, the company indicated first quarter 2026 for both indications. Slipping from late 2025 into early 2026 is common for first-in-class gene therapies as Chemistry, Manufacturing, and Controls packages, final toxicology, and clinical site activation firm up. The strategic point stands. Ophthalmology is the proving ground, and the window for first patients is opening.
From eyes to brain to body: a realistic 2026 to 2028 roadmap
If early ophthalmology trials show safety and a clear functional signal, several doors open quickly.
- Brain targeted reprogramming. YouthBio’s program is already oriented to Alzheimer’s disease. A positive vision readout would strengthen the case that transient OSK expression can help stressed neurons recover. Brain delivery brings new questions about vector choice, route, and distribution. Intracerebroventricular or intraparenchymal delivery may be explored in small, targeted regions at first, supported by magnetic resonance imaging and cerebrospinal fluid biomarkers. The ophthalmology data will provide the first human proof that the expression control system and safety measures behave as expected.
- Peripheral organs with clear endpoints. Success in the retina will also help programs in liver, muscle, and kidney, where structural and functional measures are available and where localized delivery can be attempted. Dosing lessons from the retina will inform how to set induction cycles, break periods, and total exposure in organs that turn over more slowly than the eye.
- Systemic aging interventions. By 2027 and 2028, if both safety and efficacy are established in localized tissues, companies may propose carefully bounded systemic regimens for defined patient populations, such as early frailty with sarcopenia or metabolic dysfunction with clear tissue targets. Systemic delivery raises fresh safety considerations, including biodistribution to off-target tissues and long term immunogenicity. The retina data will not answer everything, but it will provide the first human proof of controlled, beneficial partial reprogramming.
The most valuable downstream effect may be regulatory. Once one organ system shows a clear benefit-risk profile with tight control of induction, regulators will have a template for endpoints, monitoring, and stopping rules. That speeds the path for brain and systemic studies.
What to watch between now and first readouts
- The exact trial designs. Look for dose escalation with built-in safety pauses, staggered starts, and clear pharmacodynamic plans to show that the on-off switch is working. Trials should pre-specify how doxycycline dosing will be adjusted and how expression will be monitored directly or indirectly.
- Baseline enrichment. In nonarteritic anterior ischemic optic neuropathy, enrolling patients within a defined time window after onset is crucial. In primary open angle glaucoma, enriching for patients likely to show change on electrophysiology over a six to twelve month horizon will help detect a signal.
- Imaging and function alignment. The most convincing early story will align anatomical and functional changes. A gain in pattern electroretinogram paired with stabilization or thickening of the retinal nerve fiber layer and improved contrast sensitivity is more persuasive than movement in a single endpoint.
- Manufacturing clarity. Companies should detail the capsid, promoter, and the regulatory cassette they use, and how they will ensure batch-to-batch consistency for a product that aims to express three factors in a regulated fashion. This is not just for investors. It is the bedrock of a safe first-in-human experience.
Practical takeaways for teams entering the space
- Start where endpoints are strongest. If you are not in the eye, your next best targets are organs with short feedback cycles and quantitative imaging or function, such as liver or muscle. Define a core endpoint that reads within months, not years.
- Build a pharmacology plan for your switch. Do not rely on qualitative markers alone. Specify how you will prove in humans that expression turns on and turns off. Use matched sampling of aqueous humor or cerebrospinal fluid where possible.
- Pre-negotiate immunomodulation. Align with clinical sites on steroid timing, dosing, and rescue protocols. Decide how you will handle patients with preexisting neutralizing antibodies against your capsid.
- Plan for re-dosing. Even if you hope a single series is enough, determine whether and how you would re-treat. Ophthalmology can tolerate a repeat intravitreal injection. The brain will not be as forgiving without a strong rationale.
- Pair your story with patient value. In glaucoma, connect your electrophysiology gains to fall risk, driving, or reading speed. In nonarteritic anterior ischemic optic neuropathy, quantify daily life improvements. Regulators respond to clear patient benefit.
The bigger picture
There is a reason this field is entering through the eye. It is where biology, measurement, and regulation overlap in a way that lets you test an ambitious idea safely. YouthBio’s path to the clinic in Alzheimer’s and Life Biosciences’ move to human vision trials tell a coherent story. If partial reprogramming helps neurons in the retina, the same logic can reach the hippocampus and cortex. If it works there, carefully bounded systemic applications follow.
The most important lesson is not that aging has a single switch. It is that the body retains capacity that can be coaxed back with precise, temporary instructions. The job now is to prove that those instructions can be given safely, that they move the endpoints patients care about, and that the same playbook can scale from eyes to brain to body. If the first patients see better in 2026, the next patients may think more clearly in 2027, and by 2028 we could be discussing how to rejuvenate entire organ systems with the same controlled choreography.