The Next Longevity Lever: Lp(a) Suppression Goes Mainstream
In 2025, lipoprotein(a) finally became actionable. Durable RNA silencers cut Lp(a) 80 to 95 percent and an oral blocker emerged, setting up twice-yearly injections or a daily pill as a new backbone for cardiovascular prevention.
Breaking: the year Lp(a) became actionable
If you wanted a single, real-world lever to slow cardiovascular aging, it just arrived. In 2025, multiple trials showed that silencing the liver’s production of lipoprotein(a), or Lp(a), can push this stubborn risk factor down by 80 to 95 percent and keep it down for many months after dosing. One program did it with an injection given as rarely as twice a year, and another did it with a pill. Together they point to a simple future: measure Lp(a) once in a lifetime, and if it is high, suppress it on a predictable schedule as part of routine prevention. The strongest 2025 data come from lepodisiran, where Phase 2 results presented at ACC showed deep and durable lowering with infrequent dosing, as summarized in the ACC journal scan on lepodisiran Phase 2.
First, the biology in plain English
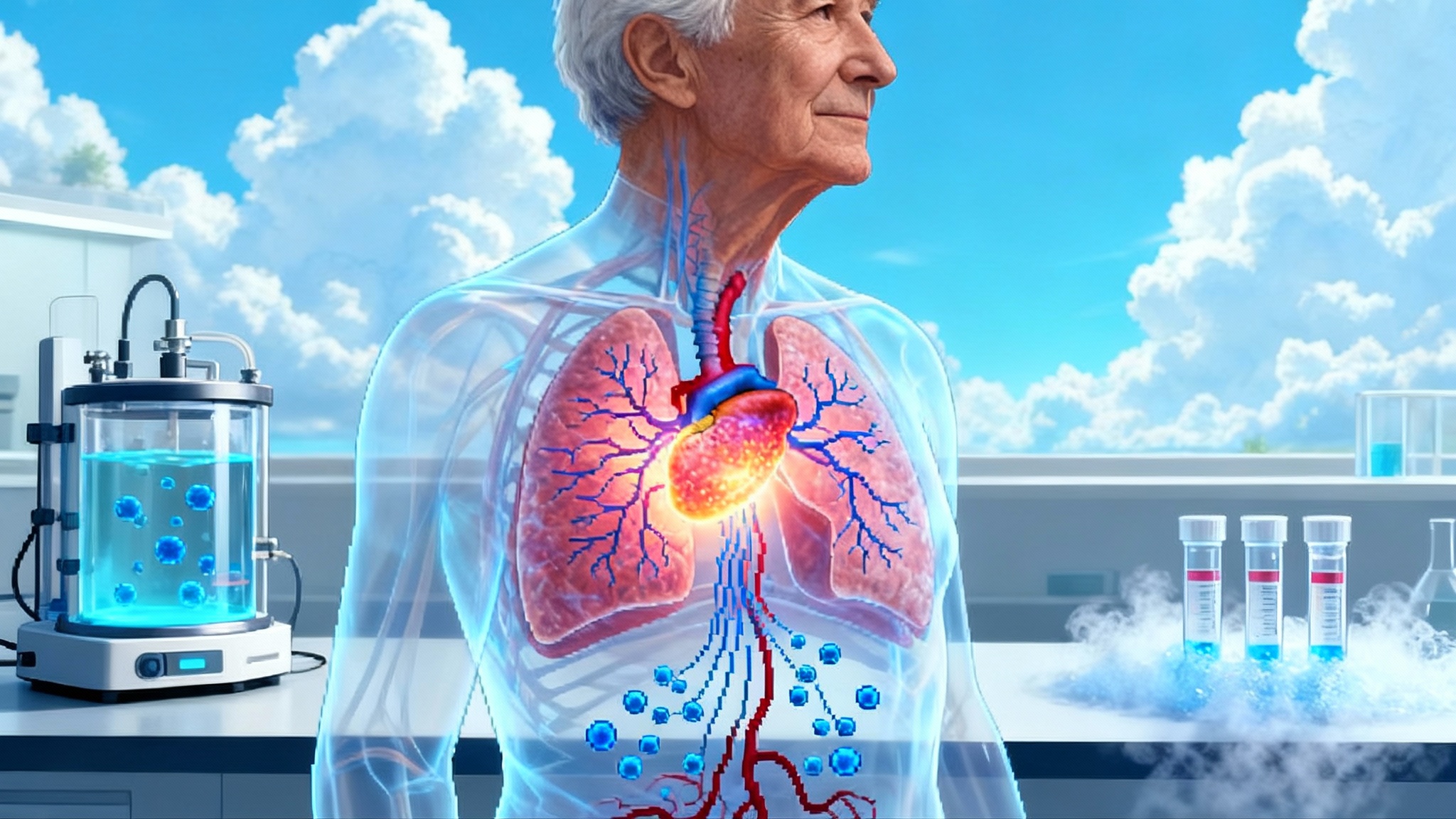
Think of Lp(a) as an LDL particle wearing a Velcro scarf. The scarf is apolipoprotein(a), a sticky protein that turns LDL into something more pro-atherogenic and pro-thrombotic. It ferries oxidized phospholipids into the artery wall and makes plaques more inflamed and fibrotic. Lp(a) is largely hardwired by the LPA gene, so diet and exercise barely move it. That is why people with pristine lifestyles can still have early heart attacks if their Lp(a) is high.
Two measurement units are in common use. Some labs report Lp(a) as milligrams per deciliter and others as nanomoles per liter. Clinically, 50 milligrams per deciliter or 125 nanomoles per liter often marks the threshold where risk rises sharply. Because the apo(a) scarf differs in size across people, nanomoles per liter better reflects particle number and many experts prefer it for decision making.
What changed in 2025
- Long-duration RNA interference worked as designed. Lepodisiran uses small interfering RNA to turn down LPA gene expression in the liver. In Phase 2, a single 400 milligram dose dropped Lp(a) by about 89 percent on average over days 30 to 360, and two doses 180 days apart achieved about 95 percent average lowering over the same window. Injection site reactions were the most common issue and were generally mild. These are the kinds of numbers that make twice-yearly dosing plausible for routine care.
- Durability after stopping looks real. With other siRNAs in the class, Lp(a) remained well below baseline many months after the last injection, a strong sign that hepatic silencing has a long tail.
- Oral therapy is now credible. Muvalaplin, a small molecule that blocks apolipoprotein(a) from attaching to apolipoprotein B, reduced Lp(a) by roughly 70 to more than 80 percent in Phase 2, depending on the assay used. That makes a daily pill a plausible option alongside injections.
- Additional siRNAs advanced. Programs with quarterly or twice-yearly dosing reported around 90 percent median maximum reductions through 36 to 48 weeks, with Phase 3 readiness underway.
Taken together, the field crossed three thresholds in 2025: deep lowering, durable lowering, and a credible oral path. That combination turns Lp(a) from a frustrating genetic trait into a controllable risk factor. For context on how genetic risk is becoming programmable across cardiometabolic care, see our look at one-time LDL editing trends.
Why Lp(a) lowering matters for aging
Cardiovascular aging is not just about LDL cholesterol. Lp(a) accelerates the calcification and inflammation that make plaques brittle and valves stiff. In midlife and older adults, high Lp(a) stacks risk on top of everything else. Lowering it could trim the background rate of nonfatal myocardial infarction and ischemic stroke and may slow calcific aortic valve disease. The mechanistic case has been strong for years, but regulators have waited for randomized outcomes trials to show that lowering Lp(a) actually prevents events, not just changes a number. 2025 set the stage for those answers. For a broader view of aging biology turning clinical, read how CHIP becomes clinical at ESC 2025.
The road to outcomes and approval
- Pelacarsen outcomes first. The event-driven readout in secondary prevention is expected in the first half of 2026. If positive, filings could follow that year.
- Olpasiran outcomes next. The secondary prevention trial is ongoing with completion expected in the 2026 to 2027 window, depending on event accrual. Primary prevention programs are staged behind it.
- The new entrants. Lepodisiran and muvalaplin both posted compelling Phase 2 efficacy. The question now is how quickly sponsors can map dosing, durability, and safety to outcomes programs that satisfy regulators.
Regulatory scenario planning matters here. Unlike LDL cholesterol, Lp(a) does not yet have a validated surrogate that guarantees approval on biomarker change alone. A clean outcomes win for any agent would create a path for class approvals. If the first readout is positive in 2026, a United States launch in 2027 is realistic, with additional agents following on staggered timelines.
The case for universal one-time testing
When a lever is this simple, prevention starts with a single blood draw. Major societies recommend at least one Lp(a) measurement in adulthood, ideally with an isoform independent assay reported in nanomoles per liter. That one measurement usually stands for life because Lp(a) is genetically set and stable outside of liver or kidney disease. See the 2024 National Lipid Association focused update for practical guidance.
Practical tips for clinicians
- Order the Lp(a) test with your next lipid panel. Ask for nanomoles per liter if your lab offers both. Document the numerical result and the unit.
- Use cut points that map to risk. Most United States guidance treats 125 nanomoles per liter or 50 milligrams per deciliter as high and 75 to 125 nanomoles per liter as a gray zone where other risks tip the decision. Explain that the number reflects particle count, not something patients can diet away.
- Code it, do not eat it. Use CPT 83695 and appropriate ICD-10 diagnosis codes for elevated Lp(a) and family history so the lab bill does not boomerang back to the patient.
From data to delivery: how to avoid repeating the LDL fight
The statin era taught us how hard it is to move from evidence to everyday care. Here is a focused checklist so we do not waste a decade getting Lp(a) right.
What the Food and Drug Administration can do
- Make expectations explicit now. Publish guidance clarifying the evidentiary standard for approval and for labeling language. If outcomes are required, define the acceptable margin of benefit and key subgroups a priori so programs design to the target and avoid post hoc surprises.
- Pre-negotiate assay language. Require that labeling and risk management refer to isoform independent, traceable assays with results in nanomoles per liter. This will reduce unit confusion and payer disputes tied to assay variability.
What payers can do
- Adopt one-time universal testing coverage on day one. The test is inexpensive and it unlocks precision allocation of a high-impact therapy to the 15 to 25 percent of adults who need it. Set a single, unit-agnostic threshold with a nanomole per liter preference to minimize disputes.
- Tie authorization to a simple rule. Approve therapy for adults with Lp(a) at or above 125 nanomoles per liter and established atherosclerotic cardiovascular disease, or for very high levels above 430 nanomoles per liter regardless of history, where lifetime risk mirrors heterozygous familial hypercholesterolemia. Reassess when outcomes data arrive.
- Price for persistence. The durability of siRNA therapies means two injections per year or less. Model payment around annualized adherence rather than monthly fill behavior to align incentives with a twice-yearly rhythm.
What health systems and clinicians can do now
- Build Lp(a) into the intake. Add a once-in-life Lp(a) checkbox to every new patient lipid order set. When it is high, flag the chart with the numeric value, unit, and date so it is visible at every visit.
- Use a two-lever approach. Keep pushing LDL cholesterol to guideline targets with statins, ezetimibe, and PCSK9 inhibitors, and add Lp(a) suppression when available. Many patients will need both because Lp(a) risk is additive, not redundant. For the pipeline view of programmable lipids, see our overview of one-time LDL editing trends.
- Prepare patient messaging. Explain that Lp(a) is inherited, not a lifestyle failing. Emphasize that suppression is preventive, like a vaccine against future events, with dosing as simple as two injections per year or a daily pill if the oral option succeeds. For additional prevention context, explore CMV readout and longevity vaccines.
What about safety and equity
Safety so far has looked clean across programs, though exposure is still short compared with cholesterol drugs that have been in use for decades. Injection site reactions and mild laboratory changes have been the most common issues in trials and no major safety signals have emerged to date. Continued surveillance during Phase 3 and early commercial rollout will matter.
Equity deserves attention early. People of African ancestry have higher median Lp(a) levels and are more likely to have extreme values. That makes universal, once-in-life testing the fairest approach. It avoids selective screening that misses those without family histories or obvious risk factors and reduces the chance that communities with higher average levels are underdiagnosed.
Timelines you can plan around
- 2026: First outcomes readout expected from pelacarsen in secondary prevention. If positive, regulatory filings could follow in the second half of 2026.
- 2026 to 2027: Additional outcomes data expected from other programs, including olpasiran, with primary prevention studies planned behind them.
- 2027 and beyond: Staggered launches if outcomes are favorable, followed by label expansions as primary prevention and subgroup data mature.
What to do this quarter
- If you are a clinician: add Lp(a) to your next 100 lipid orders, specify nanomoles per liter, record the value permanently, and counsel patients at or above 125 nanomoles per liter about aggressive LDL control now and Lp(a)-targeted therapy as trials read out. Use CPT 83695 and the appropriate diagnosis codes to normalize reimbursement.
- If you are a health plan: publish a coverage bulletin that greenlights once-per-lifetime testing and outlines a simple authorization path tied to numeric Lp(a) and clinical history. Set your internal analytics to track disparities and close them.
- If you influence policy: prepare a fast-follow quality measure that credits clinics for one-time testing and for offering suppression to eligible patients once an agent is approved. Make the measure unit-agnostic but nanomole per liter aware.
The bottom line
Cardiology has been waiting for a lever that is both genetic and practical. The 2025 data show that Lp(a) fits that bill. We can detect it with one test. We can suppress it deeply with two injections a year or perhaps a daily pill. And we will soon know if this translates into fewer heart attacks and strokes. If we plan carefully now, we can move from trials to clinics without a decade of friction. That would make Lp(a) suppression the next real-world longevity lever, not an idea waiting on the shelf.