Midlife Inflection: The Vascular-First Longevity Playbook
A 2025 multi-organ proteomics atlas reveals a midlife inflection and puts vascular health at center stage. This practical playbook gives readers in their 40s and 50s measurable steps, endpoints, and tools to add healthy years.
Breaking: the atlas that moves longevity to the bloodstream
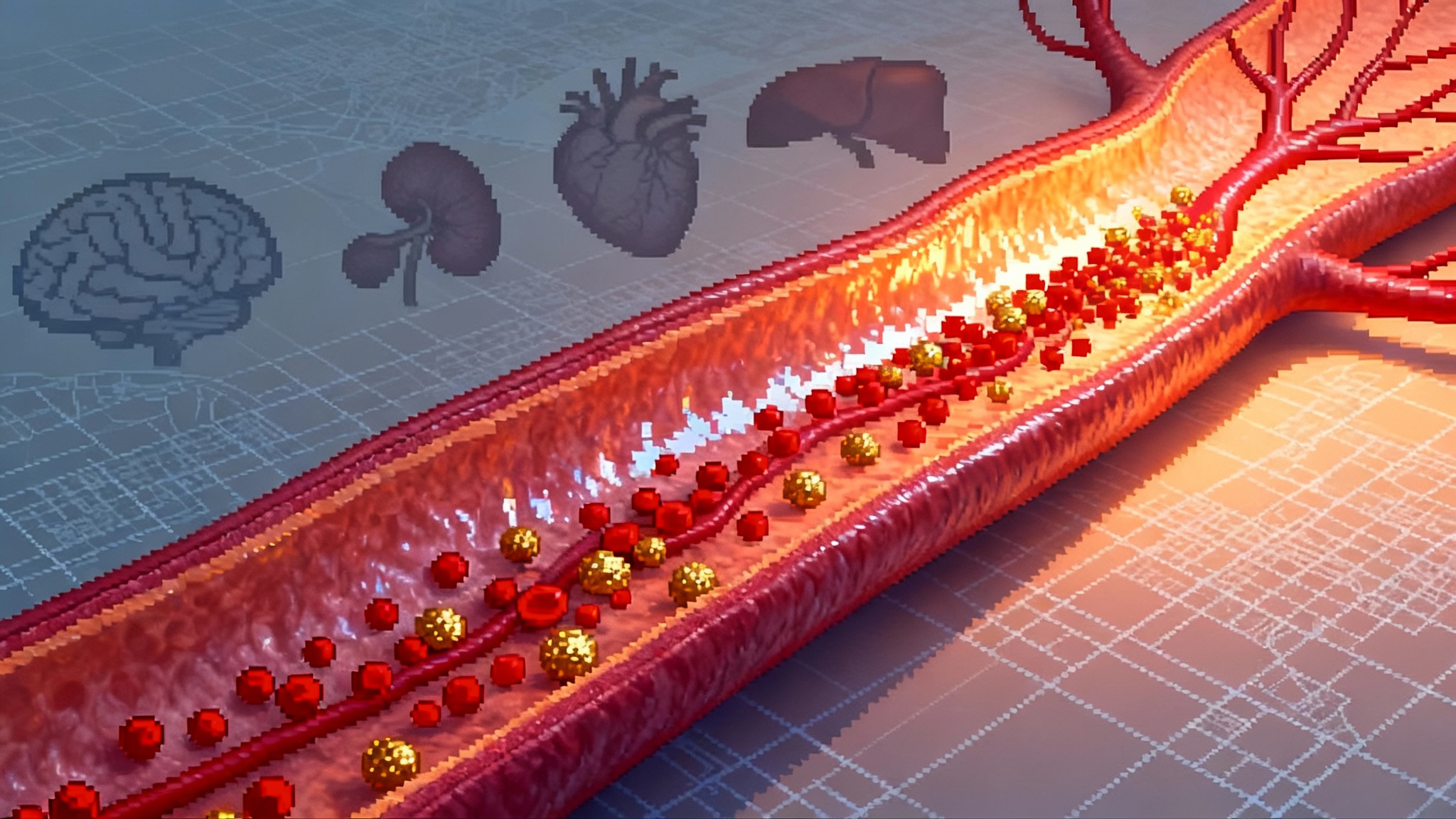
Every field has a moment when the map changes. In 2025, aging research got one. A new multi-organ human proteomics atlas across 13 tissues charted how proteins shift across the lifespan. The headline is not subtle. The curves bend sharply in midlife, roughly around age 50, and the earliest and strongest signal travels through the vasculature. The authors built tissue-specific proteomic age clocks, picked up evidence of proteostasis breakdown and amyloid load, and flagged candidate senoproteins with outsized roles in blood vessels. If you want to add healthy years, start with the pipes that feed every organ. That is the thesis behind a vascular-first longevity strategy, and the new data makes it hard to ignore. The 2025 human proteome atlas lays down the evidence.
Think of your body as a city. Proteins are the vehicles and cargo, roads are blood vessels, and intersections are the endothelial cells that decide who passes and who waits. In childhood and early adulthood, the traffic system is smooth. In midlife, subtle congestion appears. Trucks idle at on-ramps, a few exits crumble, and detours add friction. That is what the atlas shows at the molecular level. Protein traffic shifts in patterns that point to the endothelium and its surrounding matrix as early bottlenecks. If the roads falter, every neighborhood dims.
The key signal: a midlife bend in the curve
The atlas does two important things for everyday decision makers in their 40s and 50s.
- It identifies a midlife inflection, not a slow, uniform slide. That matters, because inflections are the best places to intervene. Small course corrections there yield the biggest downstream change.
- It elevates vascular aging from supporting actor to lead. Blood vessels are not just a passive delivery system. They sense shear stress, regulate inflammation, manage coagulation, and coordinate repair. When they go first, brain, heart, kidney, and metabolism follow.
Mechanistically, several themes connect to the vasculature. With age, proteins involved in complement activation, coagulation, extracellular matrix remodeling, and cellular senescence drift upward. The atlas highlights a set of plasma proteins whose tissue origins map back to vessel walls. One candidate axis features GAS6 and its receptor AXL, which together govern cell survival, efferocytosis, and inflammatory tone. Emerging evidence that aging blood clones drive vascular inflammation is rapidly moving into practice; see CHIP becomes clinical in 2025. This is a shift in where the signal is strongest and where to aim if your goal is to alter the slope of aging.
From generic anti-aging to vascular-first prevention
Most anti-aging talk floats above the ground. Supplements promise everything and commit to nothing. Vascular-first is the opposite. It is a pragmatic bundle of measurable endpoints, widely available tools, and near-term readouts that together nudge arteries, arterioles, and capillaries toward a younger phenotype. The benefit of targeting the vasculature first is compounding. Better endothelial function improves exercise capacity. Lower arterial stiffness reduces cardiac afterload. Cleaner microcirculation supports cognition and kidney filtration. The wins add up.
Below is a simple, clinic-ready playbook designed for midlife. It starts with screening you can do now, sets near-term endpoints you can move in months, and previews a pipeline of drugs and devices to watch through 2026.
Step 1: Screen in midlife like a systems engineer
The goal is to estimate your vascular age and identify the most moveable bottlenecks. Do not guess. Measure.
1) Digital vascular age from wearables
- What it is: Photoplethysmography, the pulse sensor in many watches and rings, captures waveforms shaped by arterial stiffness and endothelial tone. Modern models can convert this into a vascular age estimate and a gap from your calendar age. In a 2025 analysis using United Kingdom Biobank data, a larger positive vascular age gap predicted higher rates of cardiovascular and metabolic events, while a younger gap predicted protection. See methods in AI-derived vascular age.
- How to use it: Collect at least two weeks of resting data under consistent conditions. Record the vascular age gap and its variability. Treat big day-to-day swings as noise and focus on weekly medians.
2) Imaging that sees vessel health
- Coronary artery calcium scoring remains the best low-radiation snapshot of plaque burden for many adults over 45. A zero suggests low near-term risk, while rising scores focus attention on lipids, blood pressure, and inflammation.
- Carotid ultrasound measures intima-media thickness and detects plaque. It is noninvasive and repeatable.
- Retinal microvasculature photography provides a window on small-vessel health. Changes in arteriolar and venular caliber often track with systemic risk.
- For select cases, brain perfusion with arterial spin labeling or functional tests of endothelial reactivity can add context, especially with a family history of early stroke or cognitive decline.
3) Blood and proteome panels
- Classical labs with vascular impact: ApoB for atherogenic lipoproteins, lipoprotein(a), high-sensitivity C-reactive protein, fasting insulin or oral glucose tolerance pattern, cystatin C, urine albumin-to-creatinine ratio. For background on targeting Lp(a), see Lp(a) suppression goes mainstream.
- Proteome-based risk: Affinity panels can quantify hundreds to thousands of proteins. When interpreted in context, rising complement factors, matrix metalloproteinases, von Willebrand factor, and adhesion molecules can signal endothelial stress. Some labs and clinics now offer composite proteomic age scores. Use them for trendlines rather than labels. If you are curious about plasma interventions, see plasma exchange into testable biology for a science-first view.
4) Blood pressure and stiffness metrics at home
- Combine an automated home blood pressure cuff with a validated pulse wave velocity or augmentation index device if available. Morning and evening averages over two weeks are more useful than a single clinic reading.
Outcome of Step 1: a baseline portfolio
- Vascular age gap from wearables
- One structural marker such as coronary calcium score or carotid ultrasound
- A lab panel that includes ApoB and inflammation markers, with optional proteomics
- Home blood pressure and, if possible, pulse wave velocity
This portfolio becomes your scoreboard for the next 12 months.
Step 2: Choose near-term endpoints you can move in 6 to 18 months
Pick endpoints that respond to action, not just time. Aim for clear before-after comparisons.
- Digital vascular age gap: Your first target is directionality. A younger weekly median gap over 3 to 6 months is a promising sign. Sustained improvements over 12 months are better.
- Arterial stiffness: Carotid-femoral pulse wave velocity and augmentation index should trend down with aerobic conditioning, weight loss, and blood pressure control.
- Organ stiffness by magnetic resonance elastography: In the liver and potentially kidneys, lower stiffness often tracks with less fibrosis and better metabolic control. In the heart, strain and diastolic parameters can serve a similar role where MRE is not available.
- Plasma proteome signatures: On repeated testing, look for reductions in complement and thromboinflammatory proteins, and a shift toward a younger proteomic age clock if your lab offers one.
- Classic risk anchors: ApoB below 60 to 80 mg per deciliter for high-risk profiles, lower if you already have plaque. Home blood pressures predominantly under 130 over 80 mm Hg with low variability. Hemoglobin A1c under 5.7 to 6.0 percent if safely achievable.
Document a baseline, commit to a 6-month check, and plan a 12-month readout. Treat it like a product launch cycle.
Step 3: Interventions that move those endpoints
None of the following is a substitute for medical care. These are levers known to change the scoreboard you just built. Work with a clinician who understands cardiometabolic risk and is comfortable with data.
1) The cardiometabolic stack: GLP-1 plus SGLT2
- For people with obesity or prediabetes or type 2 diabetes, glucagon-like peptide 1 receptor agonists improve weight, blood pressure, and inflammatory markers, and have shown cardiovascular risk reduction in multiple large trials. Oral semaglutide reported a significant reduction in major adverse cardiovascular events in high-risk type 2 diabetes in 2025 results. Sodium glucose cotransporter 2 inhibitors consistently improve heart failure and kidney outcomes across varied populations. Together, they address arterial stiffness, cardiac afterload, and metabolic toxicity.
- Practical guidance: Start with one class, titrate, then consider layering under clinician supervision. Monitor kidney function, electrolytes, and blood pressure during the first months. Expect meaningful changes in resting heart rate variability and vascular-age estimates as weight and glycemia improve.
2) ApoB-first lipid strategy
- ApoB is the particle count behind atherosclerosis. Lower is safer. If you have plaque or diabetes, a statin backbone plus ezetimibe or a PCSK9 inhibitor can push ApoB into the protective range. That cascades into slower calcium score growth and a lower event rate. Recheck ApoB 6 to 8 weeks after any medication change.
3) Blood pressure with low variability
- Aim for a morning average under 130 over 80 with minimal day-to-day swing. Angiotensin receptor blockers or angiotensin converting enzyme inhibitors are effective baselines. Add a thiazide-like diuretic or a calcium channel blocker if needed. Titrate based on home logs, not occasional clinic spikes.
4) Exercise that reverses stiffness
- Two to four hours per week of zone 2 aerobic work trains the endothelium and improves mitochondrial efficiency. Add one or two short interval sessions to challenge shear stress responses. Resistance training twice weekly improves insulin sensitivity and supports arterial health when combined with aerobic work. Measure progress by changes in heart rate at a fixed pace, pulse wave velocity, and your wearable’s vascular-age trend.
5) Anti-inflammatory hygiene
- Address periodontal disease and sleep apnea. These are surprisingly potent vascular irritants. If you have established coronary disease, a clinician may consider low-dose colchicine, which reduces events in select populations. Do not self-prescribe.
6) Nutrition for the endothelium
- The diet that lowers ApoB and normalizes glucose is the one that works for your constraints and you will keep. That often means higher protein, fewer refined starches, more fiber, and regular meals that avoid wild glucose excursions. Track with a glucose meter for two weeks if you have risk factors. If weight loss is a goal, set a 12-week target and stop when you hit it. Lingering in weight-loss mode becomes counterproductive.
7) Microcirculation care
- Heat therapy, brief sauna sessions if you tolerate them, and walking after meals improve microvascular flow. If you are desk-bound, a timer that enforces five-minute movement breaks every hour is not trivial. Capillaries do not care about your calendar.
The forward-looking pipeline to watch through 2026
The atlas points to protein networks that line up with several drug classes already in late-stage trials or real-world use.
- GAS6 and AXL modulators: This axis coordinates efferocytosis and inflammation resolution. AXL inhibitors are being studied in oncology and fibrosis, and next-generation modulators could tilt endothelial repair and immune tone. Expect early mechanistic readouts in fibrosis and vascular complications before primary prevention trials arrive.
- Complement pathway agents: C3 and C5 inhibitors, factor B and D inhibitors, and antisense oligonucleotides to upstream proteins are moving in kidney and hematologic disorders where complement overdrive damages microvessels. Positive renal and vascular signals here would support targeted use in high-risk inflammatory vascular phenotypes.
- Anti-SAP and anti-amyloid approaches: Serum amyloid P component stabilizes amyloid deposits. Programs that deplete SAP or destabilize fibrils in systemic amyloid diseases may inform broader strategies for age-linked vascular amyloid. The atlas’s proteostasis signal makes this a space to watch, even as programs evolve.
- Endothelial repair and barrier integrity: Cell-free vesicles, engineered exosomes, mRNA delivery of endothelial nitric oxide synthase, and small molecules that reinforce junction proteins are moving from preclinical to early human studies. Expect narrow disease applications first, but the principle is general: restore the barrier, quiet the immune noise, and flow improves.
- Cardiometabolic next wave: Incretin combinations, long-acting amylin analogs, and peripherally selective agents that spare resting heart rate are in the queue. The practical takeaway is simple. The cardiometabolic stack is getting stronger and more tolerable, which makes vascular-first prevention easier to sustain.
How to run your personal midlife trial
You do not need a lab coat to make this rigorous.
- Define your cohort of one: age, family history, prior imaging, and a three-sentence risk story.
- Set your endpoints: choose three from digital vascular age gap, pulse wave velocity, ApoB, home blood pressure variability, and a proteomic or inflammatory panel.
- Pick your interventions: select two to three from the list above that match your profile and constraints. Put medications under clinician guidance.
- Schedule your readouts: at 6 months and 12 months, repeat the same tests under similar conditions.
- Decide with data: keep what moved your endpoints, drop what did not, and avoid adding five new variables at once.
Why this matters now
The next 12 to 18 months will bring more cardiometabolic outcomes, maturing kidney and heart failure data for combination therapy, and mechanistic readouts from complement and endothelial repair programs. None of that requires waiting to act. The 2025 proteome atlas already says where to look and when to move. The most valuable years for intervention are the late 40s and early 50s, when the curve bends and small changes travel far.
There is a big idea tucked inside all the measurements. Longevity is not an abstract fight with time. It is a concrete project to rebuild and maintain the network that every other organ depends on. Make your roads younger, and the city comes back to life.