CHIP Goes Mainstream: Slowing Aging Clones to Protect Hearts
{"excerpt":"Fresh 2025 data suggest low-dose colchicine can slow growth of TET2-driven clonal hematopoiesis while new studies link CHIP to heart failure and mortality. The case for adding inexpensive CHIP genotyping to routine cardiometabolic care is now strong."}

The 2025 signal: aging blood clones can be slowed
If you follow cardiology, you have probably seen the phrase clonal hematopoiesis of indeterminate potential. Clinicians shorten it to CHIP. It describes small groups of blood stem cell descendants that carry acquired mutations and grow faster than their neighbors. In August 2025, researchers reported that a common anti-inflammatory pill, low-dose colchicine, appeared to slow the growth of these aging clones, especially when the driver mutation was TET2. That signal came from a prespecified genetic substudy inside a large outcomes trial and matters for a simple reason. If inflammation helps these clones expand, then taming inflammation may curb both the clones and the cardiovascular risk that tracks with them. You can read the methods and numbers in the peer reviewed LoDoCo2 genetic substudy.
That finding reframes clonal hematopoiesis from an ominous passenger to a target. We already knew colchicine reduces cardiovascular events in chronic coronary disease. Now we have early human evidence that the same drug may slow the biological engine that makes some CHIP clones dangerous. This builds on our vascular-first longevity playbook.
What CHIP actually is, in plain language
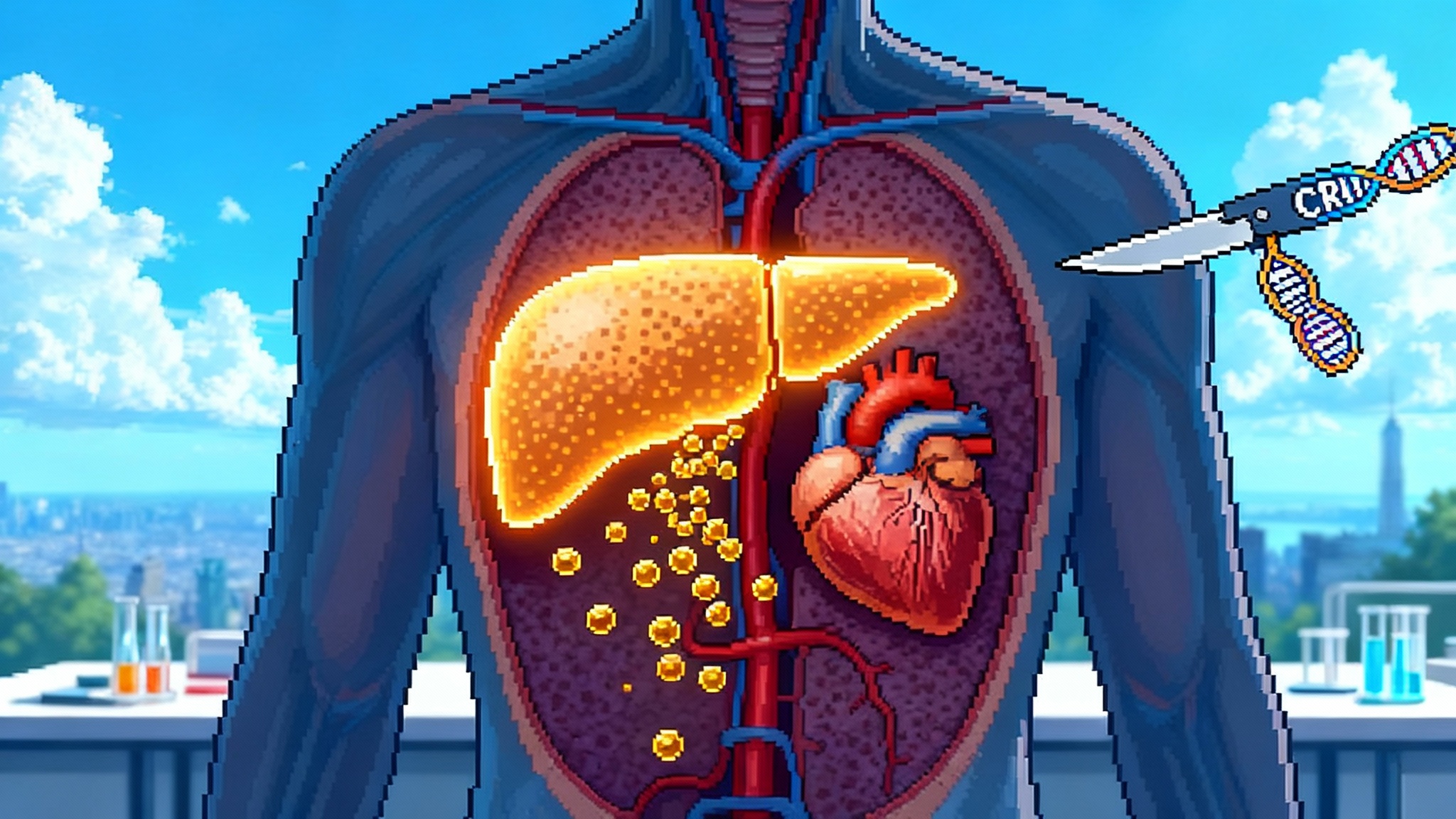
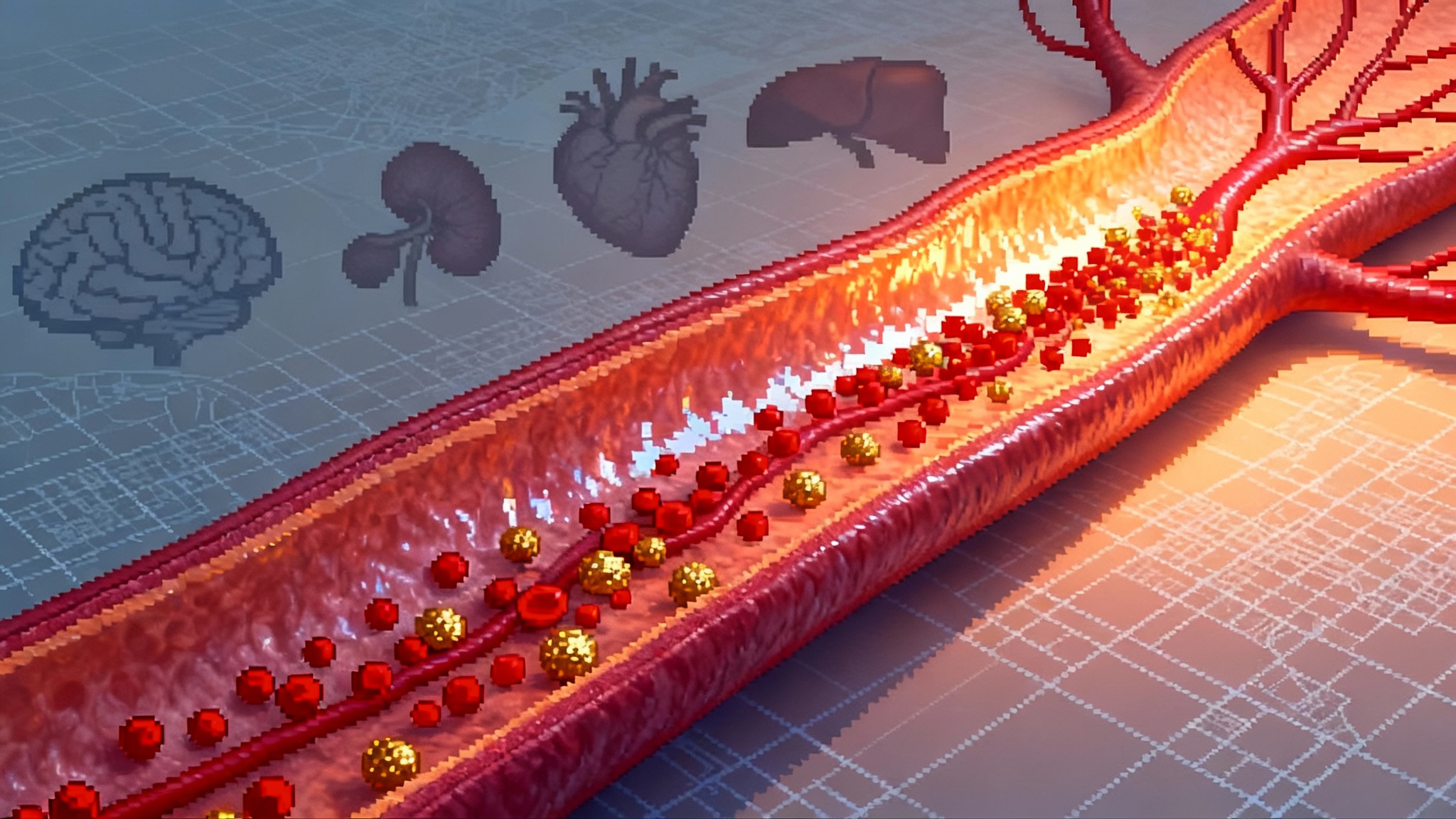
Think of your bone marrow as an orchard of lifelong trees. Each tree is a stem cell. With age, weathering and random errors, a few trees pick up a change in their bark that lets them grow a little faster. Those trees start to dominate the grove. That is CHIP. The most common changes occur in genes like DNMT3A, TET2, ASXL1, and JAK2. The fraction of blood cells derived from the altered tree is often measured as variant allele fraction. Many people carry small clones with no immediate symptoms, especially after age 60.
Why do cardiologists care? Because the altered trees secrete more inflammatory signals. In animal models and human genetics, TET2 loss turns macrophages into louder megaphones for interleukin 1 beta and interleukin 6. Those signals thicken and inflame plaque, recruit more immune cells, and destabilize lesions. The bigger the clone, the louder the signal. That link between clone size and inflammation is what makes the 2025 colchicine result so consequential.
The link to heart failure and mortality keeps firming up
For years, CHIP has been tied to coronary disease. In 2025 we saw new work connecting CHIP to progression of cardiometabolic multimorbidity and mortality in a broad population dataset, not just in highly selected cohorts. A prospective analysis in UK Biobank reported that carriers of CHIP were more likely to accumulate multiple cardiometabolic conditions over time and had higher mortality, after adjusting for traditional risk factors. See the results in the UK Biobank prospective study.
Other 2025 analyses added texture. In older women from the Women’s Health Initiative Long Life Study, specific CHIP subtypes such as TET2, ASXL1, and JAK2 remained associated with incident cardiovascular events even into their eighties. In oncology settings, a JACC CardioOncology study of patients receiving autologous hematopoietic cell transplantation found that preexisting CHIP doubled the five-year risk of heart failure and worsened survival, and the risk climbed with larger clones. Together, these lines of evidence underscore a point with practical weight. CHIP is not a lab oddity. It is a biological lens that sharpens residual risk in many patient types.
Why inflammation is the hinge for TET2 clones
TET2 helps cells read DNA methylation marks to keep inflammatory programs in check. When TET2 is lost in a blood stem cell, its progeny make more interleukin 1 beta, interleukin 6, and other cytokines. In mice, blocking interleukin 1 beta or interleukin 6 reduces atherosclerosis driven by TET2 mutant clones. In humans, a prior secondary analysis suggested that canakinumab, which blocks interleukin 1 beta, yielded larger cardiovascular benefit in people with TET2 CHIP. The 2025 colchicine substudy strengthens the inflammation mechanism in people by showing slower TET2 clone growth under anti-inflammatory pressure. Viewed together, the biology and the clinical signals are converging.
Here is the practical translation. If you have a patient whose blood carries a growing TET2 clone, interventions that quiet macrophage inflammatory signaling may pull two levers at once. They may reduce cardiovascular events and slow the clone’s expansion. That is why this year’s readout feels like a turning point.
Actionable now: how to use CHIP in today’s clinic
You do not need a new specialty clinic to begin using CHIP information. You need a disciplined workflow, clear eligibility, and a plan to act on the result.
Who to test
- Adults 60 and older, especially with diabetes, chronic kidney disease, long smoking history, inflammatory conditions, or premature coronary disease.
- Anyone with recurrent cardiovascular events despite guideline-directed therapy, including patients with high high-sensitivity C-reactive protein or lipoprotein(a).
- Selected heart failure patients, especially with preserved ejection fraction and metabolic syndrome, where residual inflammatory risk is common.
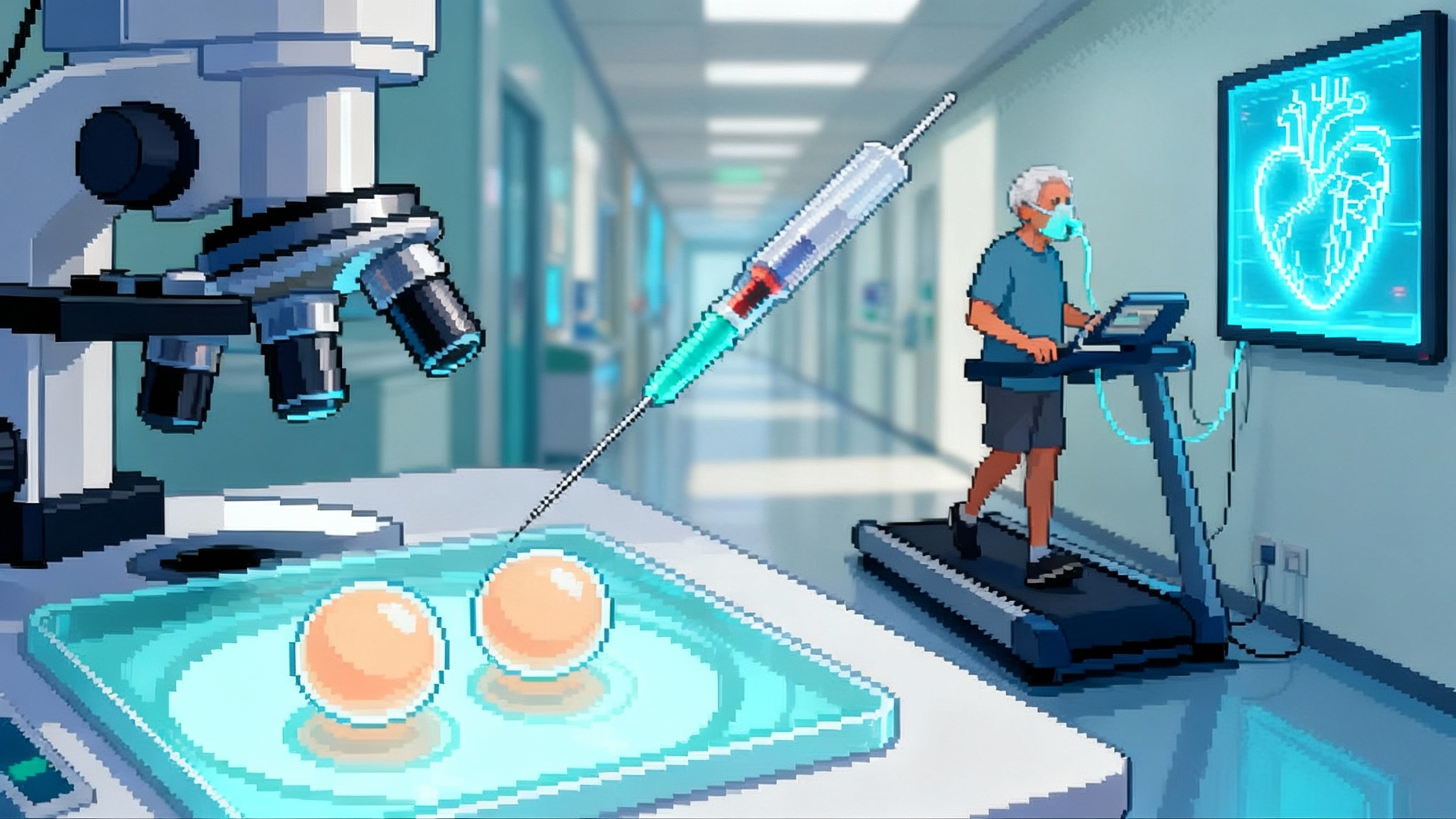
What test to order
- A targeted next-generation sequencing panel on peripheral blood that covers common CHIP genes and reports variant allele fraction. Panels that capture DNMT3A, TET2, ASXL1, JAK2, PPM1D, and TP53 are usually enough for risk stratification. The assay should reliably detect down to at least 2 percent variant allele fraction.
- If your health system does not run its own panel, most large reference labs and many academic centers do. Turnaround is usually measured in weeks, not months. Costs vary but are in the range of many lipid and imaging profiles and continue to fall as sequencing scales. For test strategy and metrics, see our trial-grade biomarker playbook.
How to interpret the result
- Any CHIP clone raises risk, but size and gene matter. Larger clones, often above 10 percent variant allele fraction, carry higher risk. TET2 and JAK2 often track with stronger cardiovascular associations than DNMT3A. Multiple clones compound risk.
- Pair the genetic readout with high-sensitivity C-reactive protein and apolipoprotein B. Inflammation plus elevated apolipoprotein B identifies the patients most likely to benefit from aggressive multipronged prevention.
How to act today
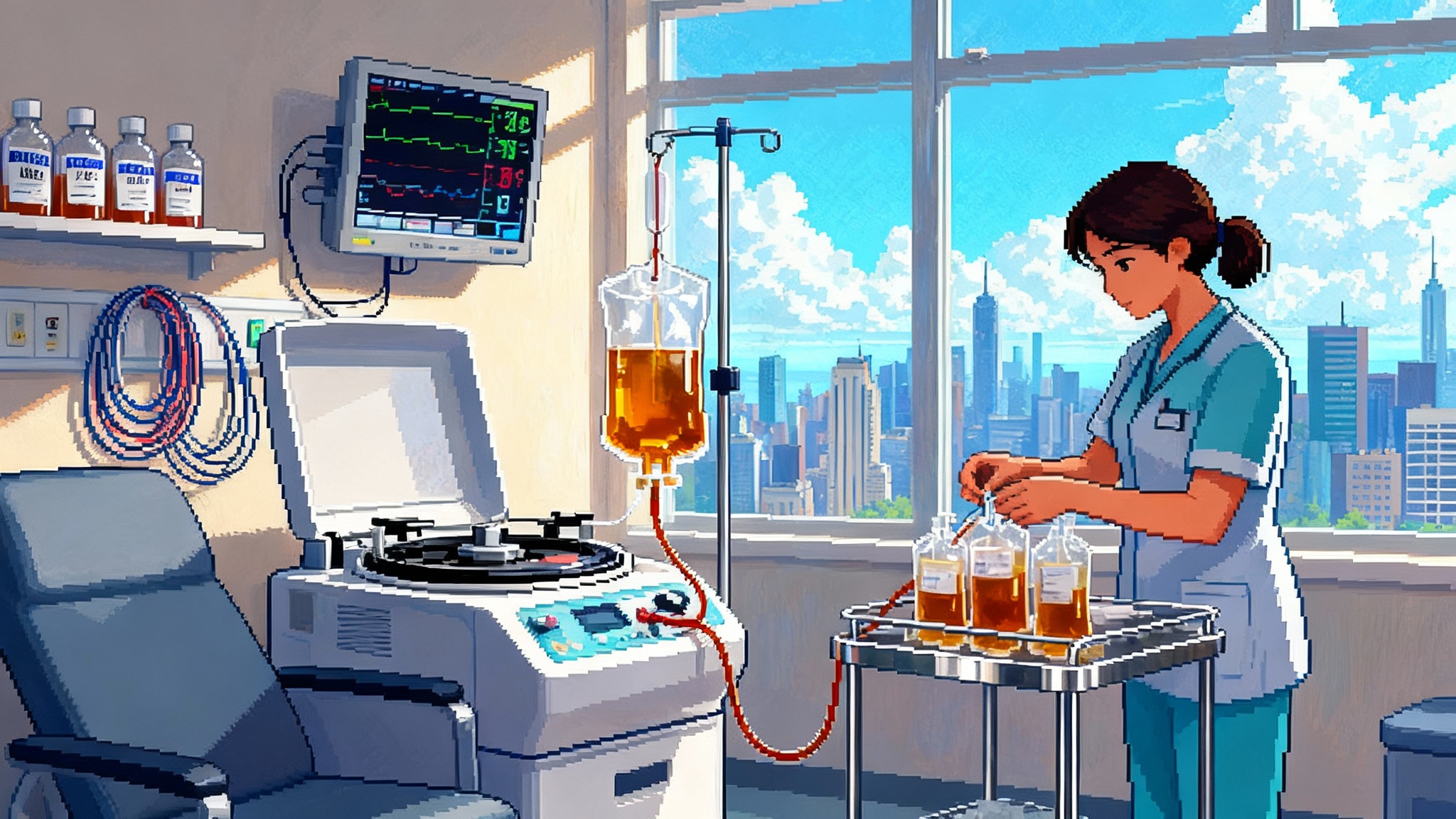
- Anti-inflammatory therapy: In patients with chronic coronary disease who meet current label, low-dose colchicine 0.5 milligrams daily reduces events and, per the 2025 substudy, may slow TET2 clone growth. Screen for drug interactions, especially strong CYP3A4 or P-glycoprotein inhibitors, and use caution in advanced renal or hepatic impairment. Recheck a complete blood count and creatinine after initiation.
- Lipid lowering: Drive apolipoprotein B as low as you safely can. Combine high-intensity statins with ezetimibe. Add a PCSK9 inhibitor such as evolocumab or alirocumab to reach targets. For the pipeline view, see one-shot PCSK9 editing.
- Glucose and weight management: For patients with diabetes or obesity, GLP-1 receptor agonists such as semaglutide or tirzepatide improve cardiometabolic profiles and reduce events in high-risk populations. Pair these with SGLT2 inhibitors in heart failure or diabetic kidney disease, which also have anti-inflammatory effects in the myocardium and vasculature.
- Lifestyle with measurable endpoints: Smoking cessation, particulate exposure reduction at home and work, sleep regularity, and resistance plus aerobic training all reduce inflammatory tone. Set numeric goals and timelines, not vague advice. Track high-sensitivity C-reactive protein alongside lipids to show progress the patient can see.
Trial enrollment right now
- Several trials are testing targeted anti-inflammatory or clone-directed strategies in people with CHIP. Examples include interleukin 1 beta blockade in TET2 CHIP with imaging of vascular inflammation and planned measurement of clone size, and oral NLRP3 inflammasome inhibitors such as dapansutrile in post–myocardial infarction patients. Look for trial identifiers in registries; for example, NCT05880355 is a current dapansutrile cardiovascular protocol.
Follow-up cadence
- Recheck clone size and high-sensitivity C-reactive protein after 6 to 12 months when you initiate or escalate anti-inflammatory therapy. Stable or shrinking TET2 clones with falling high-sensitivity C-reactive protein support that your plan is working. Growing clones despite control of traditional risk factors should trigger a trial screen or specialist referral.
What is next: from generalized to clone-directed prevention
The first wave is clear. Anti-inflammatory and lipid therapies work across many patients. The next wave is precision. Different clone types drive different biology.
-
TET2 and ASXL1 clones
- These clones raise interleukin 1 beta and interleukin 6 signaling. Several groups are testing agents that target these axes. Canakinumab blocks interleukin 1 beta. Agents that block interleukin 6 or its receptor may also help. The mouse data are strong and human signals are growing. The 2025 colchicine substudy suggests that even a simple microtubule inhibitor can dial down clone growth pressure in TET2 carriers.
-
JAK2 V617F clones
- These clones show hyperactive Janus kinase signaling and a prothrombotic state. In myeloproliferative neoplasms, ruxolitinib reduces symptoms and inflammation. Low-dose aspirin has antithrombotic benefits. It is reasonable to expect tailored prevention packages that differ by clone, once we have prospective trials.
-
Inflammasome inhibitors
- The NLRP3 inflammasome sits near the top of the danger signal cascade. Several oral inhibitors are in early cardiovascular trials. If they pan out, an NLRP3 inhibitor could become part of a combination prevention plan for CHIP carriers who have persistent inflammatory risk despite colchicine and standard care.
-
Combinations and sequencing
- CHIP control will not be a single drug. It will look like modern lipid care. Start with lifestyle and statins. Layer ezetimibe and PCSK9 inhibition for apolipoprotein B. Add colchicine when indicated. For selected patients with high-risk clones and persistent inflammation, move to an inflammasome inhibitor or cytokine blockade. Rerun the labs and watch the clones. That is the direction.
A simple clinic pathway you can adopt next month
- Identify patients 60 and older with established atherosclerotic cardiovascular disease, heart failure with preserved ejection fraction, diabetes with end-organ involvement, or high high-sensitivity C-reactive protein. Flag those with recurrent events on guideline-directed therapy.
- Order a blood-based next-generation sequencing panel that covers common CHIP genes and reports variant allele fraction. Add high-sensitivity C-reactive protein and apolipoprotein B. Document a plan to act on positive results.
- If CHIP is present, classify by gene and size. Add a CHIP line to the problem list and include variant allele fraction. Counsel the patient that this is a risk marker you can act on, not a sentence.
- Start or intensify risk-factor control. Use low-dose colchicine in chronic coronary disease when on label and tolerated. Drive apolipoprotein B down with stacked therapy. Optimize glucose and weight with modern agents when appropriate. Write down a 12-week target and schedule follow-up.
- Screen for trials if the clone is large or growing, or if inflammation remains high after standard steps. Offer a trial referral the same way you would offer cardiac rehabilitation.
- Reassess in 6 to 12 months. Repeat high-sensitivity C-reactive protein, apolipoprotein B, and, if feasible, clone size. Adjust the plan to biology rather than to habit.
Economics and ethics, without hand waving
Cost matters. Sequencing has dropped in price to the point where a focused CHIP panel is comparable to other specialty blood work. The downstream costs are familiar and often generic. Colchicine is inexpensive. Statins and ezetimibe are generic. Even PCSK9 inhibitors have seen price reductions since launch. What is new is the idea that you can measure a clone, act, and measure again. That creates accountability. If clone size and inflammation do not move, you try something else or refer to a trial.
Equity matters. Black and Hispanic patients suffer higher burdens of cardiometabolic disease and often have less access to specialty prevention. Because CHIP is common and testable, it can be a leveling technology if embedded in safety net systems and if payers recognize it as a risk stratifier. The workflow above is designed to run in primary care or cardiology, not only at academic centers.
Counseling matters. A CHIP finding can raise anxiety about blood cancers. The absolute risk of progression to leukemia is small for most carriers, especially with small clones and without cytopenias. Make that clear up front. Emphasize that the point of testing is to identify a modifiable risk pathway that links to heart and metabolic health.
The new narrative: somatic mosaicism as a longevity lever
For decades, cardiometabolic care focused on lipids, blood pressure, and glucose, then on thrombosis and renin angiotensin signaling. Inflammation was the residual risk everyone talked about but could not personalize. CHIP turns that into something you can see, label, and track. This year’s evidence suggests you can also slow its worst actor, the TET2 clone, with a pill that costs less than a morning coffee in most cities. That changes the attitude at the bedside.
The bigger picture is even more interesting. We are watching cardiology and hematology merge around a shared idea. Somatic mosaicism is not fate. It is a dial. If we pair inexpensive genotyping with targeted anti-inflammatory and lipid therapies today, and add clone-directed drugs tomorrow, we can turn that dial toward longer, healthier lives. For related frontiers in gene control, see [epigenome editing enters humans](/epigenome-editing-enters-hum longevity’s-next-switch). The orchard does not need to be perfect. It needs to be tended. In 2025, we finally got the first proof that we can prune, and the grove responds.