One-Shot PCSK9 Editing Could Recode Heart Disease Risk
In 2025, first-in-human data, Fast Track status, and a major pharma deal pushed one-time PCSK9 base editing from theory to clinical reality. Here is how a single dose could compress lifetime LDL exposure and what must still go right.
Breaking news for prevention
A single infusion that meaningfully lowers low-density lipoprotein cholesterol for years, maybe decades, has now moved from theory to human data. In April 2025, Verve Therapeutics reported initial results from its Heart-2 Phase 1b study of VERVE-102, an in vivo base editing medicine designed to turn down the PCSK9 gene in the liver. Among the first 14 participants, the company saw dose-dependent reductions in circulating PCSK9 and a mean 53 percent drop in LDL cholesterol at the top tested dose, with a maximum individual reduction of 69 percent and no treatment-related serious adverse events reported in that dataset. These are small, early numbers, but they are the first human sign that a one-time edit might produce durable lipid control. Verve's April 14, 2025 update.
The U.S. Food and Drug Administration granted VERVE-102 a Fast Track designation in April, and the company outlined a clear near-term plan: finish dose escalation with durability readouts in the second half of 2025 and start a Phase 2 trial that includes U.S. sites. If these steps hold, mid-decade could mark the first large clinical test of whether a single dose can compress lifetime atherosclerotic cardiovascular disease risk in real patients rather than models.
Why PCSK9 and why base editing
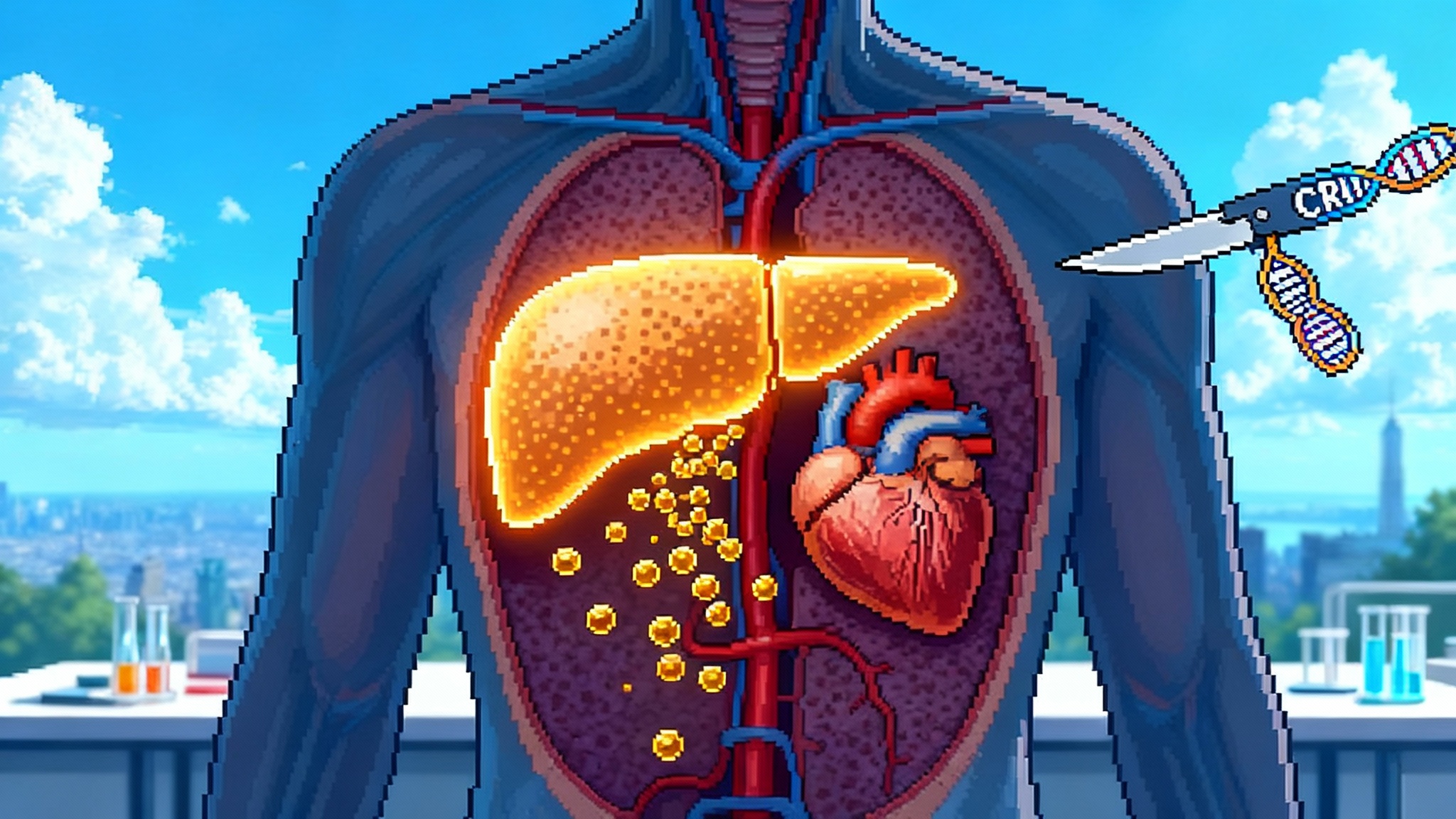
PCSK9 is a liver-produced protein that tags LDL receptors for degradation. Fewer receptors means slower clearance of LDL particles from the bloodstream. Families with rare loss-of-function variants in PCSK9 tend to have very low LDL levels and a dramatic reduction in coronary events. That human genetic backdrop makes PCSK9 a natural target for therapies that aim for long-term LDL reduction.
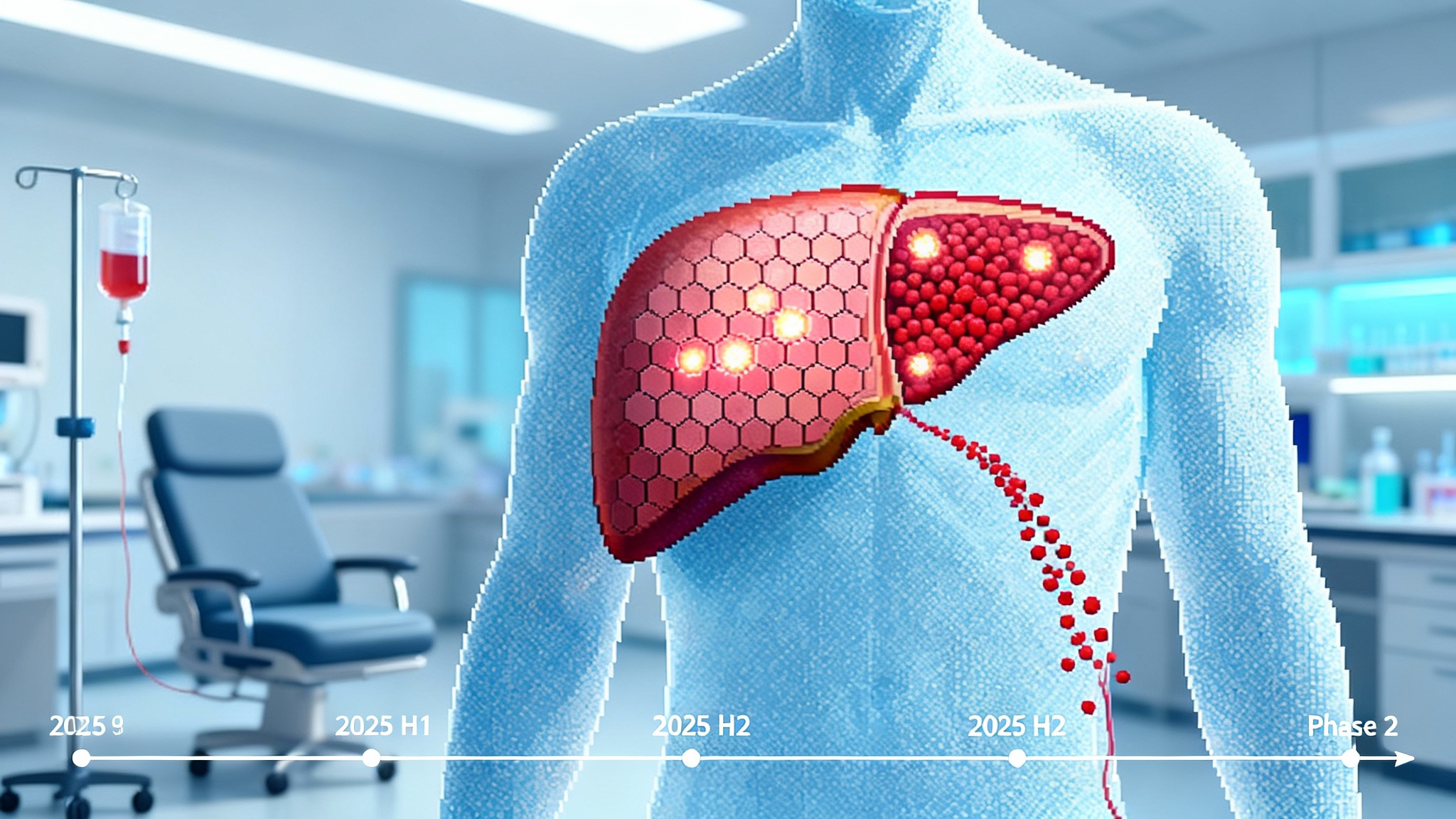
Base editing is a form of gene editing that swaps a single DNA letter without cutting both strands of the genome. Think of it as a pencil eraser rather than scissors. Verve’s candidate uses a messenger RNA payload and a guide RNA in a lipid nanoparticle that homes to hepatocytes, the liver’s workhorse cells. The mRNA is translated into the base editor inside the cell, the edit is made at the PCSK9 locus, and the editor machinery degrades within hours to days. The cell keeps the result, not the tool. For a prevention therapy, that is the point. The treatment is a moment in time, but the benefit could endure as edited cells divide and replace older ones. For broader context on gene control at scale, see our piece on how epigenome editing enters humans.
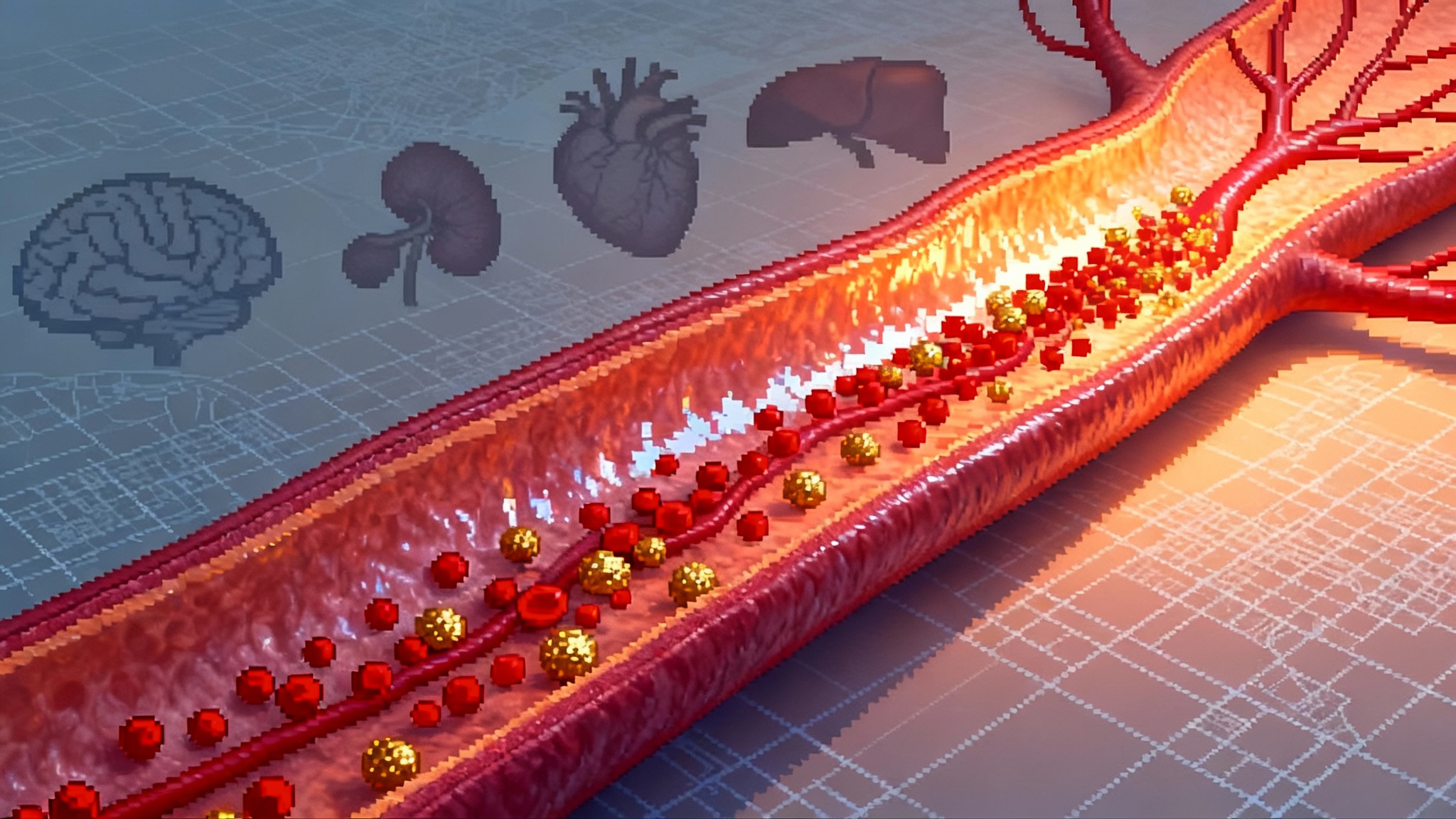
From lifetime exposure to lifetime control
Cardiovascular risk tracks with the area under your LDL curve. Imagine cholesterol as a faucet dripping into your arteries. Over decades, the bucket fills and hardens with plaque. Medicines that briefly turn the faucet down do help, but if the flow creeps back up between doses or adherence fades, the bucket still fills. A single edit that clamps the faucet to a lower setting early in midlife would change the geometry of risk. Even if your LDL is only 50 to 60 milligrams per deciliter lower than it would have been, the cumulative exposure over 20 to 30 years drops by a large margin. This is what compressing lifetime risk means in practice. For the prevention frame, see our vascular-first longevity playbook.
The 2025 momentum
Three milestones in 2025 turned this from a niche trial story into a credible roadmap for preventive gene therapy:
- First efficacy and safety readout in humans. The Heart-2 data showed a clean short-term safety profile in the early cohorts and sizable LDL reductions after a single infusion.
- U.S. regulatory traction. Fast Track status and plans to run Phase 2 with U.S. sites signal appetite to evaluate this class in a larger, more diverse population.
- Big pharma validation. In June, Eli Lilly said it would acquire Verve Therapeutics for up to 1.3 billion dollars, citing the promise of CRISPR-derived cardiometabolic medicines and the potential to bring a one-time PCSK9 therapy into mainstream care. Reuters on June 17, 2025.
This combination of clinical signal, U.S. regulatory progress, and strategic capital is what moves a field from intriguing to inevitable. It does not guarantee success, but it draws the map for the next tests that matter.
How it stacks up against the status quo
A fair comparison must consider potency, durability, adherence, and logistics.
-
Statins. Statins are the backbone of lipid management. They are inexpensive and reduce LDL by roughly 30 to 50 percent depending on agent and dose. Their real-world challenge is adherence over decades. People stop and restart. Doses get lowered after side effects. When taken consistently, statins save lives. When they are not, the LDL faucet creeps back up.
-
PCSK9 monoclonal antibodies. Amgen’s evolocumab and Regeneron and Sanofi’s alirocumab inhibit circulating PCSK9 and can lower LDL an additional 50 to 60 percent on top of statins. They work quickly and are well studied, but they require lifelong injections every 2 to 4 weeks and continued prior authorizations. For secondary prevention, many patients and clinicians make this work. For primary prevention in midlife, persistent usage outside specialty care remains uneven.
-
Twice-yearly RNA interference. Inclisiran silences the PCSK9 message inside hepatocytes. After two initial doses, it is administered every six months and delivers sustained lowering without frequent injections. That schedule improves adherence versus a daily pill but still relies on repeat clinic visits or coordinated pharmacy programs.
-
One-time base editing. If a single visit produces a multi-year or permanent reduction, adherence becomes a solved problem. There is no refill, no calendar reminder, no insurance renewal. The active question shifts from will people stay on therapy to who should receive it, when, and under what monitoring plan. For a parallel one-and-done strategy in another protein misfolding disease, see how CRISPR is switching off TTR.
Two elements could make base editing uniquely powerful in prevention. First, the biology targets the origin of the disease process in the liver rather than blocking PCSK9 protein after it is secreted. Second, durability could be measured in years rather than months, and perhaps in decades if edited hepatocytes persist and repopulate the liver. On the flip side, reversibility is limited. You cannot easily turn an edit off, which raises the safety bar and the need for rigorous selection criteria.
The safety questions that still need answers
Early data suggest an acceptable short-term safety profile, but the field must show answers to four questions before base editing can move into primary prevention for millions of midlife adults.
-
Off-target edits. Base editors can make unintended changes at sequences that resemble the target site. Preclinical studies use genome-wide assays to screen for these events, but human relevance hinges on deep sequencing of on-target and potential off-target loci in trial participants. What to do: expand unbiased and hypothesis-driven genomics in clinical protocols, report rates of off-target changes across dose cohorts, and track whether any off-targets fall in tumor suppressors or oncogenes.
-
Durability and dose. How long do LDL reductions last after a single infusion, and how much variability is there between individuals. If a portion of patients drift back toward baseline after a few years, the value proposition changes. What to do: show multi-timepoint LDL and PCSK9 protein trajectories and couple that with periodic liver biopsy or cell-free DNA measurements in a substudy to corroborate edit persistence.
-
Hepatotoxicity monitoring. Lipid nanoparticle delivery concentrates editing in hepatocytes, which is the goal and also the risk. Transient jumps in liver enzymes are manageable if they resolve, but rare serious injury would be unacceptable in a preventive setting. What to do: standardize a hepatology monitoring bundle that tracks alanine aminotransferase, aspartate aminotransferase, bilirubin, platelets, and coagulation, with predefined thresholds for intervention and a structured adjudication process across trial sites.
-
Immunogenicity. Even transient editor expression could trigger immune responses. Repeat dosing may be unnecessary, but if a second dose is ever considered, immunity to the editor protein could block benefit or create risk. What to do: integrate baseline and post-dose immune profiling, including anti-editor antibodies and T cell assays, and publish whether these correlate with safety or efficacy.
Who should be first in line
The initial priority is not every healthy 45-year-old with a borderline lipid panel. A reasonable first wave includes:
-
Heterozygous familial hypercholesterolemia. People with genetically confirmed or clinically probable HeFH who struggle to achieve targets or maintain adherence. They face high lifetime risk despite best efforts.
-
Premature coronary artery disease. Adults who had coronary events in their 40s or 50s and whose LDL control requires multiple agents. Editing could simplify their regimen and sustain control.
-
Select high polygenic risk. Individuals with elevated polygenic risk scores and persistent LDL elevation despite therapy could be studied in carefully designed trials, especially if imaging shows early plaque.
For primary prevention in midlife, the evaluation needs a transparent consent process. Patients must see not only the expected LDL reduction but the open questions. That means clear discussion support tools, shared decision-making, and a path to step back if subsequent trials reveal new safety signals.
How payers could make this work
A one-time prevention therapy will not fit chronic-drug spreadsheets. Four payer models could be tested:
- Outcomes-based annuity. Spread the price over five to seven years and tie payments to LDL reduction and event-free status at predefined checkpoints.
- Warranty pricing. A high upfront payment with partial rebates if LDL lowering below a preset threshold is not maintained at year two and year three.
- Bundled prevention episodes. Pair the edit with coronary calcium scoring, statin therapy as needed, and a structured lifestyle program, and reimburse as a package aimed at primary prevention in midlife.
- Age-gated coverage. Begin with coverage for adults aged 40 to 55 with HeFH or documented premature coronary disease and expand eligibility as longer-term data arrives.
These are not speculative finance tricks. They are ways to align incentives for a therapy whose benefits compound over decades while costs hit on day one.
The near-term roadmap that will decide everything
What happens between now and the end of 2025 will set the tone for the decade:
- Second half of 2025. Final dose-escalation and durability data from Heart-2. Expect more participants at higher doses, longer follow-up, and clarity on the range of LDL reductions and variability.
- Second half of 2025. Phase 2 initiation with U.S. enrollment. This is the first chance to test broader inclusion criteria, standardized safety monitoring, and site readiness in a system where most lipid care is delivered by primary care clinicians.
- Big pharma integration. If the Lilly transaction closes as planned, watch for how a large cardiometabolic portfolio integrates a preventive gene therapy. Manufacturing scale, payer negotiations, and field education will all accelerate under a larger umbrella.
- Competitive signals. Other companies are advancing in vivo editing for lipid genes such as ANGPTL3 and LPA. The first to show clean, durable data in a randomized setting will shape guideline debates about moving editing into primary prevention.
What would it take to shift primary prevention in midlife
By 2027 or so, guideline committees and payers will ask for three kinds of evidence:
- Durability at scale. Two to three years of follow-up that shows stable or improving LDL reductions without drift, across hundreds of participants and multiple sites.
- Safety with headroom. No signal of persistent hepatotoxicity, no pattern of concerning off-target edits, and no clustering of immune events. There must be enough headroom to justify treating otherwise healthy midlife adults who may not see a personal event risk for 10 to 20 years.
- Practicality and equity. A care pathway that primary care teams can run. That means standardized referral criteria, straightforward counseling materials, clear lab monitoring schedules, and payment models that do not lock out community clinics or underinsured patients.
If those three pillars stand, a one-time PCSK9 edit could become the first true preventive gene therapy in longevity medicine. It would not replace statins, monoclonals, or RNA interference drugs overnight. It would offer a new choice for people with high lifetime risk who want to do one definitive thing in their 40s or 50s to change their trajectory.
What to watch at the next readouts
- The slope of LDL reduction over time. Does LDL continue to fall from week four to month six as editing completes and hepatocytes turn over, or does it plateau earlier.
- Variability by dose. How tight is the distribution at the top dose. A therapy that gives most people a 50 to 60 percent reduction is easier to operationalize than one with wide swings.
- Lab signals. Liver enzymes, platelets, and bilirubin across larger numbers and longer follow-up. A flat safety profile unlocks primary prevention far more than another 5 percent of LDL lowering does.
- Operational readiness. U.S. site activation, pharmacy processes for one-time infusion, and clarity on who orders, administers, and follows these patients.
The bottom line
Prevention works when it lasts. In 2025, one-shot PCSK9 base editing took its first real steps in people and showed the kind of LDL reductions that matter. Regulatory momentum and a marquee acquisition suggest the sector is ready to test this at scale. The next six to twelve months will decide whether this becomes a durable, safe, and practical option that compresses lifetime risk for millions of people who want to stay out of the catheterization lab. If the data keep tracking, longevity’s first preventive gene therapy may arrive not with a silver-bullet cure, but with a simple idea made real: change the starting conditions early, and the future bends with you.