Beta-Cell Comeback: Vertex’s 2025 Pivot Speeds Remission
In June 2025, Vertex’s stem cell islet therapy zimislecel posted Phase 1/2 results with A1c under 7 percent and insulin independence for most at one year, pivoting the field from devices toward immunosuppression-first strategies.
The week diabetes care changed course
Every field has a moment when the signal rises above the noise. For type 1 diabetes, June 2025 delivered that moment. Vertex presented Phase 1/2 results for its stem cell derived islet therapy zimislecel, formerly VX‑880, at the American Diabetes Association meeting, paired with a same day New England Journal of Medicine publication. The headline was simple and startling: in the full dose cohort with at least one year of follow up, all patients hit guideline targets for glucose control and most were off insulin. The program’s center of gravity shifted overnight from devices that try to wall off cells from the immune system to a more classical approach that uses immunosuppressive drugs to protect transplanted cells while they take root. Vertex’s own portfolio tells the story. Its encapsulated product VX‑264 underperformed. Zimislecel surged to the front and is now steering toward regulatory filings in 2026.
If you followed the last decade of insulin pumps, continuous glucose monitors, and algorithmic dosing, this feels like a new chapter. The tools that manage glucose are now sharing the stage with a therapy that restores the tissue that makes insulin in the first place.
Key data at one year. Among the first 12 participants to receive a full dose of zimislecel and reach one year of follow up, every person achieved a hemoglobin A1c under 7 percent and more than 70 percent time in range, with 10 out of 12 off insulin entirely. Severe hypoglycemia did not recur after day 90. These numbers explain why attention snapped to zimislecel and why this article calls 2025 a watershed. See Vertex’s summary and trial design in the company’s update: Vertex presents zimislecel ADA results.
What the new data really say
Clinical trials report averages and endpoints. Patients live with days. The zimislecel dataset answers both. The early protocol used a single infusion of fully differentiated islet cells derived from stem cells. By month 12, endogenous insulin secretion was detectable and responsive to meals, hemoglobin A1c was in guideline range, and exogenous insulin had been reduced dramatically or eliminated in most participants. The primary endpoint for this portion of the study focused on removing severe hypoglycemia while normalizing hemoglobin A1c. It was met.
There is a second layer that matters for clinicians. The effect was not a brittle burst that faded. Zimislecel engrafted. C‑peptide, a marker of the body’s own insulin production, persisted. The New England Journal of Medicine paper provides granular lab values and mixed meal tests that make this feel less like hype and more like hematology grade cell therapy. See the details in the NEJM zimislecel Phase 1/2 paper.
Two caveats for scale and scope:
- This early population had severe hypoglycemic events and compromised awareness, the group with the highest risk and the most to gain.
- One year is not a lifetime. We will need three, five, and ten year follow up to understand durability and safety.
Why an immunosuppression first path is winning now
If the immune system is a neighborhood watch, transplanted cells are visitors who look like strangers. There are three ways to keep that visit peaceful.
-
You can ask the neighbors to relax a little. That is pharmacologic immunosuppression. It is familiar from solid organ transplantation. Regimens typically combine a calcineurin inhibitor with an antiproliferative agent and a steroid sparing strategy. These drugs have known dosing, monitoring, and risks. They are scalable today.
-
You can try to disguise the visitors. That is immune cloak biology. Gene edited cells can turn down the markers that T cells and natural killer cells look for, or display “do not eat me” signals like CD47. This idea is compelling, but you must prove that edited cells still function as islets for years without creating unwanted immune blind spots.
-
You can put the visitors behind a fence. That is the device route. Encapsulation aims to block immune cells while allowing oxygen, nutrients, and insulin to pass. It is elegant on paper and hard in the body, where even the most inert materials can trigger a fibrotic reaction that chokes diffusion.
In 2025, option one won. It won because it reliably delivered engraftment, regulated glucose responses, and insulin independence in a meaningful share of participants. Vertex’s own attempt at option three, VX‑264, showed acceptable safety but insufficient efficacy, which likely reflects diffusion and foreign body hurdles that have been hard to defeat across the field. Option two is maturing in labs and early programs, but it is not yet a clinic scale answer. For broader immunology context, see how cellular immune tuning is progressing in engineered Tregs and immune rejuvenation.
From headline remission to lived remission
For people with type 1 diabetes, remission is not a slogan. It is a daily change. The zimislecel results outline what that could look like in practice.
- Day to day variability shrinks. Continuous glucose traces flatten toward the target band. That means fewer alarms, fewer night checks, fewer calculations while commuting or caring for children.
- The most feared risk recedes. Severe hypoglycemia dropped to zero after day 90 in the reporting period. That changes how families plan travel, sports, and work.
- Devices become optional, not mandatory. Pumps and sensors remain valuable for safety and feedback. They may shift from life support to performance tools.
Timelines matter. In the trial, meaningful insulin reduction often emerged in the first months, with insulin independence in many by one year. For patients weighing this therapy, a realistic path looks like this: evaluation and listing for the trial or for future commercial access; a single day for the infusion; close monitoring for three months while immunosuppression is tuned; a steady climb in meal time C‑peptide and shrinking bolus doses; the possibility of putting away insulin entirely by month 12, with the understanding that partial support could return if graft function wanes.
Risks that are real and how to manage them
Immunosuppressive drugs invite infections, can raise skin cancer risk over time, and in some regimens stress the kidneys. In early zimislecel experience, the safety profile looked consistent with what transplant physicians expect. That does not make the risks trivial. It does make them legible. There are playbooks for vaccination, prophylaxis, dermatology checks, and renal monitoring. There are steroid sparing strategies and dose adjustments guided by trough levels and side effect screens. The calculus is individualized. For a person who has survived repeated severe hypoglycemia and who cannot sense oncoming lows, the trade can be worth it. For a person with excellent control and no severe events, the bar is higher.
The cost question and who gets it first
No one can quote a final price before regulators act and payers negotiate. The drivers are not mysterious, though.
- The cell therapy itself must be manufactured at scale, quality tested, cryopreserved, and shipped. Batch yields and release criteria are the key throughput and cost levers.
- The procedure is a catheter based infusion with perioperative monitoring. Hospitals will charge facility and professional fees similar to complex interventional procedures.
- The ongoing cost is the immunosuppressive regimen and the lab surveillance that goes with it.
At launch, access is likely to mirror the trial population. Expect initial indications that prioritize those with impaired hypoglycemia awareness and recurrent severe events despite best available technology. Payers will ask for documented history and a specialist’s attestation. Centers that already manage islet and solid organ transplantation are positioned to deliver the therapy first. Over time, if durability remains strong and safety remains predictable, indications can broaden.
For patients and families planning next steps, the most practical action is to assemble documentation now. Download continuous glucose monitor reports that show time in range and hypoglycemia frequency. Ask your endocrinologist to summarize severe events and automated insulin delivery settings. If you have chronic complications, confirm the status of kidney function, retinal exams, and neuropathy screens. This creates a package that accelerates evaluation once programs open.
The device route is not dead, but it must evolve
VX‑264’s underperformance matters, yet it does not close the book on devices. It clarifies the engineering targets.
- Oxygen is the choke point. Islet cells are metabolically hungry. Encapsulation must deliver reliable oxygenation in the first hours after implantation, not just diffusion of glucose and insulin days later. Designs that incorporate oxygen reservoirs or microvascular ingrowth without immune cell ingress are under study.
- The foreign body response is the spoiler. Materials that reduce fibrosis in animals often disappoint in humans. The bar is not low. Even a thin fibrotic layer can throttle diffusion.
- The surgical footprint must be simple. If implantation requires large incisions or difficult retrieval, adoption stalls. Flat pouches that slide into a well vascularized plane are more likely to scale than bulky cages.
Companies pursuing this path are experimenting with hydrogels, ultrathin membranes, and vascularizing scaffolds. The most credible next step is a hybrid, where modest immunomodulation is paired with a device that reduces, rather than absolutely blocks, immune contact. That could lower drug exposure while keeping oxygen and nutrient supply healthy. For a related surgical paradigm shift, see the xenotransplant pivot in 2025.
Immune cloak biology is the long game
If devices are fences and drugs are polite requests, immune cloak is a passport. Gene editing can delete the genes that present antigen to T cells, like beta‑2 microglobulin for class I and CIITA for class II, and add signals that ask innate cells to stand down, like CD47. The challenge is tuning this invisibility so that cells are tolerated without inviting infections or malignant transformation. Edited cells must still sense glucose, release insulin with meal time kinetics, and survive for years.
Why keep investing here if immunosuppression works today? Because a cloak that lets cells live drug free would decouple the therapy from infection risk and drug interactions, lower lifetime costs, and widen eligibility to children and to adults who have contraindications to immunosuppression. Progress in programmable cell states in humans, including epigenome editing enters humans, will inform islet programs. The likeliest near term win is a partial cloak that reduces the intensity of the drug regimen rather than eliminating it on day one.
What this means for everyday practice in 2026 and beyond
If Vertex files in 2026 and regulators agree that benefit outweighs risk for a high risk subset, diabetes clinics will need new pathways.
- Referral networks. Endocrinology practices should prearrange referral relationships with transplant capable centers, define workup checklists, and set expectations about immunosuppression education.
- Shared monitoring. Continuous glucose data will remain central, but immunosuppression requires lab surveillance. Clinics will need protocols for tacrolimus or analogous drug levels, renal function, and infection prophylaxis.
- Education for patients and families. The meaning of remission will change. People who have relied on pumps and automated dosing will need new skills for recognizing signs of infection and for medication adherence.
Importantly, automated insulin delivery does not go away. It becomes the safety net and backup plan. People who choose to discontinue immunosuppression or who experience graft decline will still have excellent options.
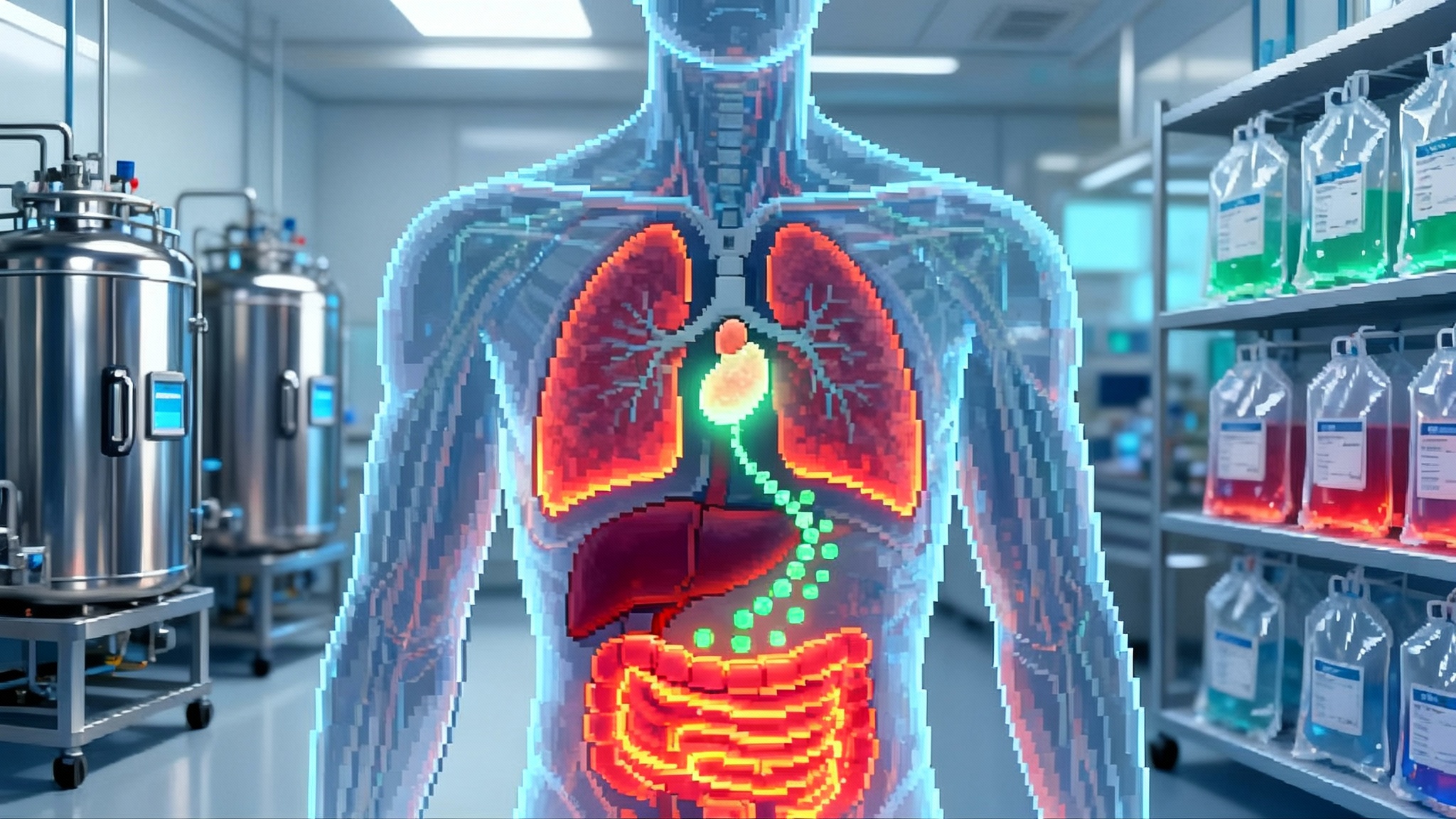
A watershed for longevity medicine
Longevity medicine is sometimes caricatured as supplements and biomarkers. The zimislecel story is the opposite. It is the restoration of a lost organ function with the goal of extending healthy metabolic span. Decades of data link sustained near normal glucose control to fewer microvascular complications of the eyes, kidneys, and nerves, and to less cardiovascular risk. If a single infusion can deliver stable C‑peptide and time in range over years, then the payoff is not only freedom from injections. It is fewer dialysis starts, fewer proliferative retinopathy procedures, fewer amputations, and fewer hospitalizations for hypoglycemia.
That is what makes 2025 feel like a hinge year. The field is moving from managing numbers to replacing tissue. The first wave will ride on familiar transplant medicine. The next waves will test edited cells and smarter devices. Each wave widens the circle of who can benefit.
What to watch next
- Durability beyond year one. The most conservative scenario is partial attrition of beta‑cell mass over time. A win would be flat C‑peptide curves out to year three and beyond.
- Immunosuppression light. Trials that step down drug intensity in stable recipients without loss of control will be a bellwether for wider adoption.
- Manufacturing scale and release criteria. Lot to lot consistency in potency and purity will determine how fast centers can treat patients once commercial supply opens.
- Pediatric pathways. Children live the longest with benefits and risks. Expect careful, staged evaluations after initial adult approvals.
The bottom line
A year ago, the smart bet in type 1 diabetes was better algorithms, better sensors, better pumps. Those will keep improving. The 2025 data say something bigger is now on the table. An off the shelf, stem cell derived islet therapy delivered as a single infusion can put a majority of high risk adults into insulin free remission by one year, with normalized hemoglobin A1c and no severe hypoglycemia. Vertex’s pivot from an encapsulated device to an immunosuppression first product is a hard earned result of biology and engineering reality. It is also a path that clinics know how to run today.
The race is not over. The next finish line is an immune cloak or a device good enough to retire chronic immunosuppression. When that arrives, the circle widens again. For now, the story is already big. We are watching a move from glucose management to durable tissue replacement. In longevity terms, that is the difference between coping with decline and restoring capacity. It is why this moment matters.