Plasma exchange hits geroscience as 2025 trials advance
A randomized Aging Cell readout showing 1 to 3 year shifts in biological age has pushed therapeutic plasma exchange from fringe idea to testable program. Here is what the data show, what they do not, and a blueprint to move fast without overselling.
The week blood factors got real
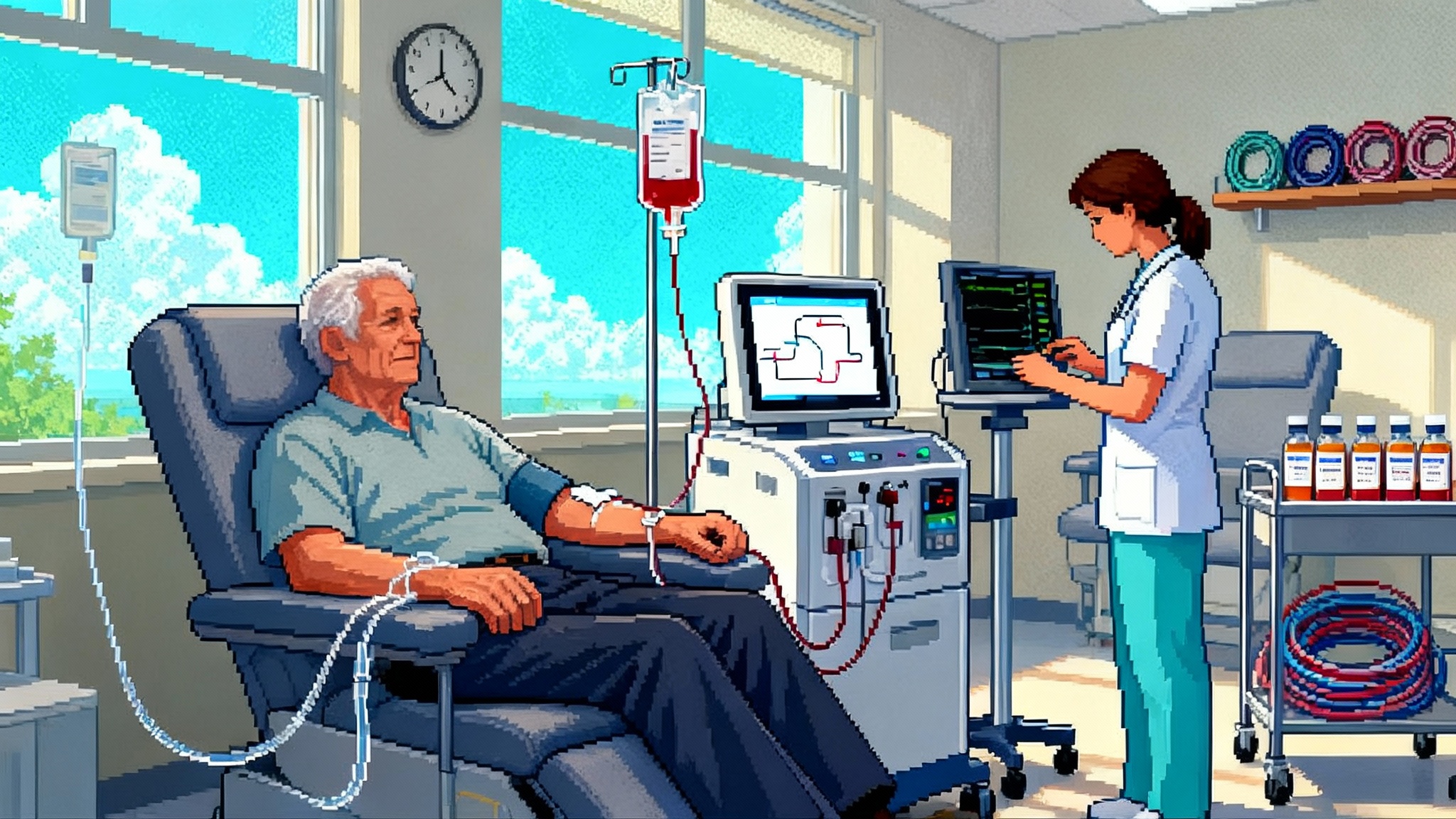
In late May 2025, a single-blind randomized trial in Aging Cell reported that therapeutic plasma exchange, with or without intravenous immunoglobulin, shifted multi-omics measures of biological age in adults over 50 by about 1 to 3 years on average. The effect was strongest when plasma exchange was paired with intravenous immunoglobulin, and the signal appeared after a handful of sessions rather than dozens. You can read the study summary and abstract on PubMed for the primary details, including the arms, adverse events, and the size of the shift across epigenetic clocks and other assays: multi-omics randomized TPE study.
The result did not prove that people lived longer or avoided disease. It did something more important for the field right now. It turned the vague idea of blood factors into a testable clinical program with a protocol, a safety readout, and a measurable biological effect that can be chased into outcomes. For context on how clocks behave in humans, see the semaglutide clock signal debate.
What plasma exchange actually does in the body
Therapeutic plasma exchange is a hospital-grade procedure that removes a person’s plasma and returns their blood cells suspended in replacement fluid, usually albumin solution. Think of it as changing the water in an aquarium while keeping the fish. The removal and replacement dilute or eliminate circulating proteins and particles that the body has been swimming in for decades. That includes inflammatory cytokines, autoantibodies, complement proteins, clotting factors, oxidized lipoproteins, microvesicles, and molecules tied to advanced glycation. Albumin replacement brings in a clean carrier protein that binds many toxins and metabolites, which can change how these molecules move in and out of tissues.
The idea that blood composition is causal for aging biology is not new. Animal experiments using heterochronic parabiosis suggested that old blood contains pro-aging signals and young blood contains supportive ones. Human translation stalled because transfusing young plasma at scale is not practical and carries ethical and regulatory problems. Plasma exchange is a cleaner engineering solution. Instead of adding young plasma, it removes the old plasma environment and replaces it with a standardized, regulated fluid.
Biomarker wins are not endpoints
The 2025 trial readout is a biomarker success, not a clinical victory. Epigenetic clocks, proteomic scores, immune composites, and other multi-omics measures are useful because they compress sprawling biology into trackable numbers. They correlate with risk. They are not the thing a patient or payer ultimately cares about. For a broader view of biomarker architecture, see how SenNet atlas maps biomarkers.
Why that distinction matters now:
- Surrogates can change quickly. Outcomes change slowly. A 2.6-year shift in a composite biological age metric over a few months is a striking laboratory result, but it is not a guarantee of fewer infections this winter or fewer heart attacks in five years.
- Clocks disagree. Different epigenetic clocks and proteomic scores can move in different directions based on the tissues sampled and the features they weigh. A composite win across multiple clocks is more convincing than a win on one, yet still a surrogate.
- Regression to the mean is a real confounder. People who volunteer for a longevity trial often arrive with worrying labs that improve with attention, repeat testing, and behavior change. Randomization and a sham arm help, but short trials are always at risk of over-reading noise.
If geroscience is to graduate from intriguing to inevitable, the next study has to bridge biomarkers to outcomes.
A blueprint for the first outcomes-grade trial
Designing the right randomized controlled trial does not need to be mysterious. Build it like a cardiovascular outcomes trial, with endpoints patients feel and payers reimburse. Here is a pragmatic plan that sponsors and investigators could run now. For how other aging programs have crossed from mechanism to clinic, see our thymus reboot translation playbook.
- Population: Adults 60 to 80 in the community with at least two risk features at baseline, such as high-sensitivity C-reactive protein above 2 mg/L, prior hospitalization for infection, or an elevated biological age metric relative to chronological age. Exclude people with immunoglobulin A deficiency or a history of thrombosis without appropriate prophylaxis.
- Arms: Three arms with 1:1:1 randomization. Arm A: plasma exchange with albumin only. Arm B: plasma exchange with albumin plus intravenous immunoglobulin at 0.5 g/kg after each exchange. Arm C: sham apheresis with identical chair time and fluid volume adjustments to keep blinding credible.
- Dosing cadence: Induction of three exchanges in the first six weeks, then maintenance every 12 weeks for two years. The 2025 trial hinted at diminishing returns after the first three sessions, which argues for spacing rather than weekly forever.
- Co-interventions: Standard preventive care and vaccinations. Capture and adjust for statin, antihypertensive, and glucose-lowering medications.
- Primary endpoint: Composite of first serious infection requiring antibiotics or hospitalization, incident major adverse cardiovascular event, or meaningful decline in physical function over 24 months. Define function a priori as a 1-point drop in the Short Physical Performance Battery or a 0.1 m/s drop in gait speed sustained at two visits.
- Key secondary endpoints: Change in frailty phenotype score, days alive out of hospital, total infection count, and a prespecified panel of biological surrogates including epigenetic and proteomic age, immune cell composition, and inflammatory proteome.
- Safety endpoints: Infusion reactions, symptomatic hypotension, hypocalcemia, catheter complications, thromboembolic events, and renal adverse events. Monitor total immunoglobulin levels to avoid persistent hypogammaglobulinemia.
- Power and size: Event-driven design targeting 80 percent power to detect a 20 percent relative risk reduction in the primary composite at alpha 0.05. In a moderate-risk cohort, that likely means 1,200 to 1,800 participants across 20 to 30 sites with two years of follow-up.
- Substudies: Pre-specified mechanistic cohorts for deep immunophenotyping and metabolomics, plus a home-based digital function substudy to detect changes in mobility and sleep that clinical visits miss.
This design is straightforward, clinical, and audit-proof. If plasma exchange truly changes the risk landscape, it should show up in fewer infections, steadier walking, and fewer cardiometabolic events.
Dosing cadence and diminishing returns
The biomarker trial suggests a pattern that is familiar from many clearing therapies. Early sessions do most of the work. Later sessions maintain the change. That makes sense if you think of plasma exchange as draining a bathtub that is constantly refilling. The first turns of the drain lower the water line dramatically. Once the tub is near your target, you only have to crack the drain to keep it there.
Operationally, an induction of three exchanges in six weeks followed by quarterly maintenance balances signal with burden. Biological monitoring can personalize the cadence. If immunoglobulin levels fall too low or the inflammatory proteome remains quiet, skip a maintenance cycle. If the proteomic risk fingerprint creeps back, move a maintenance cycle forward.
The IVIG variable: cost, safety, and supply
Intravenous immunoglobulin is both attractive and problematic. It likely cushions the transient drop in antibodies that follows plasma exchange, and the 2025 trial saw the largest biomarker shift when it was included. It is also expensive and constrained by supply.
An easy way to get your arms around the cost is to do the dose math. A common replacement dose after exchange is 0.5 grams per kilogram. For an 80 kilogram person, that is 40 grams. Medicare’s published average sales prices for common immunoglobulin products work out to roughly one hundred dollars per gram on the drug component alone, so the product acquisition cost for that person is on the order of four thousand dollars before any pharmacy handling, site fees, or margin. Real-world prices to patients can be far higher depending on setting and insurance.
Safety deserves equal attention. Immunoglobulin products carry boxed warnings for thrombosis and renal dysfunction, especially in older adults or those with vascular risk, and they can trigger hypersensitivity reactions. Good programs will hydrate patients, screen for risk, use the minimum effective dose and infusion rate, and monitor renal function and blood viscosity when indicated.
Supply constraints are real. Immunoglobulin comes from pooled human plasma collected over many months. That means longevity clinics cannot will new supply into existence. Any outcomes-grade program that routinely uses immunoglobulin needs procurement plans that do not cannibalize essential indications like primary immunodeficiency or chronic inflammatory demyelinating polyneuropathy.
The economics: eight to ten thousand dollars a session
Plasma exchange offered as a self-pay longevity service currently runs about eight to ten thousand dollars per session in the United States. That number reflects an intensive care capability delivered in an outpatient setting: trained nursing, apheresis capital equipment, sterile disposables, albumin replacement, chair time, and overhead. Adding immunoglobulin after exchange increases the cost materially. The business thesis for new entrants has been that people will pay, that centers can learn on real-world data while randomized trials mature, and that the path to insurance coverage runs through outcomes.
Investors have noticed. In July 2025, Circulate Health announced a twelve million dollar seed round led by Khosla Ventures to expand clinic partnerships and run additional studies. That funding arrives on the heels of the Aging Cell study and a growing waiting list at high-end clinics, but investors emphasized that proof of endpoints will take years. Read the funding announcement for the strategy and rollout details: Circulate raises 12 million seed.
Why we should be enthusiastic and cautious at once
If you only looked at the 2025 biomarker readout, you might think plasma exchange just became the first testable longevity therapy with human data. If you look sideways, the picture gets more complicated.
- In Alzheimer’s disease, the AMBAR program from Grifols used plasma exchange with albumin replacement and reported hints of slowed decline in moderate disease but not clear wins in mild disease. It showed feasibility and signals, not an approved therapy.
- Plasma-derived fraction approaches, such as Alkahest’s GRF6019, were safe but did not deliver consistent benefits on cognitive and functional endpoints in small randomized studies.
Those adjacent experiences do not knock plasma exchange out of contention. They remind us that biology is messy and that positive signals tend to attenuate as you move from lab surrogates to lived outcomes. They also underline a practical truth. If plasma exchange is going to be a real longevity therapy, the field has to prove reductions in infections, falls, hospital days, or cardiometabolic events in older adults who do not have a specific autoimmune diagnosis.
A practical acceleration plan
Here is how the field can move fast without overselling, starting today:
- Build a multi-site registry with a common data model. Every paying patient gets the same baseline panels, the same adverse event capture, and the same six and twelve month function testing. Use cloud-based randomization to stagger induction and maintenance timing across centers so that even real-world programs yield quasi-experimental leverage.
- Pre-specify what good looks like. For biomarker responders, define a minimal important difference on composite biological age that justifies a maintenance session and one that does not. Avoid open-ended induction that burns resources with little added gain.
- Use a sham where possible. The Aging Cell protocol showed that a sham is doable and acceptable to participants. Blinding matters in procedures with strong expectancy effects.
- Tie pricing to evidence. Clinics can offer a lower price for patients who agree to randomization and full follow-up. Investors can tie milestone financing to the completion of outcomes cohorts, not marketing metrics.
- Publish adverse events quickly. Make it easy for outside clinicians to see rates of hypotension, bleeding, catheter issues, and thromboembolic events, along with how often immunoglobulin is used and at what dose.
- Plan for payer conversations early. The first serious infection endpoint, the days-alive-out-of-hospital metric, and gait speed are legible to insurers. Bring them into the protocol design now so that a positive result has a chance at coverage later.
What to watch in the next 12 to 24 months
- The first large, outcomes-oriented randomized controlled trial launch in the United States with a sham arm and maintenance dosing every quarter.
- Real-world safety signals as expansion proceeds. Immunoglobulin supply alerts, lot withdrawals, or thrombosis clusters will stress test protocols and may force dose adjustments.
- Biomarker-to-outcome mapping. If specific proteomic or epigenetic shifts reliably forecast infection risk or functional decline, they can guide timing and identify responders.
- Payer pilots. Regional insurers might test coverage for high-risk older adults with recurrent infections, especially if bundled with a disease management program.
The bottom line
Plasma exchange has crossed an important line. It is no longer only a provocative animal story or a boutique procedure for autoimmune disease. In 2025, it became a clinical program with randomized human biomarker data, a safety profile in healthy older adults, and a plausible path to outcomes. The price tag is high, the logistics are nontrivial, and immunoglobulin complicates both safety and supply. Yet there is a straight road from here to proof. It runs through a well-powered trial with hard endpoints, sensible dosing, honest reporting, and a business model tied to evidence.
If the next studies show fewer infections, steadier steps, and fewer cardiometabolic events, plasma exchange will not just make people look younger on a lab report. It will make them feel and live younger in ways that count. That is when the field will have earned the right to call this a longevity therapy in the plain sense of the word.