Senolytics Get Real: 2025 Eye Trial Puts Them on the Map
Unity Biotechnology’s senolytic UBX1325 kept pace with aflibercept over 36 weeks in diabetic macular edema, with clean ocular safety and a clear responder subgroup. Here is why the eye was the right proving ground and what this means for the next wave of aging drugs.
The moment senolytics moved from idea to clinic
For a decade, the pitch behind senolytics has been straightforward: clear out damaged, retirement‑age cells that refuse to die, and tissues should work better. The concept has been tested in mice, debated at conferences, and pursued by dozens of startups. In 2025 it finally met a demanding human benchmark.
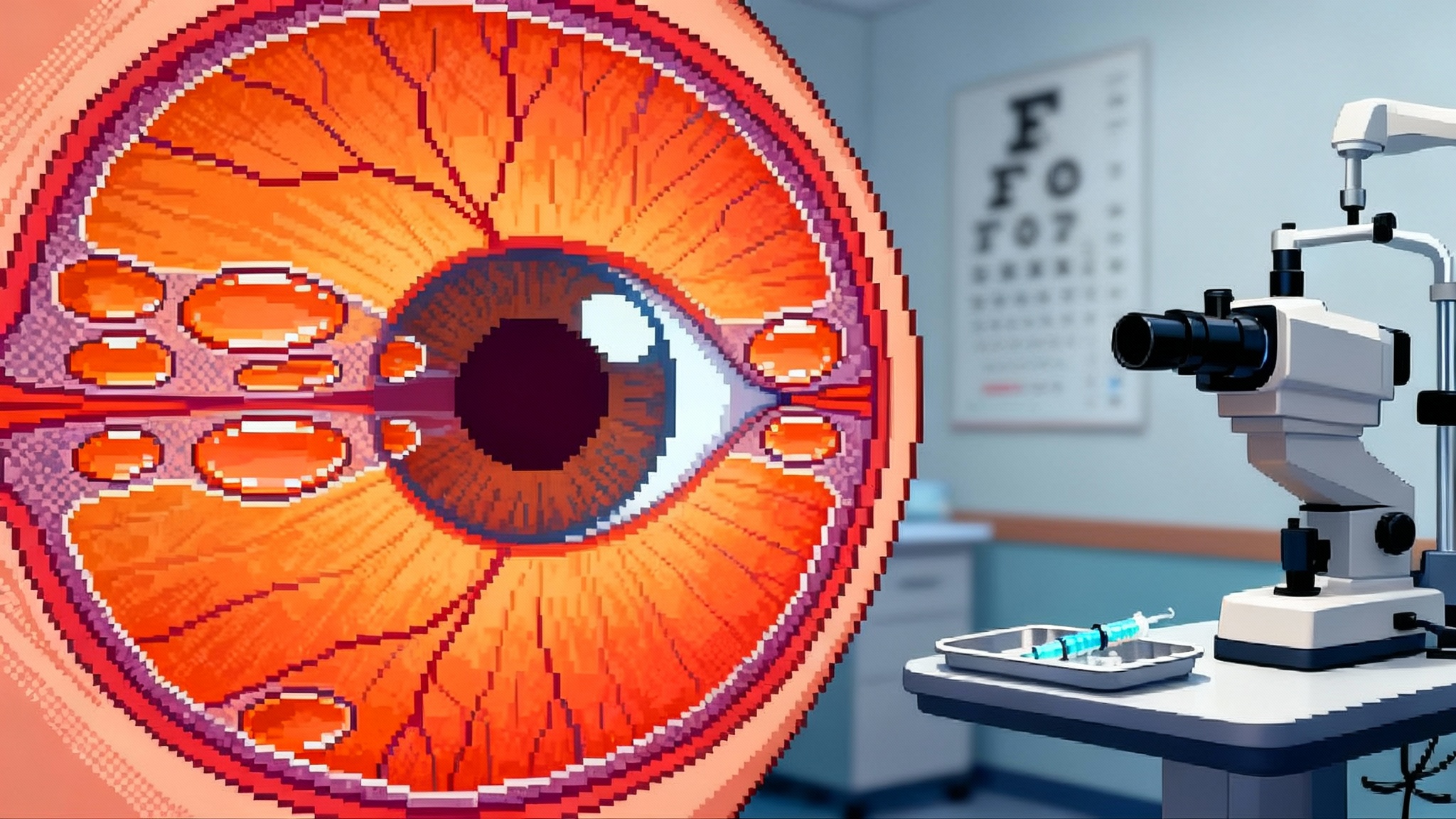
In May, Unity Biotechnology reported complete 36‑week results from its Phase 2b ASPIRE trial in diabetic macular edema (DME). Patients received either UBX1325, a small molecule that pushes senescent cells over the edge by targeting BCL‑xL, or aflibercept, the standard anti‑VEGF injection used across retina clinics. UBX1325 delivered vision gains that were statistically non‑inferior to aflibercept at week 36, with a generally clean safety profile and no inflammatory complications. The full readout is here: Unity’s 36‑week ASPIRE results.
The numbers behind the headline build confidence. Unity highlighted best corrected visual acuity gains of roughly five letters from baseline, comparable to aflibercept, and superiority signals in a pre‑specified subgroup that made up about sixty percent of the trial. The primary analysis, a pre‑specified average of weeks 20 and 24, fell just short of a stringent non‑inferiority threshold, but by week 36 UBX1325 was clearly in the same performance lane as the incumbent. For a first‑in‑class senolytic in a head‑to‑head retinal trial, that is a milestone.
Why the eye went first
If senolytics aim to selectively remove problem cells, ophthalmology is the ideal test bed. Three practical reasons explain why:
- Direct delivery. Intravitreal injections put the drug exactly where disease is playing out. That means lower systemic exposure and the ability to modulate dose and schedule with precision. In senolytics, where the goal is to cull specific cells without collateral damage, local delivery is a decisive advantage.
- Sharp endpoints. Vision is quantifiable in letters gained. Retinal anatomy is mapped in microns by optical coherence tomography. Investigators can see fluid pockets dry up and measure central subfield thickness session by session. This level of resolution favors mechanisms that need proof of effect, not just plausible biology.
- Fast readouts. DME patients often respond within weeks, and durability is evident within months. A study can show whether a new mechanism stacks up against a standard injection schedule far faster than in systemic diseases where outcomes take years.
This pattern is why other frontier mechanisms have also launched in retina. For example, see why the eye often goes first.
What the ASPIRE data really says
The claim of non‑inferiority at week 36 is not a participation trophy. Aflibercept is the anchor therapy across DME and wet age‑related macular degeneration, and it has earned that position in numerous randomized studies. Matching it in visual outcomes while coming from a different mechanism suggests UBX1325 is doing something meaningfully therapeutic. The pre‑specified subgroup advantage in patients with moderately aggressive disease, defined by central subfield thickness under 400 microns, strengthens the case. That pattern hints that clearing a pool of senescent cells may help most when disease is active but not in a full‑blown flare.
Safety matters in the eye because inflammation or vascular events can damage vision quickly. Unity reported no intraocular inflammation, vasculitis, retinal artery occlusion, or endophthalmitis across its trials to date. For a drug that induces apoptosis in a targeted set of cells, clean ocular tolerability is a critical box to tick.
There is a sober footnote. Unity simultaneously announced it would explore strategic alternatives, a way of saying the company will likely seek a partner or buyer to finance Phase 3 and beyond. That reflects the capital intensity of late‑stage ophthalmology trials and the reality that large retinal franchises often live inside companies like Regeneron, Roche, and Novartis. The biology can be right while the balance sheet pushes a handoff.
How a senolytic works in the retina
UBX1325 targets BCL‑xL, a protein that many senescent cells depend on to avoid apoptosis. Think of BCL‑xL as a guardrail that keeps a damaged cell from tipping into programmed death. Blocking it removes the guardrail, and cells already primed by stress are the ones that fall. In theory this selectivity is what separates a senolytic from broadly cytotoxic agents. The eye’s immune‑privileged environment and small tissue volume increase the odds that you remove the intended targets and minimize bystander effects.
DME has a population that makes this particularly attractive. Many patients have responded to anti‑VEGF therapy but still carry residual edema or plateaued vision gains. If a senolytic can maintain visual acuity while reducing visits or improving anatomy in a subset that stalls on standard care, it can carve out a role either as switch therapy or in combination.
Why ophthalmology is the proving ground for aging drugs
Aging biology is full of hard questions: which cells are truly senescent, which are harmlessly paused, and which serve useful roles in wound healing. Systemic drugs that indiscriminately chase senescent markers risk off‑target effects. The eye avoids some of this complexity. Investigators can:
- Deliver locally and monitor a confined compartment.
- Use imaging as a functional biomarker of disease state in near real time.
- Run head‑to‑head trials with established dosing schedules.
It is no coincidence that other aging‑relevant programs also validate in compartments with precise endpoints. For a broader view of translational pacing, see how plasma exchange trials are advancing.
What this means for systemic aging diseases
The question every geroscience team is asking is whether a clean ophthalmology win can translate into systemic indications such as osteoarthritis, kidney disease, lung fibrosis, or vascular aging. The cautious answer is yes, but with specific conditions:
- You need the same level of selectivity. In the eye, a low dose in a sealed compartment can find stressed cells and spare healthy tissue. In systemic disease, you must deliver enough drug to the right tissues without knocking out helpful cell populations. That points toward targeted delivery systems, local injections into joints, or periodic pulsed dosing that allows recovery.
- You need practical, disease‑relevant endpoints. Senescent cell burden is not a clinical outcome. Pain and function scores in osteoarthritis, glomerular filtration rate in kidney disease, and forced vital capacity in lung fibrosis are what matter. A systemic senolytic must move those needles within a time frame that investors and regulators can accept.
- You need evidence that the mechanism matches the disease stage. The ASPIRE subgroup signal suggests disease context matters. In some tissues, senolytics may shine when disease is smoldering rather than roaring. That argues for stratified enrollment using imaging, fluid biomarkers, or genetic risk scores to find the state where clearance helps most.
Translation will not be linear, but the retina experience gives a template. Start where you can deliver locally and measure precisely, expand to well‑chosen compartments like the knee or the kidney, and only then push to systemic aging endpoints.
The regulatory accelerants for 2026 to 2027
Two developments could speed the path from promising mid‑stage data to approval decisions.
First, more refined endpoints in retina. Regulators have already accepted best corrected visual acuity as a primary outcome and have shown flexibility when drugs extend dosing intervals without compromising vision. For senolytics, sponsors can design Phase 3 studies that test non‑inferiority on vision while demonstrating clinically important advantages such as fewer injections, better anatomic dryness on optical coherence tomography, or reduced treatment burden for patients who previously needed frequent visits. Real‑world outcomes like injection‑free intervals and clinic visit reductions, collected prospectively, can add weight.
Second, better biomarkers and a clearer process for using them. The Food and Drug Administration’s program provides a formal pathway to validate biomarkers for a defined context of use. See the agency’s overview: FDA biomarker qualification program. For discovery and context, compare with SenNet’s 2025 atlas on biomarkers.
Here are three practical biomarker moves sponsors can make now:
- Build an ocular fluid panel of senescence‑associated secretory phenotype markers, such as interleukin 6 and matrix metalloproteinases, and validate how changes correlate with optical coherence tomography dryness and vision. Use those data to support a mechanistic secondary endpoint.
- Use widefield imaging to track microaneurysm turnover alongside optical coherence tomography measurements. If senolysis reduces the formation of new lesions while drying the retina, that supports disease modification rather than symptom control.
- Predefine a responder subgroup using central subfield thickness, prior anti‑VEGF response, and baseline inflammatory markers. If the same pattern of benefit repeats in Phase 3, it can justify label language for a population where senolytics are most effective.
These steps do not replace vision endpoints. They strengthen the narrative that a senolytic mechanism is acting on disease biology, which gives regulators more confidence and helps clinicians decide when to use the drug.
The competitive context and what to watch next
The ophthalmology landscape moves quickly. Regeneron and Bayer are extending aflibercept dosing with higher‑concentration formulations. Roche and Novartis are pursuing longer‑acting biologics and delivery systems. Against this backdrop, a first senolytic that matches vision outcomes and reduces visit burden in the right subgroup could earn a real clinical niche, especially for patients who stagnate on anti‑VEGF cycles.
Unity’s strategic review means the next move likely comes from a partner with a retina sales force and a manufacturing engine. Expect discussions to center on three items: the subgroup data, the clean safety profile, and a Phase 3 design that offers a clear use case such as switch therapy or combination with anti‑VEGF in patients with moderately aggressive disease.
Beyond retina, several teams are pushing senolytics toward joints, kidneys, fat, and the vasculature. The lesson from ASPIRE is to avoid one‑size‑fits‑all claims. Pick indications where delivery can be localized or where short pulses can reach the target tissue. Choose endpoints that move within a year. Predefine biomarker panels and stick to a context of use that is realistic. The fastest path to a systemic label is a string of wins in places where the biology and the clinic are aligned.
The takeaways for builders, clinicians, and investors
- For companies: design Phase 3 around non‑inferiority on vision, superiority on treatment burden or anatomy, and a predefined responder subgroup. Secure a manufacturing partner early, because ophthalmology programs live or die on supply chain reliability.
- For clinicians: identify patients who plateau on anti‑VEGF with residual fluid and moderate thickness. If Phase 3 confirms the subgroup effect, those are the candidates who may benefit from senolysis.
- For investors: value the mechanism, not just the p‑value. A drug that matches vision, trims injections, and targets a large real‑world problem can be commercially attractive even without statistical superiority on the primary endpoint.
- For researchers: push biomarker qualification with shared datasets. If a small set of ocular markers can be accepted as pharmacodynamic surrogates, it will shorten timelines for every program in the class.
The bottom line
Senolytics just cleared a bar that matters. In a rigorous, head‑to‑head retinal trial, a drug designed to remove harmful cells kept pace with the standard of care and showed advantages in a common subgroup. The eye, with its precision delivery and crisp endpoints, was the right place to prove it. If sponsors pair that playbook with smart biomarkers and pragmatic trial designs, the first approvals for a senolytic mechanism could sit on the calendar by 2027. The next chapter of aging therapeutics might start with better vision, and it will be written by teams that treat senescence as a target to measure, modulate, and, when it helps patients, remove.