Anti-CH Arrives: Slowing TET2 Clones to Extend Healthspan
Late-2025 data move clonal hematopoiesis from biomarker to modifiable risk. Here is how screening at 55 and up, near-term anti-inflammatory drugs, and future gene edits could reshape prevention of heart disease and cancer.

Breaking: a blood aging target becomes actionable
Clinicians have spent a decade watching clonal hematopoiesis creep into the charts of older adults as an ominous biomarker. This year the story changed. In August 2025, a subanalysis from a large cardiovascular trial reported that daily low-dose colchicine did more than cut events in chronic coronary disease. It also slowed the growth of high-risk TET2-mutated blood clones that define clonal hematopoiesis. That shift, from association to modification, moves clonal hematopoiesis from the margins of precision prevention to the middle of the stage. The implications reach from how we staff primary care to the economics of aging.
The new result is not a curiosity of lab metrics. TET2 clone size tracks with inflammation and cardiovascular risk. When a cheap, widely available anti-inflammatory blunts that growth signal, the field gets the first practical lever for age-related blood clones. The study’s authors observed attenuated expansion of TET2 clones over time in patients randomized to colchicine compared with placebo, consistent with the drug’s known effect on the interleukin 1 beta pathway. For prevention, that is a door opening, not an endpoint. It points directly to a future where we screen for clonal hematopoiesis after midlife and then treat it to reduce heart disease and possibly cancer risk. See the late-breaking summary from the American College of Cardiology: ACC summary on TET2 clones.
Clonal hematopoiesis, in plain language
Your blood system renews itself from a small pool of stem cells in the bone marrow. Over decades, these cells pick up DNA typos. Most of those mutations do not help a cell compete. A few do. If a mutation grants a small fitness advantage, that stem cell and its descendants take up a growing share of the blood factory. When the share gets big enough to detect on a sensitive blood DNA test, we call it clonal hematopoiesis. When there is no overt blood cancer, many clinicians still use the term CHIP. Think of it as gray hair for your bone marrow, except some strands push inflammation in the rest of the body.
Two genes dominate this landscape. DNMT3A and TET2 account for a large share of age-related blood clones, with JAK2 and ASXL1 less common but often more ominous. These genes shape how immune cells behave. TET2 loss pushes white blood cells toward a noisier inflammatory profile. DNMT3A loss often rides along with age but can be less inflammatory at a given clone size. The bigger the clone, the louder the signal. Bigger is measured as variant allele fraction, the percentage of sequencing reads carrying the mutation.
What matters clinically is not only leukemia risk, which remains low for most carriers, but a wider web of consequences. Studies over the last few years connected TET2 and other non-DNMT3A clones to higher risk of myocardial infarction, heart failure with preserved ejection fraction, atrial fibrillation, and inflammatory conditions such as pericarditis and myocarditis. Animal data mirror that signal and give it teeth by showing causality in inflammation circuits. The persistent theme is simple. Mutant blood can drive disease in organs that are otherwise structurally intact. For broader context on vascular aging, see our take on midlife arteries as a systems controller: arteries as aging’s command hub.
From biomarker to target: why the 2025 signal matters
A biomarker that moves is a target. Colchicine has already proven itself in two major cardiovascular outcome trials for event reduction. The 2025 clonal analysis adds a mechanistic layer that clinicians can act on today while the field builds the next tier of therapies. If tamping TET2-driven inflammation also slows the expansion of the clone itself, we are not only lowering the flame. We may be turning down the gas.
This is not the first hint that targeting interleukin 1 beta matters more in TET2 carriers. Exploratory analyses of earlier outcomes trials suggested that people with TET2 clonal hematopoiesis might get outsized cardiovascular benefit from interleukin 1 beta blockade. That pattern, combined with the colchicine clonal dynamics data, gives the field both a low-cost starting point and a rationale for precision anti-cytokine strategies.
What screening could look like at 55 and older
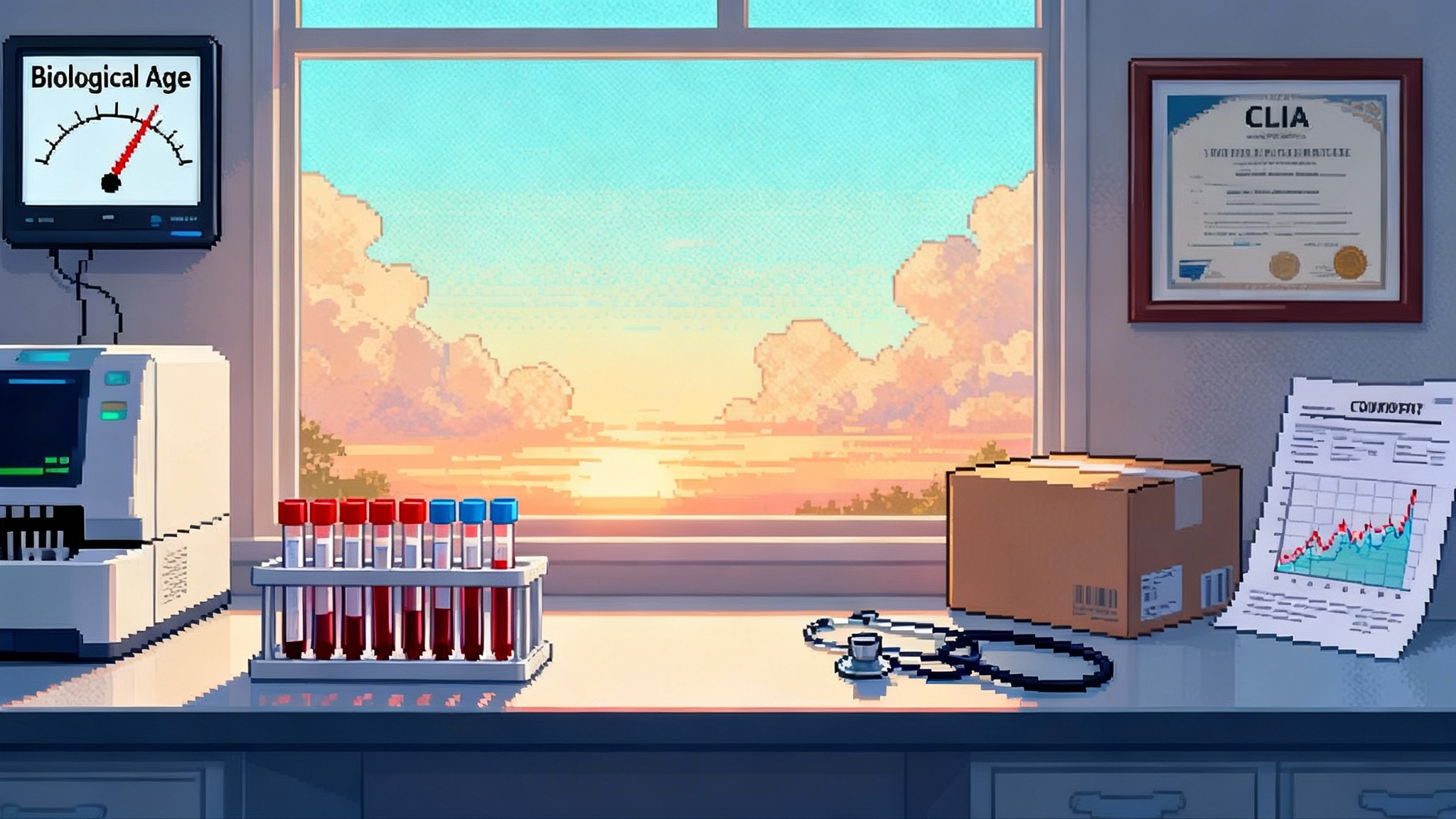
The barrier to screening is not technology. It is policy and workflow. Today, a targeted next generation sequencing panel on a single blood draw can detect the major clonal drivers at variant allele fractions as low as a few percent, and even lower with error-corrected methods. What primary care needs is a simple pathway that meshes with annual prevention visits.
Here is a pragmatic blueprint that clinics could adopt without creating a new specialty visit.
- Who to test first: Adults 55 and older with any of the following: established atherosclerotic cardiovascular disease, persistent high high-sensitivity C-reactive protein despite guideline therapy, family history of premature heart disease, prior cancer therapy that involved cytotoxic agents, or unexplained macrocytosis. Age alone qualifies at 65 and older.
- What to measure: A small blood DNA panel that includes DNMT3A, TET2, ASXL1, JAK2, and splicing-factor genes common in myeloid disease. Include variant allele fraction reporting and flag multiple mutations.
- How to risk-tier: Combine gene identity and clone size. TET2, ASXL1, and JAK2 at any material clone size move patients into higher cardiovascular surveillance. DNMT3A alone at low variant allele fraction may stay in watchful waiting unless there is rapid growth or multiple clones.
- What to repeat: Recheck the panel in 12 months for anyone with a detected clone. Earlier if symptoms or blood count changes appear.
- What to act on now: Use the result to sharpen cardiovascular prevention. This means closing gaps in statin therapy, blood pressure control, smoking cessation, and vaccine updates. For TET2 carriers in particular, discuss low-dose colchicine if there is a cardiovascular indication and no contraindication. The 2025 data suggest an added benefit on clonal dynamics while you are already treating vascular inflammation.
This design leaves room for shared decision making and protects against overdiagnosis. It also builds a data spine that health systems can mine for outcomes as payers decide what to reimburse.
The therapy ladder: from cheap pills to precise edits
Think of anti-CH therapy as a ladder that climbs from broad to precise.
- Near-term, low-cost anti-inflammatories
- Colchicine at 0.5 mg daily already reduces cardiovascular events in chronic coronary disease. The new clonal data strengthen its case in TET2 carriers by showing slower clone growth in addition to event reduction. Side effects are usually gastrointestinal. Watch for drug interactions with strong P-glycoprotein or cytochrome P450 3A4 inhibitors and avoid use in advanced renal or hepatic impairment. Cost is modest and access is simple.
- Statins remain foundational. They lower low-density lipoprotein and have anti-inflammatory effects. In practice, colchicine layers on top of statins rather than replacing them. Patients should still get to guideline low-density lipoprotein targets. For where LDL therapy is headed, see PCSK9 base editing leap.
- Targeted cytokine blockade
- Interleukin 1 beta inhibitors, such as canakinumab, reduced recurrent events in high-risk patients in prior trials. Exploratory genomics suggests TET2 carriers may benefit more than average. That is biologically plausible because TET2 loss shifts myeloid cells toward interleukin 1 beta signaling. New, small randomized studies are starting to test whether directly dampening interleukin 1 beta reduces vascular inflammation more in TET2-positive individuals than in others. If those trials hit vessel wall signals and safety endpoints, larger event-driven studies can follow.
- Interleukin 6 ligand blockade with ziltivekimab has shown dramatic reductions in inflammatory biomarkers and is in outcomes testing. If outcomes data confirm benefit, a subgroup analysis by clonal status will be important. The biology lines up, since TET2 and related clones drive an interleukin 1 to interleukin 6 axis. Cost, injection logistics, and infection risk will be the constraints that payers watch.
- Clone-specific small molecules
- Several biotech programs are moving upstream toward the clone itself. The principle is to selectively blunt the fitness advantage of mutant cells without suppressing the entire marrow. Strategies include nudging epigenetic balance to restore differentiation, inhibiting stress pathways that TET2 or DNMT3A clones rely on, and dialing down pattern-recognition signaling in myeloid cells. Early collaborations between small companies and academic labs are starting to test compounds against clonal hematopoiesis models and patient-derived cells. Expect first-in-human signals on clonal burden before hard outcomes. If a pill consistently shrinks TET2 variant allele fraction over a year without cytopenias, the case for combination with anti-inflammatory therapy becomes strong.
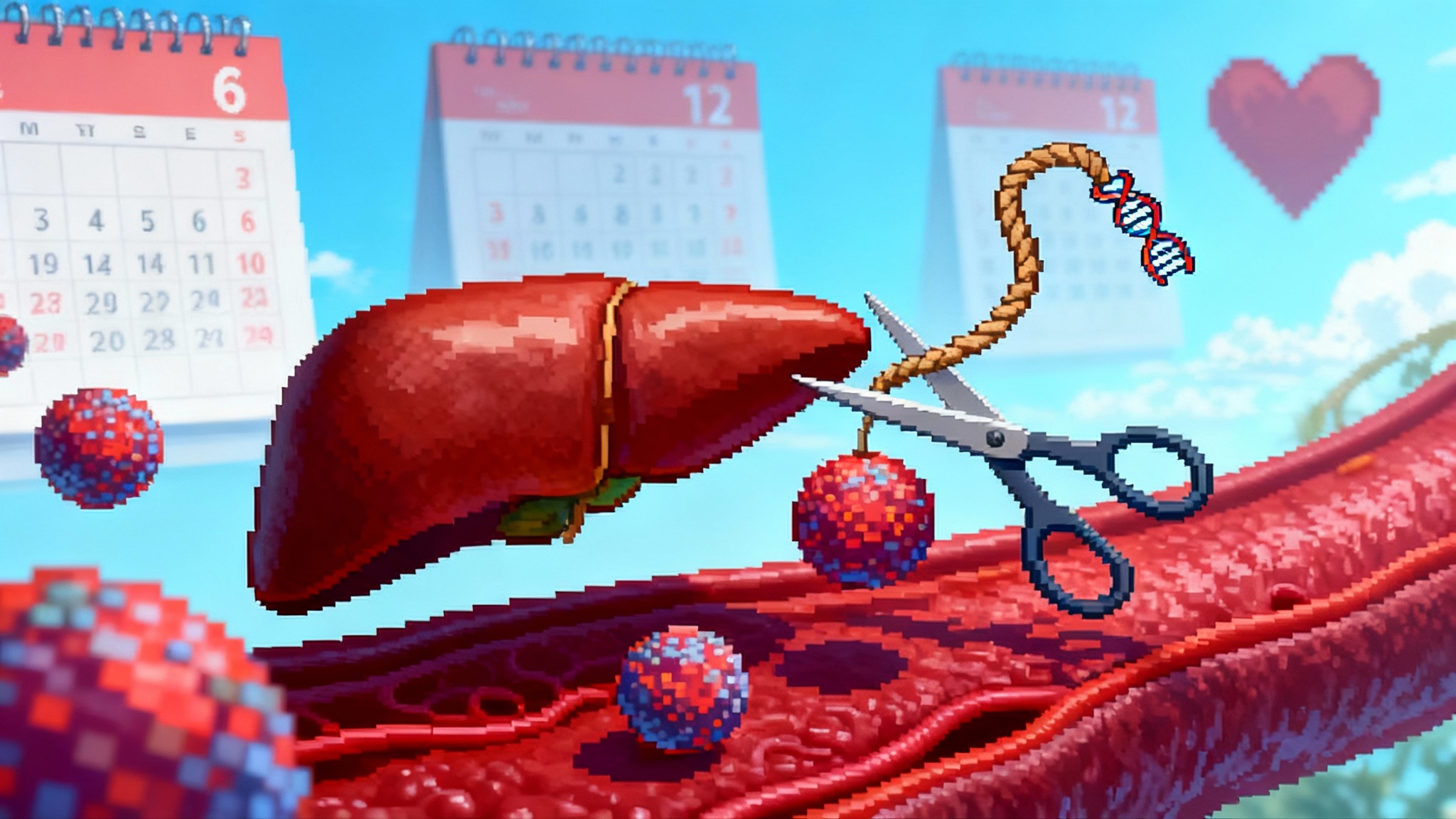
- In vivo edits to the stem cell compartment
- The endgame is precise editing. Delivery systems that target hematopoietic stem cells in vivo are maturing in other diseases. If they safely reach marrow stem cells, one could imagine a one-time treatment that clips the mutant edge off a clone or installs a safety circuit that makes mutant cells more sensitive to natural brakes. This will require exquisite specificity and careful modeling of what happens when you partially correct a mosaic marrow. Expect oncology-style monitoring for off-target edits and clonal selection. The first wave will likely be small trials in high-risk clones where the natural history is rapid and the benefit-risk balance is favorable.
Policy and payment: the 24 to 36 month window that matters
For screening to move from thought experiment to clinic default, two forces must align. Regulators must allow pragmatic tests to reach patients, and payers must be willing to reimburse when the clinical logic is clear.
The regulatory road actually got smoother this fall. In September 2025, the Food and Drug Administration rescinded its 2024 rule that would have tightly regulated laboratory developed tests as devices after a federal court vacated that rule. That return to enforcement discretion means Clinical Laboratory Improvement Amendments certified labs can continue to offer clonal hematopoiesis panels without device clearance, while still meeting quality standards. That lowers time to clinic for improved assays that measure small clones and track them over time. See this summary from the American Hospital Association: AHA update on LDT rule. For a related trend on diagnostics re-entering care pathways, read aging clocks return to clinic.
Payment will hinge on three near-term questions.
- What outcomes do payers accept for coverage of a screening panel in people without diagnosed cancer or blood disease? A reasonable bar is documented risk reclassification that changes management and lowers events when paired with anti-inflammatory therapy. Health systems can start by building registries that track clonal status, medications, and outcomes. If 55 and up screening paired with colchicine yields fewer hospitalizations for unstable angina or heart failure, that will move coverage decisions.
- Will payers cover cytokine blockers for TET2-positive prevention? Not without hard outcomes or a high-risk indication. Bridge studies that randomize TET2-positive patients with established coronary disease to interleukin 1 beta blockade versus placebo and read out vascular inflammation, clonal dynamics, safety, and a composite of admissions could set the stage. Manufacturers should plan outcomes-based contracts that link payment to reductions in emergency visits and admissions.
- Can we avoid false positives and overuse? Yes, with rules. Start with a focused gene list, require variant allele fraction thresholds for action, and repeat testing to confirm growth before escalating therapy. Laboratories should automatically annotate results with risk tiers and standard language for primary care.
What health systems and clinicians can do this year
- Build a simple 55 and up screening pathway. Add a clonal hematopoiesis panel to the annual prevention visit for patients who already meet cardiovascular risk thresholds. Start with TET2, DNMT3A, ASXL1, and JAK2. Ask your lab to report variant allele fraction and to flag multiple mutations.
- Update your cardiovascular order sets. Add a colchicine option for patients with chronic coronary disease and no contraindications, with counseling that benefits may include both fewer events and slowed TET2 clone growth.
- Stand up a registry. Capture clonal status, variant allele fraction, medications, cardiovascular events, blood counts, and infections. Share de-identified data within your system to support quality improvement and payer discussions.
- Assign ownership. In most systems, cardiology or preventive cardiology will co-own the pathway with hematology. Primary care should not be left alone to interpret rare JAK2 findings or unusual panels.
The ecosystem that is forming
Most large oncology testing companies already identify and subtract clonal hematopoiesis signals from liquid biopsy reports to avoid mistaking blood mutations for tumor mutations. That means the infrastructure for detecting clonal hematopoiesis in routine care is already in use, just aimed at a different question. On the therapeutics side, big companies are advancing cytokine blockers in broader cardiovascular populations while smaller biotechs pursue clone-specific approaches with academic partners. Health systems can use that tailwind to adopt screening and contribute real-world evidence.
Investors should watch for three milestones. First, replication of the colchicine clonal dynamics signal in an independent cohort. Second, randomized readouts that show greater vascular inflammation reduction in TET2-positive patients receiving interleukin 1 beta blockade. Third, early human data that a clone-specific small molecule safely reduces variant allele fraction over a year.
Bottom line
Clonal hematopoiesis has been a warning label. Late 2025 moved it toward a treatment target. A cheap anti-inflammatory slowed the growth of the riskier TET2 clones while treating cardiovascular risk. Regulators cleared the runway for labs to offer better tests. The next two to three years will decide whether payers embrace a simple 55 and up screen and treat pathway that trims hospitalizations for heart and inflammatory complications. If they do, anti-CH therapy will join statins and blood pressure control as a mainstream way to extend healthspan.
We have seen this movie before. Low-density lipoprotein was once a number in a lab report. It became a goal, then a target, then a toolkit. Clonal hematopoiesis is entering the same arc. For a preview of one-shot lipid lowering, see one-and-done LDL editing. The moment to design the clinic playbook is now.