The Muscle Turn: 2025’s Sarcopenia Race and the GLP-1 Gap
2025 turned muscle into medicine. As GLP-1 weight loss reshapes cardiometabolic care, lean mass is at risk. Here is how PGE2 repair, anti-inflammatory strategies, and growth-release agents could close the sarcopenia gap using endpoints that regulators trust.
The year muscle stepped into the spotlight
It finally happened. In 2025, muscle stopped being a side story to weight loss and longevity and became the main plot. Three events set the tone. In September 2025, Epirium Bio reported positive Phase 1 results for MF-300, a first-in-class 15-hydroxyprostaglandin dehydrogenase inhibitor designed to restore prostaglandin E2 and reactivate muscle repair. In February 2025, TNF Pharmaceuticals opened a Phase 2b study of an oral tumor necrosis factor alpha inhibitor for post-fracture frailty, a population that needs strength gains now rather than promise later. Then in September 2025, Eli Lilly halted a study that combined bimagrumab, an anti-activin receptor type II antibody that lifts the brakes on muscle growth, with tirzepatide, a modern weight loss drug. That stop underscored the problem every clinician sees in the clinic: powerful weight loss can carry meaningful lean mass loss unless you plan for muscle from day one.
Muscle is not just motion. It is a glucose sink, a reservoir for amino acids during illness, an endocrine organ that signals to bone, brain, and immune cells. Lose enough and the world narrows. Stairs become cliffs. Small infections become hospitalizations. Falls break people, not just bones. This is why muscle is the next mainstream gerotherapy. It addresses falls, frailty, and everyday resilience. In 2025 the science and the urgency finally met.
Why muscle preservation is the next mainstream gerotherapy
A good gerotherapy should do three things. First, reduce risk that accumulates with age. Second, work across multiple systems, because aging is multiplex. Third, fit into the care pathways people already use. Muscle checks all three boxes.
-
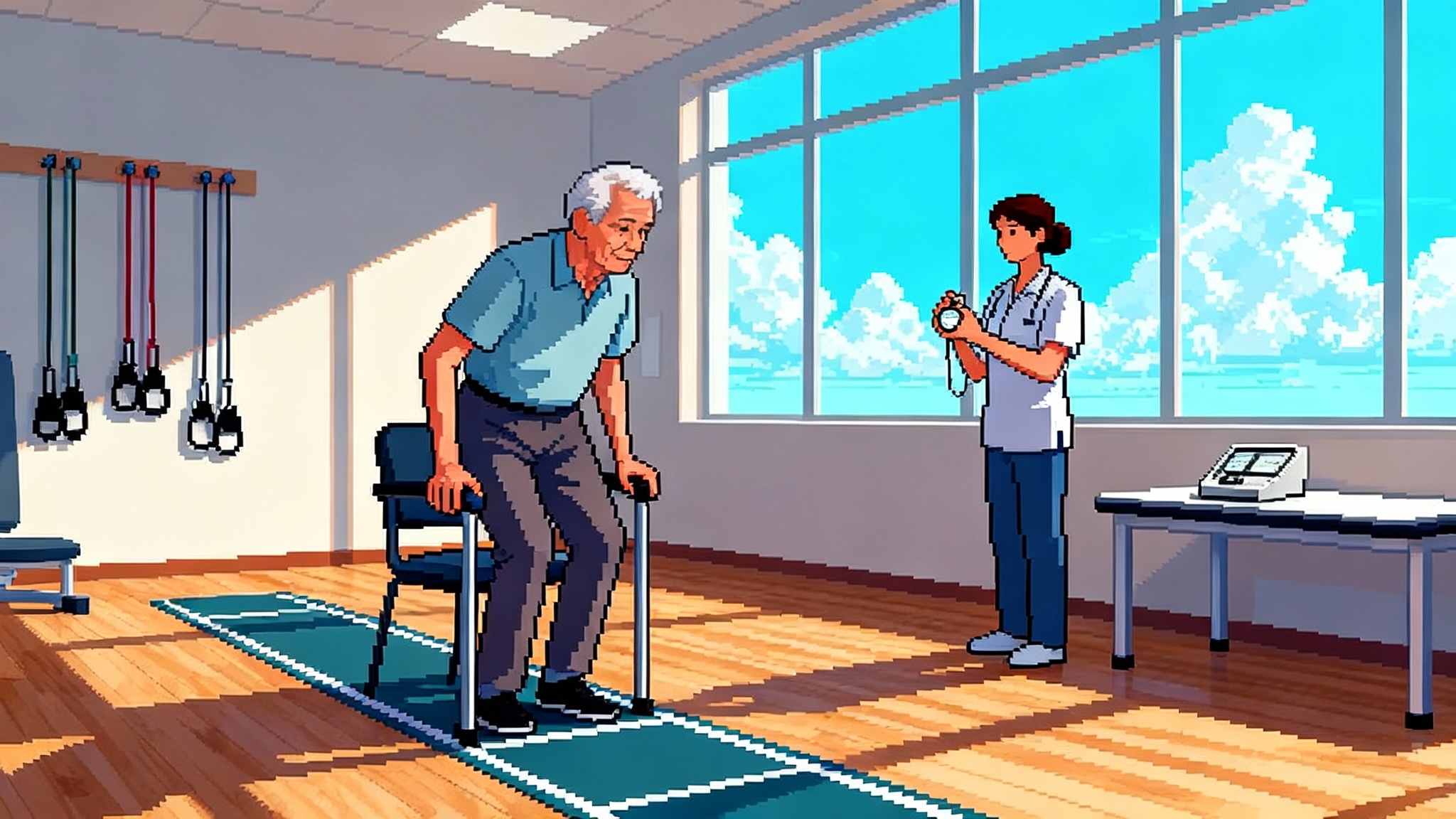
Risk reduction: Low muscle mass and impaired strength increase hospitalization risk, disability, and mortality. The differences are not cosmetic; they are measurable. Slower usual gait speed predicts future falls and loss of independence. The Short Physical Performance Battery, which combines balance, chair stands, and gait speed into a 0 to 12 score, has strong links to outcomes that matter, like institutionalization and mortality.
-
Multisystem benefits: Muscle stores glycogen, acts as a shock absorber for metabolic stress, and secretes myokines that talk to bone, liver, and immune cells. Stronger muscle often means steadier glucose, better recovery from infections and surgeries, and faster return to baseline after a setback.
-
Clinical fit: Muscle function shows up in the metrics clinicians already track. Grip strength can be measured in minutes. Gait speed can be captured in a corridor. These are not lab curiosities; they are clinic tools.
The current moment is defined by tension. Weight loss drugs help reduce cardiovascular and metabolic risk, yet they can reduce lean mass as weight comes down. That gap is a design opportunity. The winners in the next wave will be the teams that protect or improve function while the scale is moving. For context on how adjacent geroscience fields evolve when regulators weigh new endpoints, see our piece on FDA reversal on aging clocks.
Three routes to stronger muscle
The 2025 field cohered around three scientific strategies: restore pro-regenerative signaling, calm chronic inflammation that blocks anabolism, and release growth brakes.
Route 1: Restoring PGE2 to restart repair
MF-300 targets 15-hydroxyprostaglandin dehydrogenase, the main enzyme that degrades prostaglandin E2. Think of PGE2 as a local wake-up call for tissue repair. When muscle fibers are damaged, PGE2 helps activate satellite cells, nudges them to proliferate and differentiate, and supports mitochondrial remodeling so new fibers have power, not just size. With age, PGE2 tone diminishes and repair slows. Inhibiting 15-PGDH raises local PGE2, raising the volume on regeneration signals.
This approach does not brute-force growth. It aims to restore a native switch that is already in the muscle playbook. That may matter for safety and for function. If you improve the quality and power of fibers and not just their volume, you should see changes in chair stands and gait, not only in scans.
Key questions for the next phase
- How durable is the effect after dosing stops?
- Does higher PGE2 in older adults behave like youthful PGE2, or does tissue context change the downstream signals?
- Can we show a functional improvement in Short Physical Performance Battery or gait speed within one or two dosing cycles?
Epirium’s Phase 1 readout in September 2025 sets the stage for these tests in 2026.
Route 2: Quieting TNF alpha to lift the anabolic block
Chronic, low-grade inflammation with age, often called inflammaging, blunts muscle protein synthesis and accelerates breakdown. Tumor necrosis factor alpha is a central node in this network. When TNF alpha is high, the signal to build new muscle gets damped and the signal to degrade gets amplified. TNF Pharmaceuticals is running at this target with an oral inhibitor, starting in a high-need group: adults who become frail after a fracture.
Why post-fracture frailty? Because the window is tight and the stakes are obvious. After a hip fracture, for example, muscle deconditioning can spiral quickly. An oral agent that reduces inflammatory brakes and allows rehab to work better could shorten the interval between bed and baseline function. If the drug reduces pain or fatigue enough to increase daily steps, that secondary behavior change can compound the effect. The Phase 2b launch in February 2025 tells us to watch for function-first readouts in 2026.
The risk here is familiar. Over-suppress inflammation and infection risk rises. The bet is that a small-molecule oral inhibitor tuned for older adults can quiet the background noise without muting the immune alarm. Dosing strategies that rise during rehab and taper after recovery could help balance risk and benefit.
Route 3: Releasing myostatin and activin brakes
Myostatin and related ligands signal through activin receptors to keep muscle growth in check. Bimagrumab binds the activin receptor type II and blocks that inhibitory pathway, which can increase lean mass even without heavy training. That is a clean mechanism with a clear biomarker: dual-energy X-ray absorptiometry lean mass goes up.
The September 2025 halt of Lilly’s study combining bimagrumab with tirzepatide will be debated for years. Was it a lack of incremental benefit over a very strong weight loss baseline? Was it safety? Was it trial design? No matter the reason, the message is simple. Mass is not enough. If a drug meaningfully increases lean mass but cannot reliably improve chair stands, gait speed, and fall risk, clinicians will hesitate and regulators will ask for more. The path forward for this class likely lies in better patient selection and functional endpoints that capture quality, not just quantity.
The GLP-1 muscle gap
The modern weight loss agents that act on glucagon-like peptide 1 receptors, and in some cases both glucagon-like peptide 1 and glucose-dependent insulinotropic polypeptide receptors, are changing cardiometabolic medicine. As weight drops, blood pressure, lipids, and liver fat often improve. Yet across studies a meaningful fraction of weight loss comes from lean mass, especially early in the journey. That is not a reason to avoid treatment. It is a reason to plan muscle support from the start. For background on this class, see Semaglutide’s 2025 clock signal.
The practical question for 2026 is simple. Can we pair weight loss with muscle preservation so that the person who loses 20 percent of body weight also stands up faster, walks with confidence, and avoids the post-fracture spiral? Success will not be judged on magnetic resonance scans alone. It will be judged on the kind of outcomes that keep people out of the hospital.
Combination strategies are the likely shape of success. A PGE2-restoring agent that upgrades repair during calorie deficit. An anti-inflammatory that reduces soreness and fatigue during rehab so daily activity rises. A carefully selected growth-release agent in a subgroup with clear anabolic resistance. Each of these can be layered with progressive resistance training and adequate protein. The next winners will be the teams that hardwire these combinations into trials rather than bolting them on as lifestyle advice. For a look at how combination geroscience trials are moving from theory to practice, see our report on plasma exchange geroscience trials.
The endpoints that unlock approval
Regulators have been clear in other fields. When measures predict how people feel and function, they count. When measures track laboratory phenomena without clear links to outcomes, they are supportive at best. For muscle-preserving gerotherapies, a shortlist of endpoints is emerging.
- Grip strength: Fast, low cost, and prognostic. A rise in grip strength is meaningful when it crosses thresholds associated with mobility and self-care. Grip should be paired with a leg-dominant measure to avoid false comfort.
- Gait speed: Usual gait speed over 4 to 6 meters is simple and predictive. Small improvements, on the order of a few tenths of a meter per second, have been associated with better survival and fewer hospitalizations. Trials should standardize distance, footwear, and instructions to reduce noise.
- Short Physical Performance Battery: The SPPB summarizes balance, chair stands, and walking into a single 0 to 12 score. It is practical in busy clinics and sensitive to change over weeks to months. A one-point improvement sustained over time is a target worth pursuing in Phase 2.
- Fall risk and fall events: Time to first fall and rate of falls are gold-standard outcomes but require larger samples and longer follow-up. Creative trial designs can de-risk this by enrolling post-fracture adults or high-risk groups with validated fall history.
- Secondary digital measures: Wearables can capture sit-to-stand transitions, step power, and activity fragmentation. These are not approval endpoints yet, but they can reveal whether a drug changes how people move in daily life, not just in the clinic. If the digital signal aligns with SPPB and falls, it will accelerate confidence.
Sponsors should pre-specify a function-first hierarchy. For example, SPPB as the primary endpoint, with gait speed and time to first fall as co-primary or key secondary endpoints, and lean mass as a supportive biomarker. That stack puts the emphasis where it belongs: on performance.
The 2025 scoreboard and what to watch in 2026
The current scoreboard looks like this.
- Epirium Bio: Positive Phase 1 in September 2025 for MF-300, a 15-PGDH inhibitor that aims to restore PGE2 tone and muscle repair. What to watch in 2026: dose ranging for function, a clean safety profile in older adults, and early signals in SPPB, chair stands, and gait speed.
- TNF Pharmaceuticals: Phase 2b launch in February 2025 for an oral TNF alpha inhibitor in post-fracture frailty. What to watch in 2026: whether dampening inflammation accelerates rehab, reduces pain or fatigue, and increases daily steps enough to shift fall risk within a season.
- Eli Lilly and bimagrumab combinations: Study halted in September 2025. What to watch in 2026: retooled designs that focus on function-first outcomes and subgroups with clear anabolic resistance, along with better integration of resistance training.
Beyond these anchors, expect a steady flow of small molecules and biologics that modulate muscle stem cell niches, mitochondrial biogenesis, and neuromuscular junction health. Expect more hybrid trials that combine pharmacology with structured strength programs and protein targets, measured not by diaries but by connected devices that can prove adherence.
How the first approvals could land by 2026 to 2027
A slightly accelerationist case is emerging. If sponsors run function-first trials, pick high-risk groups, and allow combination strategies, the first anti-frailty approval could arrive as early as 2026 to 2027. Here is a realistic playbook.
- Pick populations where events are frequent: Post-fracture adults and older adults with recent hospitalizations have more falls and functional decline per unit time. That lowers sample sizes and increases power.
- Choose endpoints that regulators and clinicians trust: Make SPPB the primary. Anchor to gait speed and falls. Use lean mass as a supportive biomarker, not a surrogate for function.
- Build combinations into the protocol: Do not ask sites to add exercise on top. Provide a structured, progressive resistance program with adherence tools. If the investigational drug targets repair or inflammation, design dosing around the rehab window. In weight loss settings, start muscle support when calorie deficit begins, not months later.
- Use adaptive designs with early functional gates: If a dose does not move chair stands or gait speed by a prespecified margin by week eight, drop it. Concentrate exposure on doses that move function.
- Plan for real-world deployment: Payers will ask how to deliver this at scale. Collect data on home-based strength programs, remote monitoring, and safety in older adults with polypharmacy. Show that the protocol can survive outside the academic center.
Regulators reward clarity. A program that connects mechanism to function and function to hard outcomes can move quickly. The science is ready. The clinic is ready. The logistics are finally catchable because digital tools can confirm that people are doing the exercises that make the drugs work.
Practical implications for clinicians and builders
For clinicians, the near-term actions are straightforward.
- Screen for muscle function now: Add grip strength and usual gait speed to annual visits for adults over 65 or anyone beginning a weight loss program. Do not wait for a prescription to start resistance training.
- Pair weight loss with muscle protection: Start progressive resistance and protein targets at the same time as calorie deficit. If a patient is on a glucagon-like peptide 1 pathway drug, plan for strength, not just scale.
- Plan for recovery windows: After fractures or surgeries, use the most intensive phase of rehab to test whether anti-inflammatory or pro-repair approaches can accelerate returns to baseline.
For builders and sponsors, the message is to design for function from day one.
- Translate mechanism into a functional hypothesis: If the drug improves repair quality, chair stands should improve; if it reduces inflammation, daily step power should rise; if it releases growth brakes, stair ascent time should fall. Then measure the thing the mechanism should move.
- Center the patient journey: Map where fatigue, pain, and fear of falling block progress in the first four to eight weeks after a setback. Target those weeks. That is where drugs and rehab can synergize.
- Pre-negotiate with payers on endpoints: Identify the functional thresholds that trigger coverage and continued use. Design trials that deliver those thresholds inside six months.
The bottom line
2025 will be remembered as the year muscle medicine stepped into the clinic. A PGE2-restoring strategy showed early human promise. An oral anti-inflammatory started a pivotal test in a high-need group. A growth-release combo stumbled in a way that clarified what success should look like. The field learned the lesson that matters. In the gerotherapy era, muscle is not a vanity metric. It is the platform for resilience.
The next two years will reward teams that aim at function first, embrace combinations, and choose endpoints that let regulators and clinicians say yes. If that happens, the first approved anti-frailty drug could arrive earlier than many expect. When it does, it will not be because we chased mass for its own sake. It will be because we treated muscle as the organ that lets us keep living the lives we want.