Colchicine vs Clonal Aging: Slowing TET2-Driven Mutations
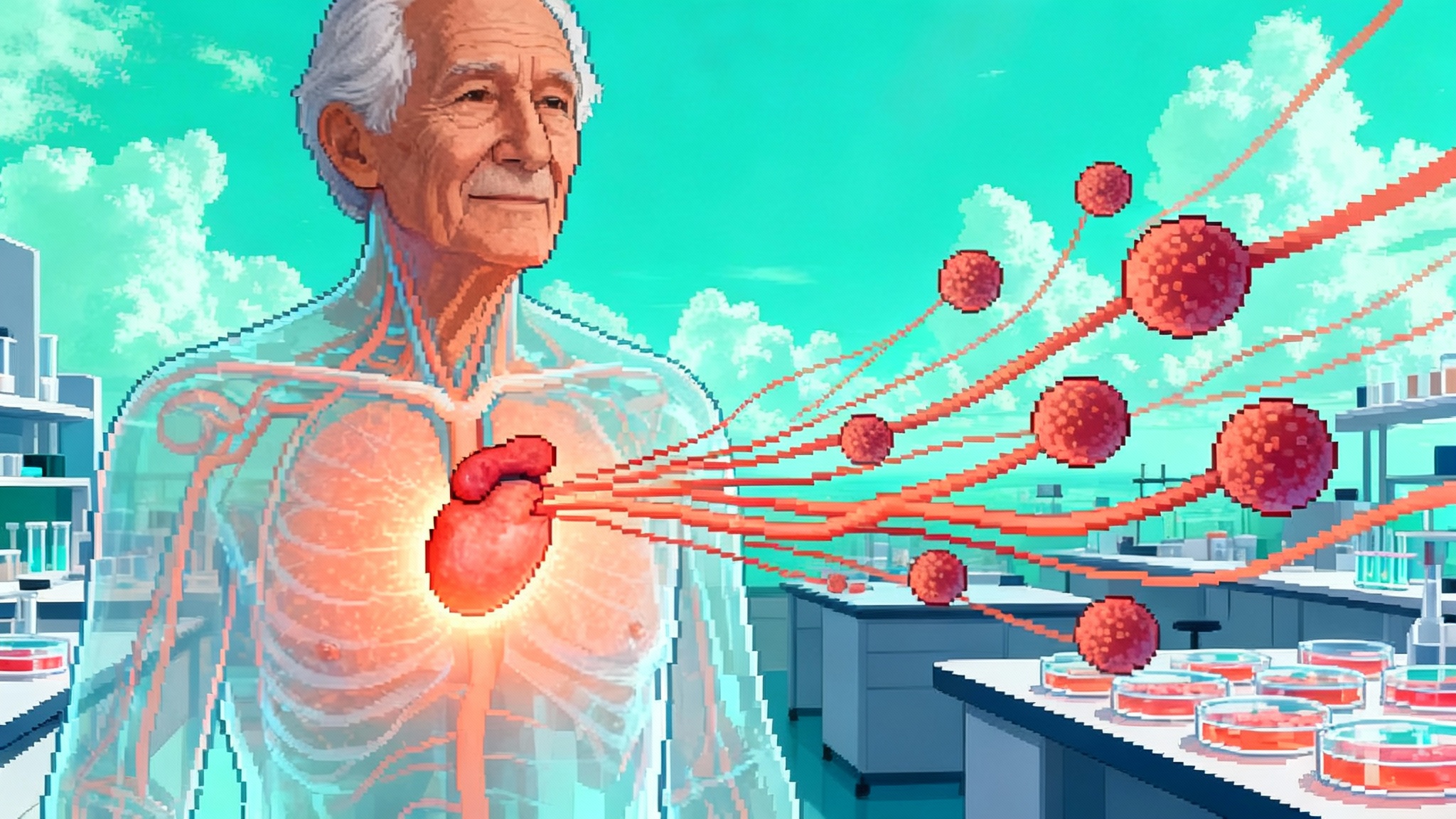
Fresh August 2025 cardiology genetics data suggest that low-dose colchicine may slow TET2-driven clonal hematopoiesis in people with coronary disease. Here is what CHIP is, who to test, and how to act while we wait for genotype-enriched trials.
A quiet inflection point in cardiology and aging
In late August 2025, a genetics substudy from the LoDoCo2 cardiovascular outcomes trial reported a subtle but important signal: among people with chronic coronary disease, those randomized to low-dose colchicine showed slower growth of TET2-driven clonal hematopoiesis. Overall clone growth rose about 15 percent per year on placebo and 6 percent on colchicine, a difference that did not reach statistical significance. In carriers of TET2 mutations, clone size grew roughly 30 percent per year on placebo and about 9 percent with colchicine, a significant interaction, as detailed in the LoDoCo2 CHIP substudy in JACC.
The idea is provocative: an inexpensive anti-inflammatory might modulate the somatic evolution that accompanies human aging.
Key takeaways
- CHIP is common with age and tracks with higher cardiovascular and cancer risk.
- TET2 biology links inflammation to atherosclerosis, creating a plausible target for anti-inflammatory therapy.
- Low-dose colchicine may slow TET2 clone growth, but this is exploratory and needs confirmation in genotype-enriched trials.
What exactly is CHIP, and why it matters
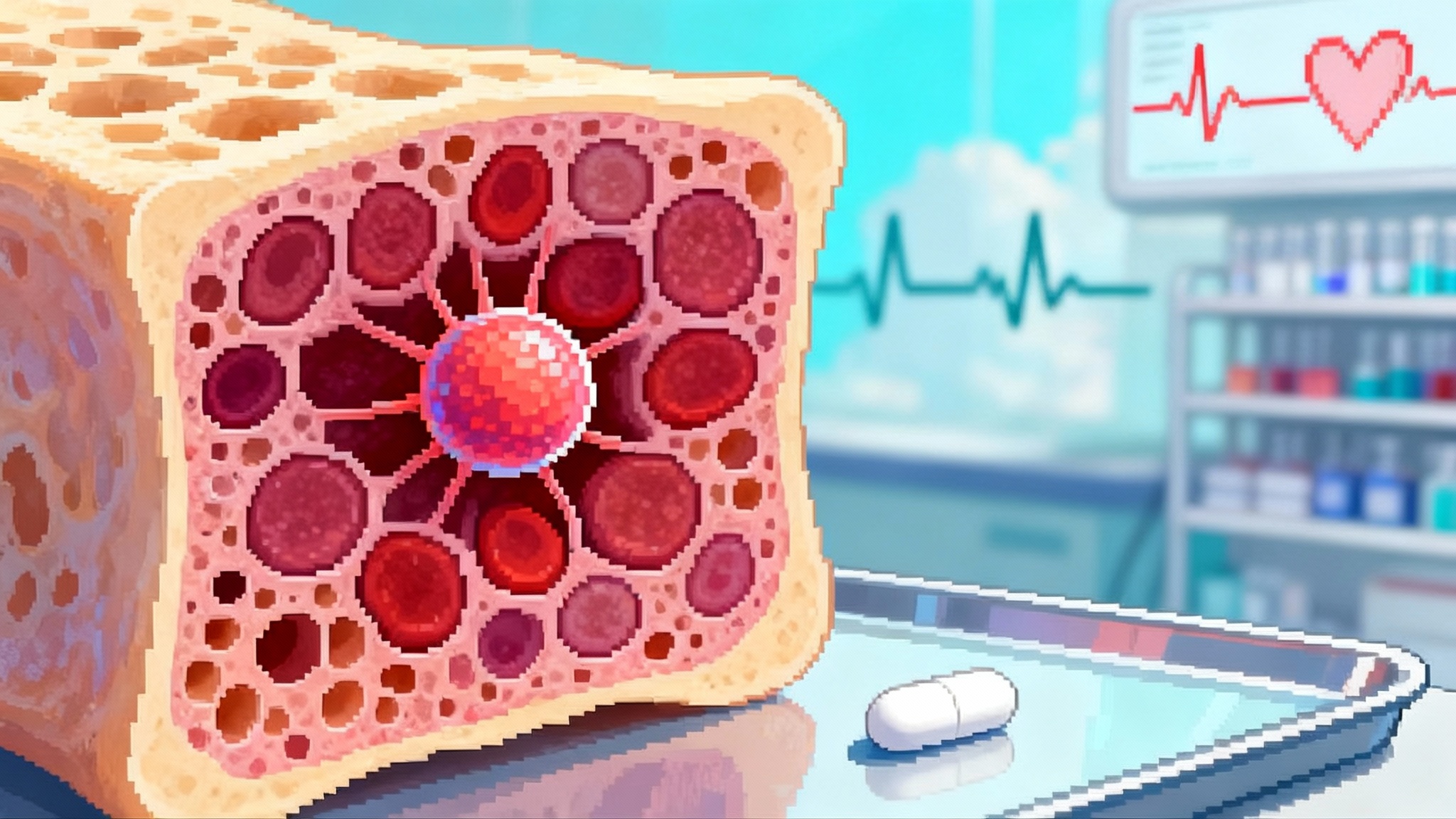
Clonal hematopoiesis of indeterminate potential, or CHIP, refers to acquired DNA mutations in blood stem cells that give a small subset of cells a growth edge. The standard definition requires a variant allele fraction of at least 2 percent. With modern sequencing, most clinical labs can detect even smaller clones, but risk rises as clone size rises.
Common driver genes include DNMT3A, TET2, ASXL1, JAK2, SF3B1, SRSF2, IDH1, IDH2, TP53, and PPM1D. These changes are usually asymptomatic yet consistently linked to three domains of risk:
- Cardiovascular disease: higher rates of myocardial infarction, stroke, heart failure, and atrial fibrillation.
- Hematologic malignancy: a small but real increase in myeloid cancer risk over years, especially with high-risk genes and larger clone sizes.
- All-cause mortality: likely driven by cardiovascular outcomes and systemic inflammation.
Mechanistically, TET2-mutated blood cells tend to overproduce interleukin-1β and other mediators that amplify innate immune activation in vascular tissue. In short, a molecular change in the marrow can tilt the inflammatory set point throughout the body.
Somatic evolution in the bloodstream
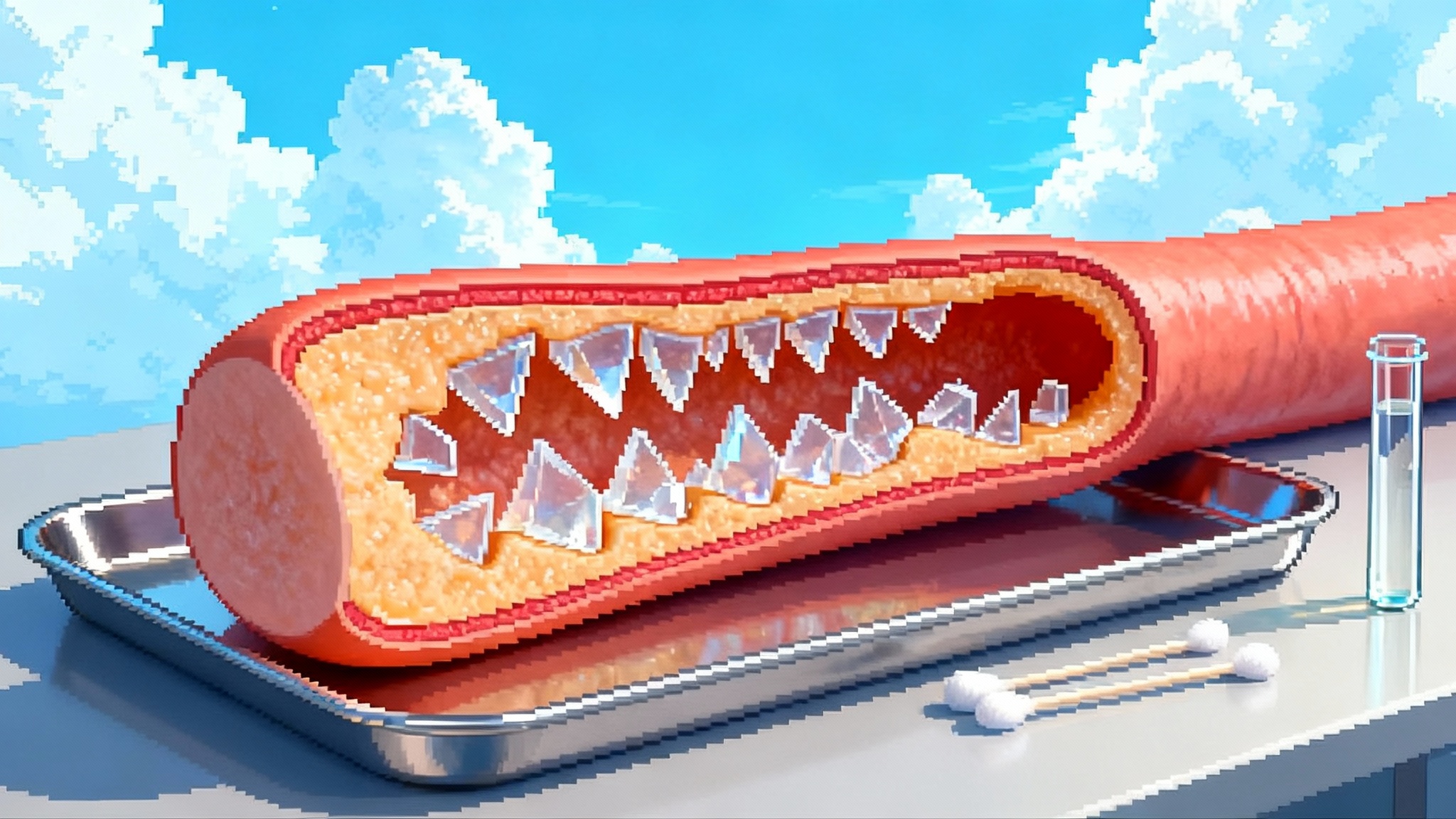
Every person accumulates somatic mutations across life. Most are neutral. A few confer a tissue-specific fitness advantage. In marrow, constant self-renewal and differentiation create an environment where small selective advantages compound over time.
Selection pressures are not purely cell intrinsic. Aging brings reduced stem cell fitness, altered niche signals, and low-grade inflammation. TET2 loss of function can heighten inflammatory signaling and nudge progenitors toward myeloid fates, creating a feedback loop where inflammation helps the clone and the clone promotes inflammation.
Clone trajectories vary. Some stay flat for years; others rise by 10 to 30 percent in variant allele fraction annually. Larger clones carry more risk. Multiple small clones can add up. A JAK2 V617F mutation may carry elevated thrombotic risk even at modest clone sizes. What matters clinically is the slope over time, the gene involved, and the host’s risk context.
Why colchicine might matter for CHIP
Colchicine has been used for centuries to calm inflammation in gout and pericarditis. At low doses it interferes with microtubule polymerization in innate immune cells, blunting chemotaxis, adhesion, and inflammasome assembly. The NLRP3 inflammasome drives the maturation of interleukin-1β, strongly implicated in TET2-mutant biology.
Preclinical and human observational data hinted that colchicine might be particularly relevant to TET2-driven clonal hematopoiesis. In 2024, investigators showed that colchicine prevented accelerated atherosclerosis in mice with TET2-mutant clonal hematopoiesis and appeared to attenuate the association between TET2 mutations and myocardial infarction in humans prescribed colchicine, as summarized in the TET2 CH atherosclerosis study.
These mechanistic threads set the stage for the 2025 LoDoCo2 substudy signal. If inflammatory tone acts like a tailwind for certain clones, dialing it down could remove the selective advantage and slow clonal growth.
The 2025 signal, unpacked
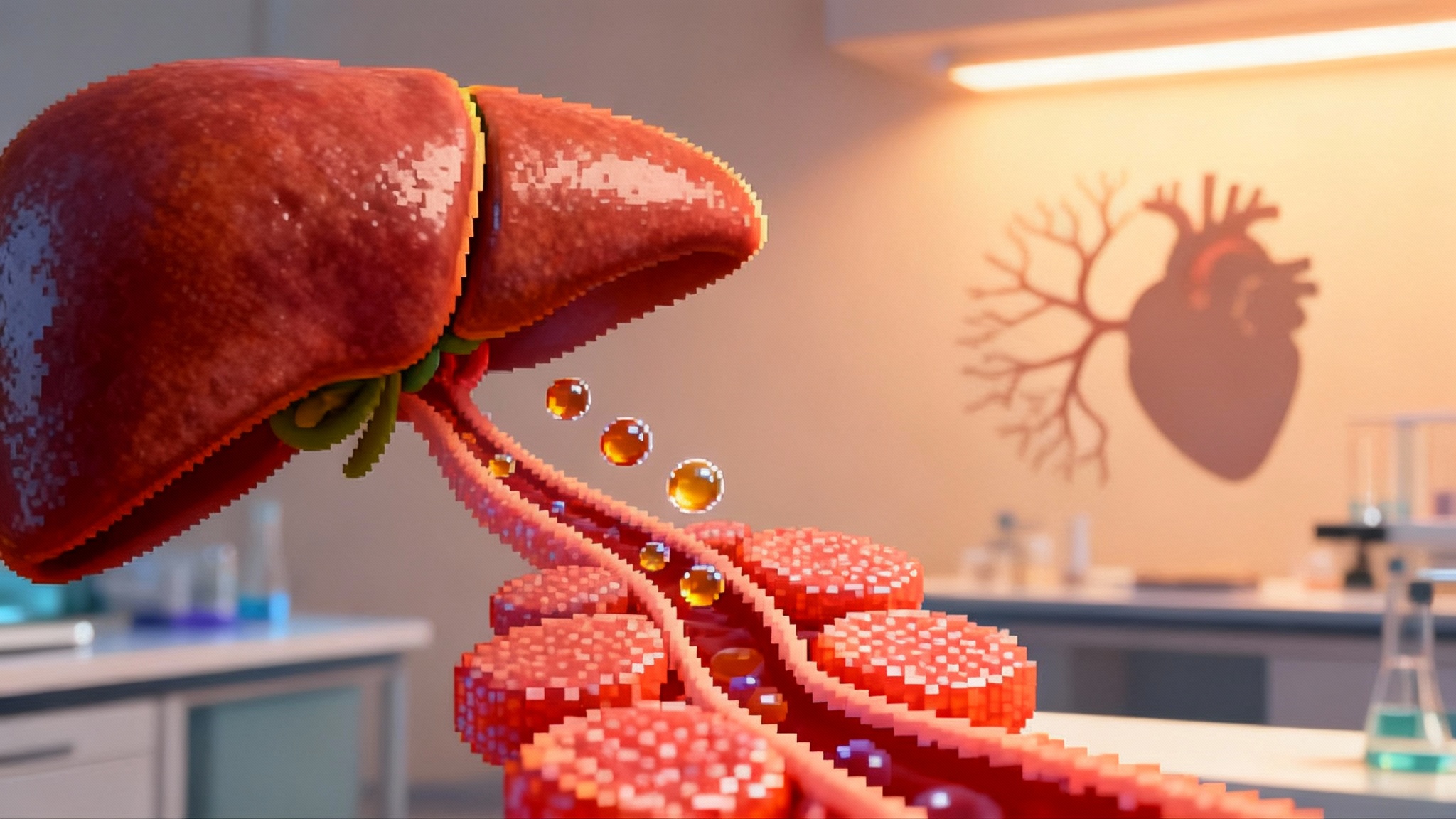
The LoDoCo2 genetics substudy drew serial blood samples at four time points and sequenced for CHIP mutations. Across all detected CHIP, placebo recipients saw about a 14.9 percent annual increase in clone size, while colchicine recipients saw a 6.3 percent increase that did not meet statistical significance. In gene-specific analysis, TET2 clones in the placebo arm grew around 29.6 percent per year versus 9.1 percent per year with colchicine, a significant difference by interaction testing. Interleukin-6 rose less over time with colchicine among people with non-DNMT3A CHIP, consistent with reduced inflammatory tone.
Important caveats apply. This was exploratory. Participants were not randomized by CHIP status or genotype. The overall CHIP effect did not reach significance. The study cannot prove causality for TET2 clone slowing, nor can it tell us whether such slowing translates into fewer heart attacks, strokes, or cancers in CHIP carriers.
Who to screen for CHIP, and how
There are no universal screening guidelines. The decision depends on goals, risk profile, and how results will be used.
- Consider targeted CHIP testing in older adults with established coronary disease, especially with residual inflammatory risk such as elevated high-sensitivity CRP or a family history of early cardiovascular disease.
- Consider testing after chemotherapy or radiation exposure, particularly if blood counts drift or macrocytosis appears.
- Evaluate unexplained cytopenias, persistent macrocytosis, or monocytosis with a myeloid panel.
- Use caution with population-wide screening of asymptomatic adults if results will not change management or might trigger anxiety and unnecessary procedures.
Panels and practical details
- Genes: at minimum include DNMT3A, TET2, ASXL1, JAK2, SF3B1, SRSF2, IDH1, IDH2, TP53, and PPM1D.
- Depth: aim for error-corrected sequencing when available, with a reliable limit of detection near 1 to 2 percent variant allele fraction.
- Calling thresholds: the traditional CHIP cutoff is 2 percent VAF. Below that, some labs will report low-level clonal hematopoiesis with uncertain risk. Risk scales with clone size and the gene involved.
- Follow-up: repeat testing at 6 to 12 months to establish a personal slope. Rapid growth or high-risk genotypes may prompt hematology input.
VAF thresholds that matter
- 2 percent VAF: commonly used threshold to define CHIP.
- 5 to 10 percent VAF: risk becomes more meaningful for cardiovascular events in many cohorts.
- Greater than 10 percent VAF or multiple clones: higher risk and higher likelihood of progression to cytopenias over years, especially with TP53 or spliceosome mutations.
- JAK2 V617F: even small clones can carry thrombotic risk and may warrant more aggressive cardiovascular risk management and hematology review.
Counseling points
- Most people with CHIP will never develop a blood cancer.
- The near-term risk to focus on is cardiovascular, which is modifiable with standard therapy and lifestyle.
- Clone size and inflammation are not destiny. They are dials you can potentially turn.
Colchicine in practice for people with CHIP
Low-dose colchicine already has a role in secondary prevention for stable coronary disease in many regions. The CHIP signal adds a new possible reason to use it in selected patients.
- Dose: 0.5 mg daily where available or 0.6 mg daily in the United States.
- Benefits: in large cardiovascular trials, colchicine reduced major adverse events by roughly 23 to 31 percent in broad coronary artery disease populations. The new substudy suggests a potential additional benefit of slowing TET2 clone growth.
- Side effects: the most common is gastrointestinal upset, which often improves after one to two weeks or with temporary dose interruption.
- Drug interactions: avoid with strong CYP3A4 or P-glycoprotein inhibitors such as clarithromycin and certain azoles. Use caution with high-dose statins or in advanced renal or hepatic impairment.
- Monitoring: routine labs are not required for everyone, but consider checking creatinine and liver enzymes when there is comorbidity, and creatine kinase if muscle symptoms occur. If cytopenias appear, pause colchicine and reassess.
A reasonable, individualized strategy for an older adult with coronary disease and a documented TET2 clone could be to prioritize low-dose colchicine as part of secondary prevention, alongside statins, antiplatelet therapy when indicated, and aggressive risk factor control. This is not yet a guideline-directed use of genotype to select therapy.
Clinical caveats and unanswered questions
- Generalizability: the observed slowing was most evident in TET2, not across all genes. DNMT3A, the most common CHIP driver, may behave differently.
- Outcomes linkage: we still need proof that slowing clonal growth changes hard outcomes like myocardial infarction or progression to myeloid malignancy.
- Optimal candidates: should we focus on people with high VAF TET2, on multiple non-DNMT3A clones, or on anyone with CHIP and residual inflammatory risk?
- Duration: how long must colchicine be taken to influence clonal dynamics meaningfully, and are effects reversible if stopped?
- Safety in frailty: in very old or frail adults, the risk-benefit balance of long-term colchicine needs careful assessment.
The trials we need next
1) Genotype-enriched randomized trials
- Enroll adults with coronary disease and TET2 CHIP at or above a VAF threshold such as 2 to 5 percent.
- Randomize to low-dose colchicine or matching placebo on top of guideline-directed therapy.
- Primary endpoints: change in TET2 VAF over 12 to 24 months and change in inflammatory biomarkers.
- Key secondary endpoints: composite cardiovascular outcomes, incident atrial fibrillation, and time to hematologic neoplasm.
- Methods: error-corrected sequencing with centralized calling and predefined rules for clone tracking; adjudicated clinical events.
2) Comparative anti-inflammatory strategies
- Test colchicine against an IL-1β pathway inhibitor or an NLRP3 inhibitor in TET2 carriers to see whether deeper inflammasome blockade yields greater clone slowing or superior clinical outcomes.
3) Prevention in high-risk oncology survivors
- Enroll survivors of chemotherapy or radiation with CHIP and high baseline CRP to assess whether colchicine reduces clone growth and cardiovascular events.
4) Implementation science
- Study how to deliver CHIP-informed care in cardiology clinics without creating anxiety or overtesting. Evaluate shared decision tools, genetic counseling models, and payer coverage.
Beyond CHIP: first levers on aging
If a low-cost anti-inflammatory can slow the growth of a common age-acquired mutation, it hints at something larger. Aging is partly the story of somatic evolution, tissue by tissue. The selective pressures that favor certain clones are often environmental and modifiable. In marrow, chronic inflammation can act like fertilizer. Turn down the fertilizer, and the fastest growers may slow.
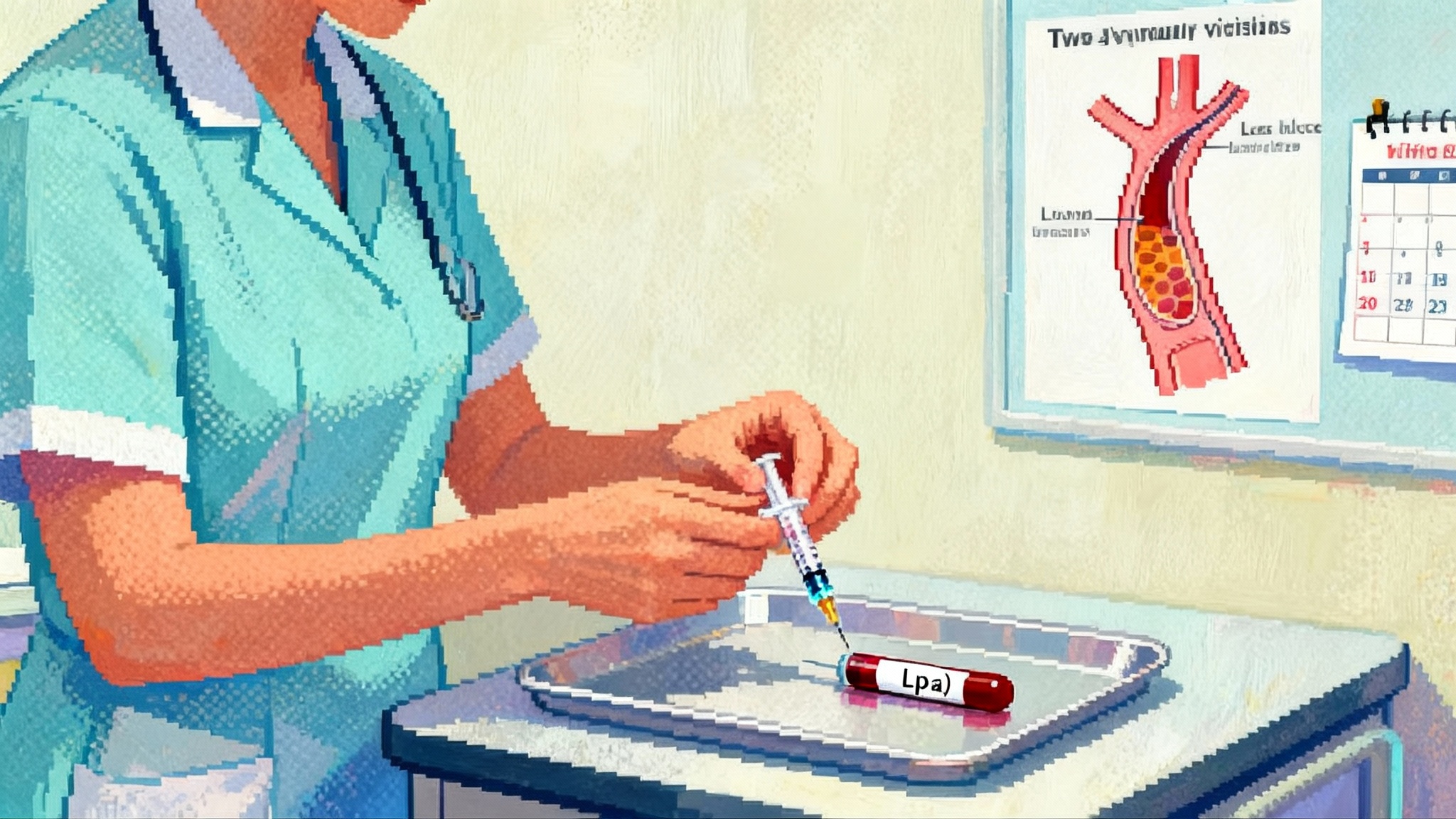
The broader cardiometabolic landscape is shifting in parallel, from how Lp(a) shots reset risk to the GLP-1 muscle-sparing race. Environmental drivers matter too, as shown by emerging links between microplastics and vascular aging.
There are ethical guardrails. Screening for CHIP should be optional, informed, and tied to an action plan. Clinicians should avoid fatalistic language. Patients should know that most clones are slow and that overall risk is modifiable with blood pressure control, lipids, exercise, sleep, and diet.
The bottom line
- CHIP is common with age and matters for both cardiovascular and cancer risk.
- In August 2025, an exploratory LoDoCo2 substudy associated low-dose colchicine with slower growth of TET2-driven clones and smaller rises in inflammatory markers, aligning with prior mechanistic work.
- Screening should be targeted and thoughtful, using panels that capture major CHIP drivers and VAF thresholds that map to risk.
- Colchicine may become a practical lever to modify a piece of aging biology at the bedside, pending dedicated genotype-enriched trials that test clinical outcomes.