The GLP-1 Muscle-Sparing Race to Real Longevity Gains
New 2025 data suggest GLP-1 combinations can shift weight loss toward fat while protecting muscle. Here is how ActRII and myostatin strategies, amylin add-ons, and smarter training could make weight loss longevity-safe for older adults.
The next frontier of obesity care is better weight loss, not just more
The first wave of GLP-1 and incretin therapies made double digit weight loss common. Yet a stubborn blind spot remains. Along with fat, people lose lean mass. For a 45 year old with plenty of reserve, losing roughly one quarter of total weight as lean tissue may be a tolerable tradeoff. For a 68 year old with creeping sarcopenia, it can be the difference between independent living and a fall, a fracture, a hospitalization. Summer to fall 2025 brought a decisive shift. Conference readouts and pipeline moves signal a race to make GLP-1s longevity safe by preserving muscle while amplifying fat loss.
Two developments stood out. First, mid year presentations and press materials from the BELIEVE Phase 2b program reported that combining an ActRII blocker with semaglutide pushed the quality of weight loss toward fat while protecting lean mass, with a high proportion of total loss coming from adipose tissue rather than muscle. BELIEVE also sat beside an intriguing late breaking poster on a continuous protein sensor designed to monitor muscle catabolism and protein intake in real time, hinting at a near future where clinicians can titrate nutrition and training around pharmacologic weight loss with actual biosignals rather than guesswork. See the American Diabetes Association’s concise recap: BELIEVE combination preserved lean mass.
Second, EASD 2025 brought full 26 week results from Regeneron’s COURAGE trial, which combined semaglutide with a myostatin neutralizing antibody. The addition of the antibody prevented roughly half the lean mass loss seen with semaglutide alone and increased fat loss, with early functional and cardiometabolic trends moving in the right direction. The interim dataset published in June framed the stakes clearly, and the complete 26 week analysis preserved the signal while underscoring tolerability boundaries for more aggressive triplets. Sponsor summary: preserving lean mass with trevogrumab plus semaglutide.
Together these updates mark a pivot. The GLP-1 era is maturing from how much weight to what kind of weight. The center of gravity is moving from appetite to architecture, from pounds to partitioning.
Why lean mass protection is a longevity lever
Lean tissue is not a vanity metric. It is a multi organ reserve that underwrites healthy aging.
- Sarcopenia and frailty: Losing muscle and strength increases fall risk, fracture risk, disability, and mortality. Even modest declines in gait speed and grip strength predict hospitalizations and shortened survival. For broader context on frailty biology, see our overview of the frailty trial and aging vaccines.
- Metabolic resilience: Skeletal muscle is the largest site of glucose disposal and a major regulator of resting energy expenditure. Preserving it buffers against glucose intolerance, weight regain, and the energy dip that makes maintenance so hard as cardiometabolic risk management evolves with RNA shots for Lp(a).
- Functional independence: Muscle mass and quality determine stair climb power, balance, and the capacity to recover from illness. In older adults, those functions are the hard endpoints that matter.
If obesity therapies can shift weight loss toward fat while maintaining or improving muscle performance, the downstream could be fewer falls, fractures, deconditioning spirals, admissions, and deaths. That is the true longevity prize, not a lower number on a smart scale.
The biology behind muscle sparing strategies
Three complementary levers dominate the 2025 playbook.
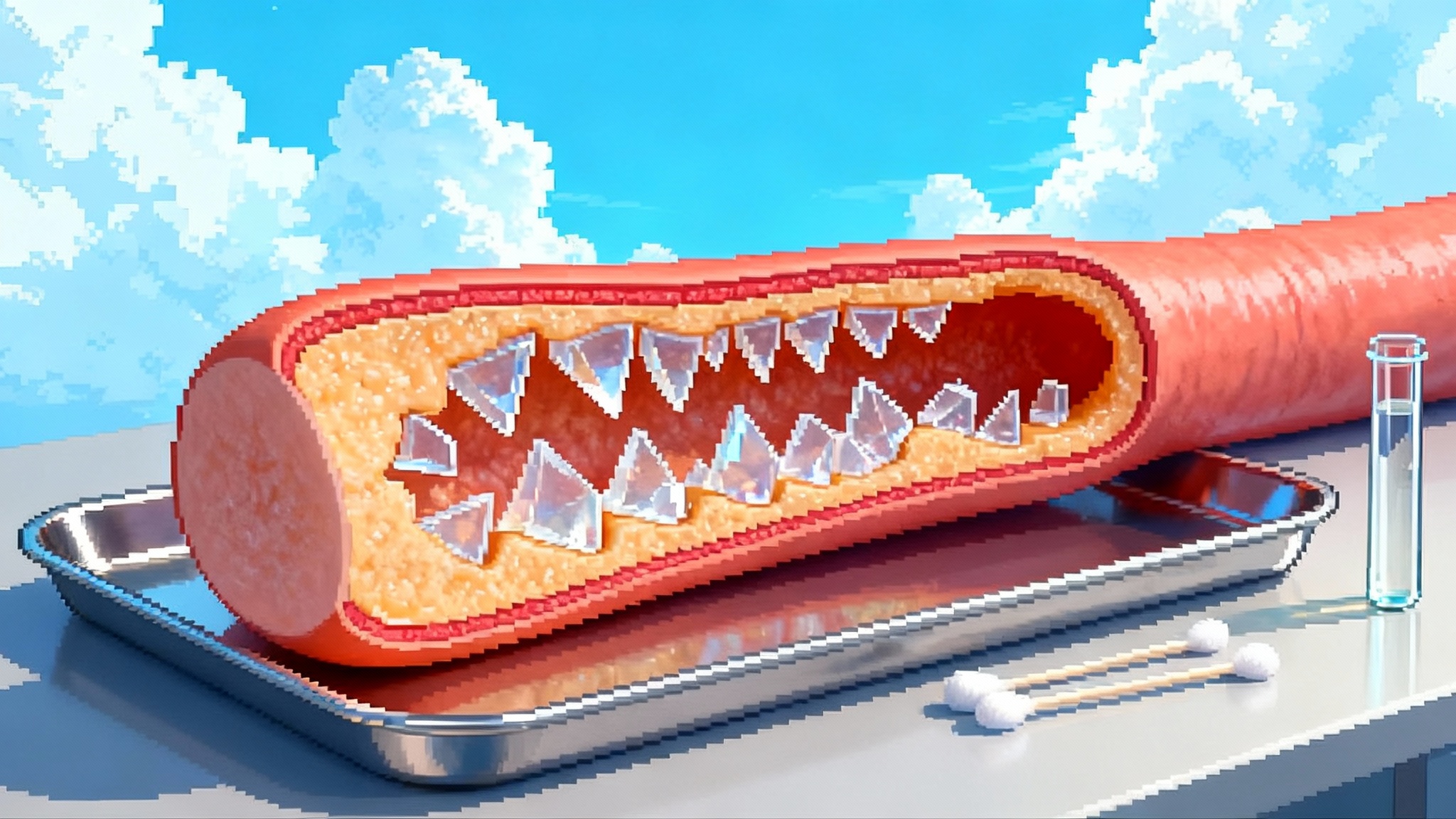
- ActRII pathway blockade to disinhibit muscle
- Myostatin and activins are brake signals that restrain muscle growth. Antibodies that block the activin type II receptors, or neutralize myostatin directly, release that brake. Bimagrumab, trevogrumab, and other agents in this family aim to keep or grow muscle during negative energy balance.
- The tradeoffs are nuanced. Overly broad blockade can have safety limits, and past attempts that saw limited efficacy taught developers to target more selectively and to combine rationally with GLP-1s rather than replace them.
- Amylin co agonism to deepen satiety without excessive lean loss
- Amylin analogs like cagrilintide paired with semaglutide in co formulated regimens can amplify weight loss and blunt compensatory hunger. As later stage programs mature, dedicated body composition substudies are clarifying whether amylin plus GLP-1 tilts loss more toward fat compared with GLP-1 alone. Early 2025 readouts showed strong efficacy and glycemic benefits, with body composition analyses expected to inform which populations benefit most.
- Training and protein to defend contractile tissue
- Resistance training two to three days per week and higher protein intake, often 1.2 to 1.6 g per kilogram of body weight per day for older adults during weight loss, remain the only proven, scalable tools to protect lean mass at the bedside. Leucine rich proteins, intelligent distribution across meals, and progressive overload work synergistically with pharmacotherapy. For perspective on what works versus hype, see the NIH taurine verdict. The difference between a GLP-1 only plan and a GLP-1 plus lifting plus protein plan can be measured in kilograms of muscle preserved and in the ability to get up from a chair at speed.
How trials are evolving in 2025
Designs are catching up to what clinicians care about.
- Body composition as a primary readout: Sponsors are elevating DEXA measured lean mass and fat mass from exploratory to primary or key secondary endpoints. Trials are also using MRI of visceral fat and muscle quality metrics to map fat from the liver and viscera while tracking intramuscular fat and muscle volume.
- Functional outcomes: Gait speed, timed stair climb power, and grip strength are moving into hierarchical outcome sets. These capture not just mass, but use. In older adults and in sarcopenic obesity, function is the practical currency.
- Real world evidence: Claims and registry based studies are beginning to link body composition friendly regimens to concrete events like falls, fracture diagnoses, and 30 day readmissions. Expect longitudinal EHR data to stratify patients by baseline frailty and to compare GLP-1 monotherapy versus muscle sparing combinations or structured exercise nutrition adjuncts.
Summer to fall 2025: what changed
- ActRII and myostatin combinations cleared an important bar. The BELIEVE Phase 2b experience pairing ActRII blockade with a GLP-1 documented a higher fraction of fat loss with better lean mass preservation, and Regeneron’s COURAGE program reproduced the concept in a different antibody target with semaglutide. The dose response and tolerability natural limits of triplets also came into view.
- A first glimpse of consumer grade muscle nutrition telemetry emerged. A continuous protein sensor proof of concept appeared among late breaking data, pointing to aptamer based biosensors that can detect amino acid flux associated with protein intake and muscle breakdown. If validated clinically, such sensors could individualize protein timing and the up titration of resistance training around dose escalations, nausea windows, and plateaus.
- Pipelines reshuffled. One large sponsor halted a type 2 diabetes cohort in a muscle sparing antibody program while continuing a companion obesity study, a reminder that even validated mechanisms must meet evolving regulatory and commercial bars. Oral GLP-1 contenders diverged, with one major player exiting a daily pill program after a liver safety signal and another advancing an oral small molecule GLP-1 through multiple Phase 3 successes. None of these oral agents, on their own, solve the lean mass problem, but they will broaden access and set the stage for muscle conscious co therapies.
The competitive landscape, simplified
Antibody and co therapy classes aimed at preserving muscle
- ActRII blockers and myostatin neutralizers: Multiple sponsors are advancing agents that either block activin type II receptors or neutralize myostatin. The goal is to prevent the typical one quarter lean component of total loss seen with GLP-1 monotherapy, especially in older or sarcopenic patients.
- Androgen receptor modulators: Selective androgen receptor modulators are being tested with GLP-1s to preserve lean mass and add incremental fat loss, with early trials using DEXA and functional tests like stair climb as co primaries.
- Amylin combinations: Cagrilintide plus semaglutide is the flagship. The efficacy bar is high and the tolerability window is narrow. Body composition substudies across diabetic and non diabetic populations will decide where and how it fits.
Oral incretin pills
- Non peptide oral GLP-1s are approaching the market. Their strategic role in a muscle sparing era may be as a backbone for combinations or as a mass market option where injections are a barrier. Body composition data will be essential, but durability, adherence, and access could matter more in practice.
Emerging consumer and clinic tech
- Continuous protein and muscle status biosensors: The late breaking aptamer based protein sensor suggests a coming wave of wearables that track amino acid surges from meals and signals of muscle breakdown. In clinics, expect streamlined DEXA access, low dose CT or MRI body composition modules, and dynamometers and gait mats embedded in routine visits.
What to do now in clinic
This is not just about new drugs. It is a protocol mindset.
-
Who should consider a combination or structured adjuncts
- Adults over 60 with clear sarcopenia or frailty risk starting an incretin
- Anyone beginning a GLP-1 with a history of falls, osteoporosis, or a major surgery in the next year
- Athletes or physically demanding workers who cannot afford a strength dip during rapid weight loss
- Patients who plateau early or show clear signs of low protein intake or disuse
-
The minimum viable muscle protection stack
- Resistance training: Two to three non consecutive days weekly. Prioritize multi joint movements, aim for 8 to 12 hard sets per major muscle group each week, and progress load gradually. Pair with light daily activity to maintain energy expenditure.
- Protein: 1.2 to 1.6 g per kilogram body weight per day for older adults during active weight loss, split evenly over three to four meals. Anchor meals with 25 to 40 grams of protein and at least 2 to 3 grams of leucine per meal. Add a casein rich snack near bedtime in early phases of treatment if daily targets are not met.
- Micronutrients and bone: Ensure adequate calcium and vitamin D. Screen for osteoporosis if indicated. Consider creatine monohydrate in selected patients, especially those who struggle to hit protein targets and who have no contraindications.
- Track what matters: Baseline and follow up DEXA at six months if feasible, then annually. Add a simple functional battery at each visit, such as 5 times sit to stand, 4 meter gait speed, and grip strength.
-
When to escalate beyond lifestyle plus GLP-1
- Older adults with documented lean mass loss beyond expected class averages despite adherent training and protein
- Patients whose function is declining as weight drops
- Those with very low baseline lean mass or with a history suggesting anabolic resistance
In these groups, a discussion about clinical trials, or about future access to myostatin or ActRII pathway inhibitors once approved, is appropriate.
What to watch in 2025 to 2026
- Pivotal and near pivotal combination readouts: Full year COURAGE maintenance data will test whether early lean mass preservation translates into sustained performance and whether triplet strategies can stay tolerable. Next wave ActRII and myostatin programs will define which mechanism, dose interval, and combination partners are best suited for older adults.
- Body composition enriched endpoints: Expect more trials to make DEXA or MRI primary or co primary, alongside functional tests like gait speed, stair climb power, and grip. Sponsors that embrace a composite success definition weight loss plus fat fraction plus function will be set up for payer and regulator conversations.
- Reimbursement and coverage: Medicare wide coverage for anti obesity drugs remains unsettled. Federal proposals to broaden access stalled in spring 2025, while bills to expand coverage continue to work through Congress. For muscle preserving add ons, the key will be demonstrating more than pretty DEXA scans. Health systems and payers will ask for fracture reductions, fewer falls, lower admissions, shorter rehab stays, and durable independence in older beneficiaries.
- Hard outcomes that prove longevity value: Does a muscle centric strategy cut fractures by double digits, prevent deconditioning admissions, and reduce mortality in high risk patients over two to three years. There is a path to show this with pragmatic trials and linked claims data. If the signal emerges, it will transform reimbursement and standard of care.
- Oral GLP-1 timelines and positioning: As oral agents file globally, watch for head to head comparisons on adherence and access. They will not remove the need for muscle focused strategies, but they could make combinations simpler to use.
- Consumer biosensors crossing into practice: The moment a protein or muscle status wearable proves reliable in daily life, expect it to plug into remote coaching and to reshape how clinicians titrate protein and resistance training around dose escalations and side effect windows.
The bottom line
The GLP-1 revolution made meaningful weight loss routine. The 2025 pivot is making that weight loss safer for aging bodies by sparing muscle. The science is finally aimed at what patients and clinicians care about most: function, independence, and resilience. The winners in 2026 will be those who prove not just lower weight, but stronger people who fall less, fracture less, and live more years on their feet.