What a 117-year-old taught us about aging and disease
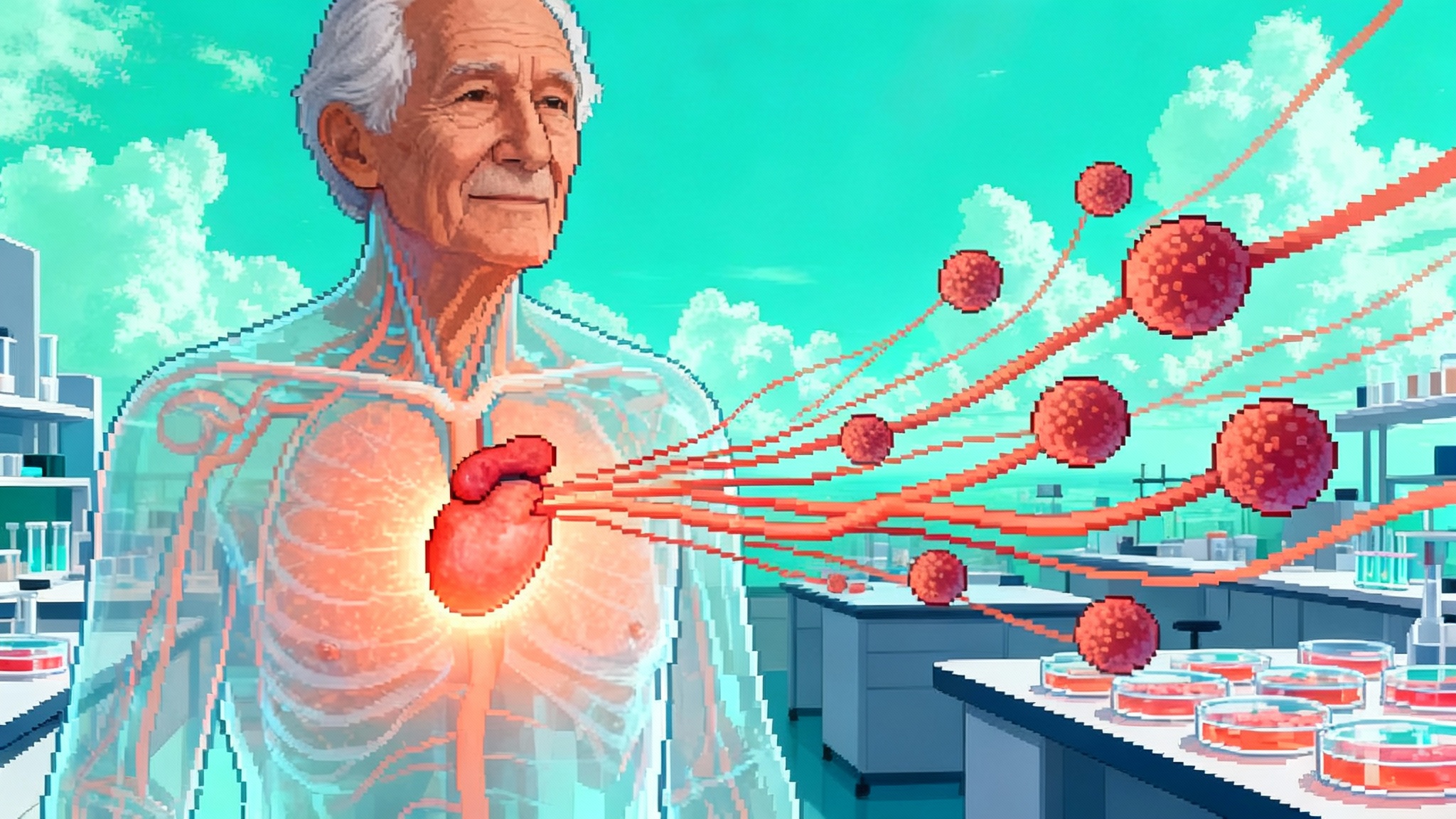
A 2025 case study of supercentenarian Maria Branyas Morera reveals low inflammation, a youthful microbiome, protective genes, and a younger epigenome. The findings shift longevity science toward resilience and trial designs that measure recovery and function, not just age.
A single 117-year-old, a new map for aging
In 2025, researchers published a multi-omics portrait of Maria Branyas Morera, who died in 2024 at 117. The case, reported in Cell Reports Medicine, reads like a paradox. Extreme chronological age coexisted with signals of biological youth, including low systemic inflammation, a microbiome with youthful hallmarks, protective genetic variants, and a younger epigenetic profile. The authors argue that aging and disease can, under certain conditions, be uncoupled, a claim with major implications for longevity science and clinical trials. See the primary paper: Cell Reports Medicine multi-omics case.
The study does not claim time stood still in her cells. There were unmistakable signs of advanced age, such as short telomeres and immune changes that usually track with late life. Yet the signature that stood out was a set of protective systems that appeared to buffer damage, sustain function, and keep disease at bay. For a news overview, see the El País English summary and quotes.
The central signal: decoupling age from disease
The team sampled saliva, blood, urine, and stool during her final years, then layered genomics, transcriptomics, proteomics, metabolomics, epigenomics, and microbiomics. Several themes emerged:
- Inflammation control: Circulating markers suggested a low inflammatory set point relative to expectations for extreme old age. In the language of geroscience, the inflammaging curve looked flatter than expected.
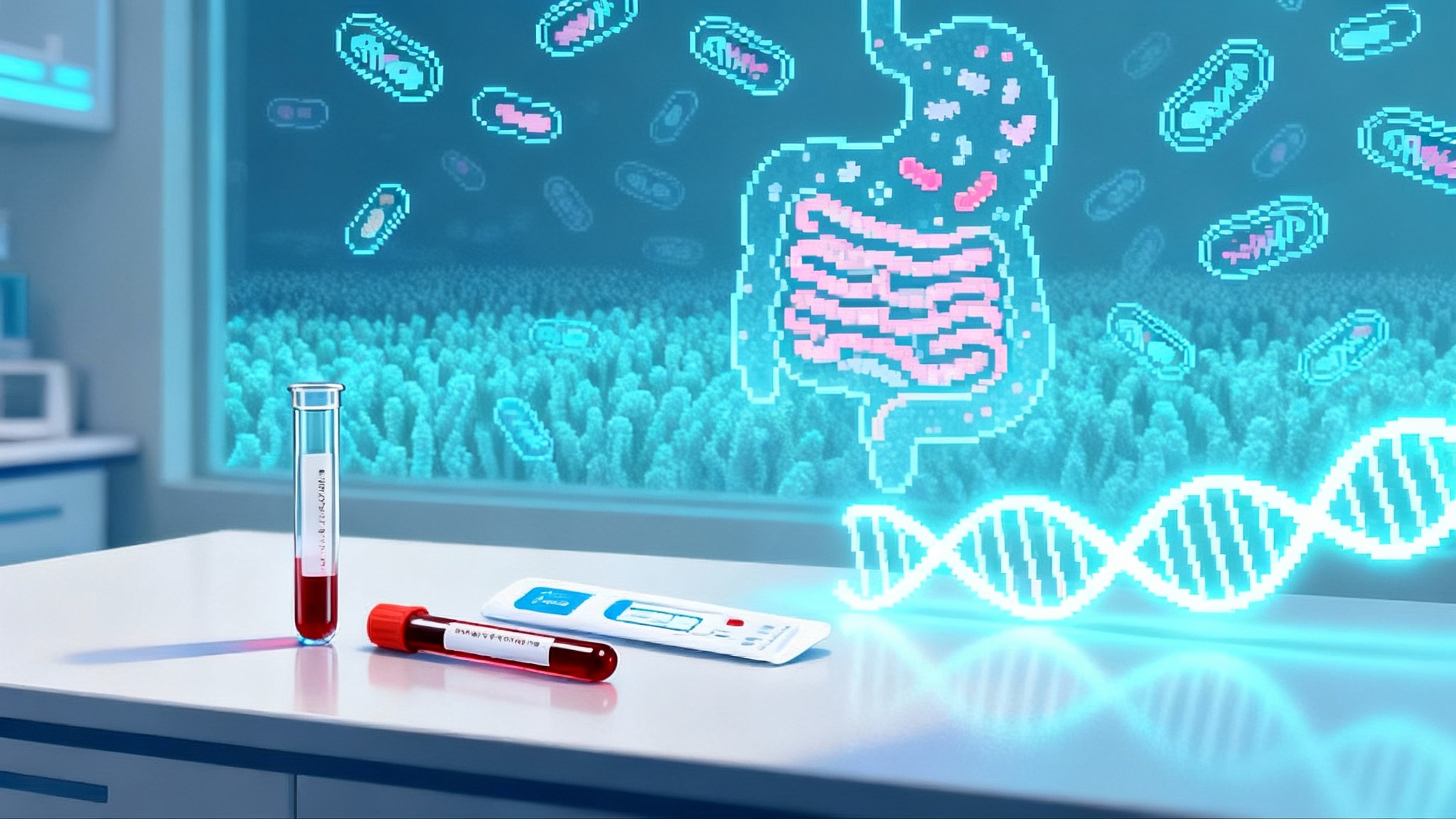
- Youthful microbiome features: Her gut community was enriched for health-associated taxa, including bifidobacteria that typically decline with age. This is the microbial signature you would expect in a younger gut.
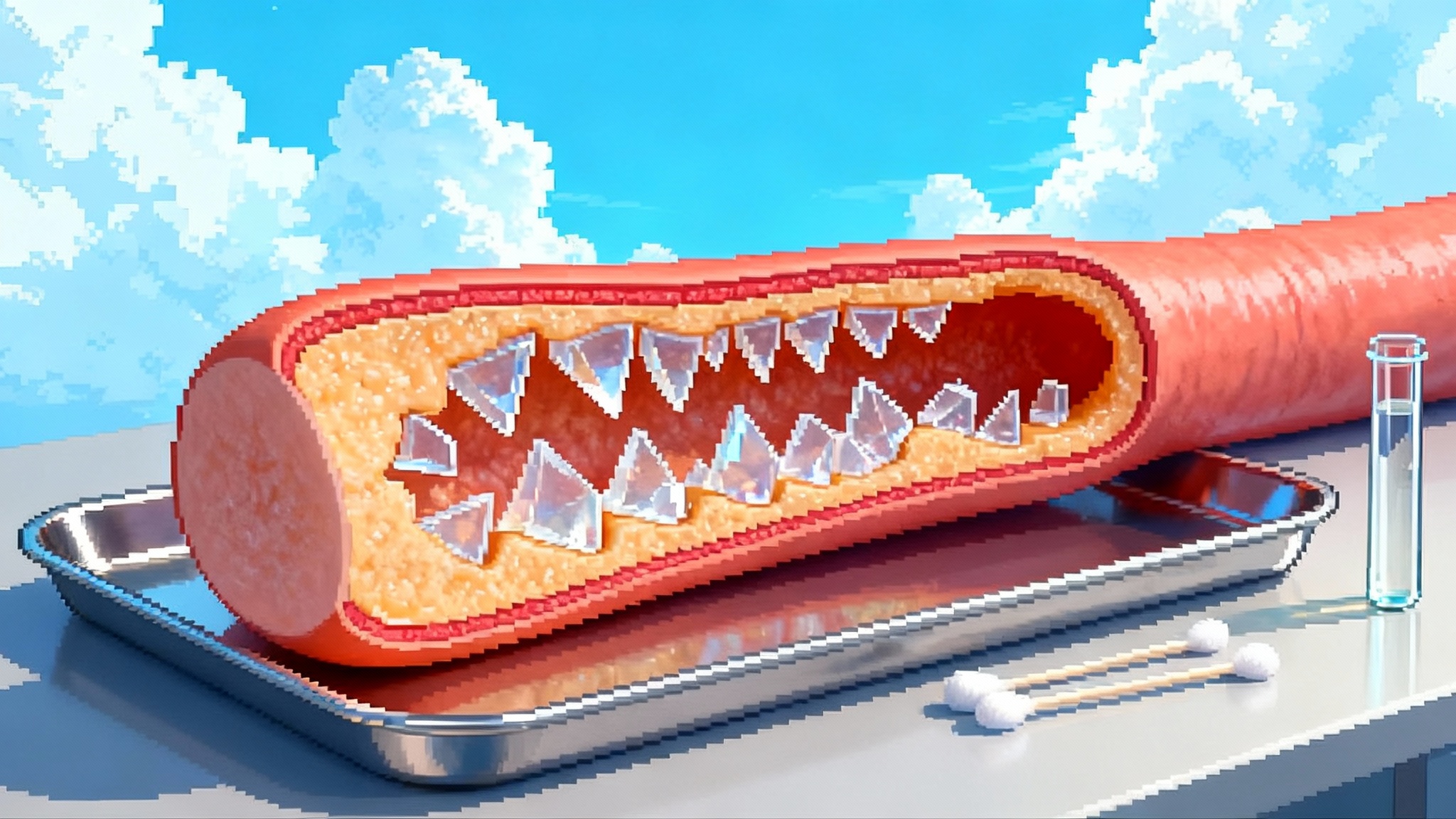
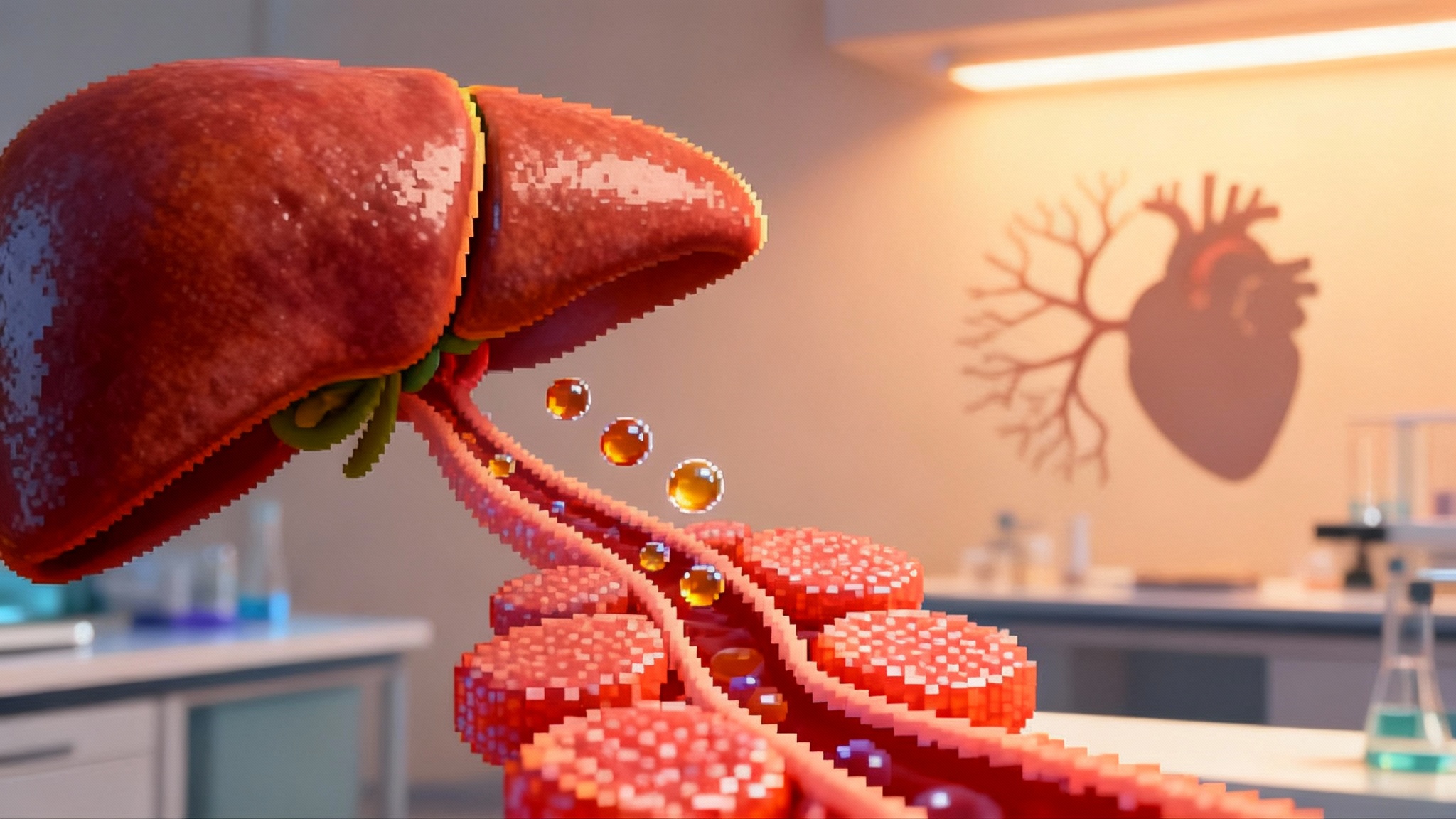
- Protective variants: Whole genome analysis identified rare variants associated with cardioprotection and neuroprotection, and a pattern of lipid handling that matched healthy arteries and clean metabolic lines.
- Younger epigenetic profile: Across multiple methylation clocks, biological age read younger than the birth certificate, in some tissues by a decade or more.
- Mitochondrial function: Measures pointed to efficient mitochondrial housekeeping and low oxidative burden, the sort of energetic poise that keeps cells responsive rather than fragile.
Taken together, the signals push us to ask a different question. Rather than asking how to slow the clock, we can ask how to harden the circuits that keep physiology stable as time passes. Resilience may be a better target than aging rate per se.
From signals to systems: what resilience looks like
The case points to four resilience domains that can be translated into research programs and, eventually, interventions.
1) Inflammation set point and immune competence
Healthy aging requires two things at once. The immune system must be calm at baseline, yet ready to mount rapid, proportionate responses to threats. The Branyas profile fits that pattern. Markers of chronic inflammation were low, yet evidence of robust immunologic memory remained. This balanced state reduces the constant tissue wear and tear that feeds cardiovascular disease, type 2 diabetes, and frailty, while preserving the ability to fight infection and surveil for cancer. For potential levers, see emerging work on thymus rejuvenation strategies.
2) Microbiome symbiosis and barrier integrity
A microbiome rich in bifidobacteria and other cooperative taxa supports short-chain fatty acid production, maintains gut barrier function, and feeds back on systemic inflammation. It can also influence lipid metabolism and aspects of cognition through microbial metabolites. A youthful gut community is not cosmetic; it is a metabolic and immunologic organ that shapes the host’s aging trajectory.
3) Mitochondrial housekeeping and redox control
Energy production and damage control live side by side in mitochondria. Efficient mitophagy, robust electron transport, and restrained reactive oxygen species keep cells adaptive under stress. The case’s signals of mitochondrial efficiency point toward a resilience axis that integrates with both inflammation control and epigenetic stability.
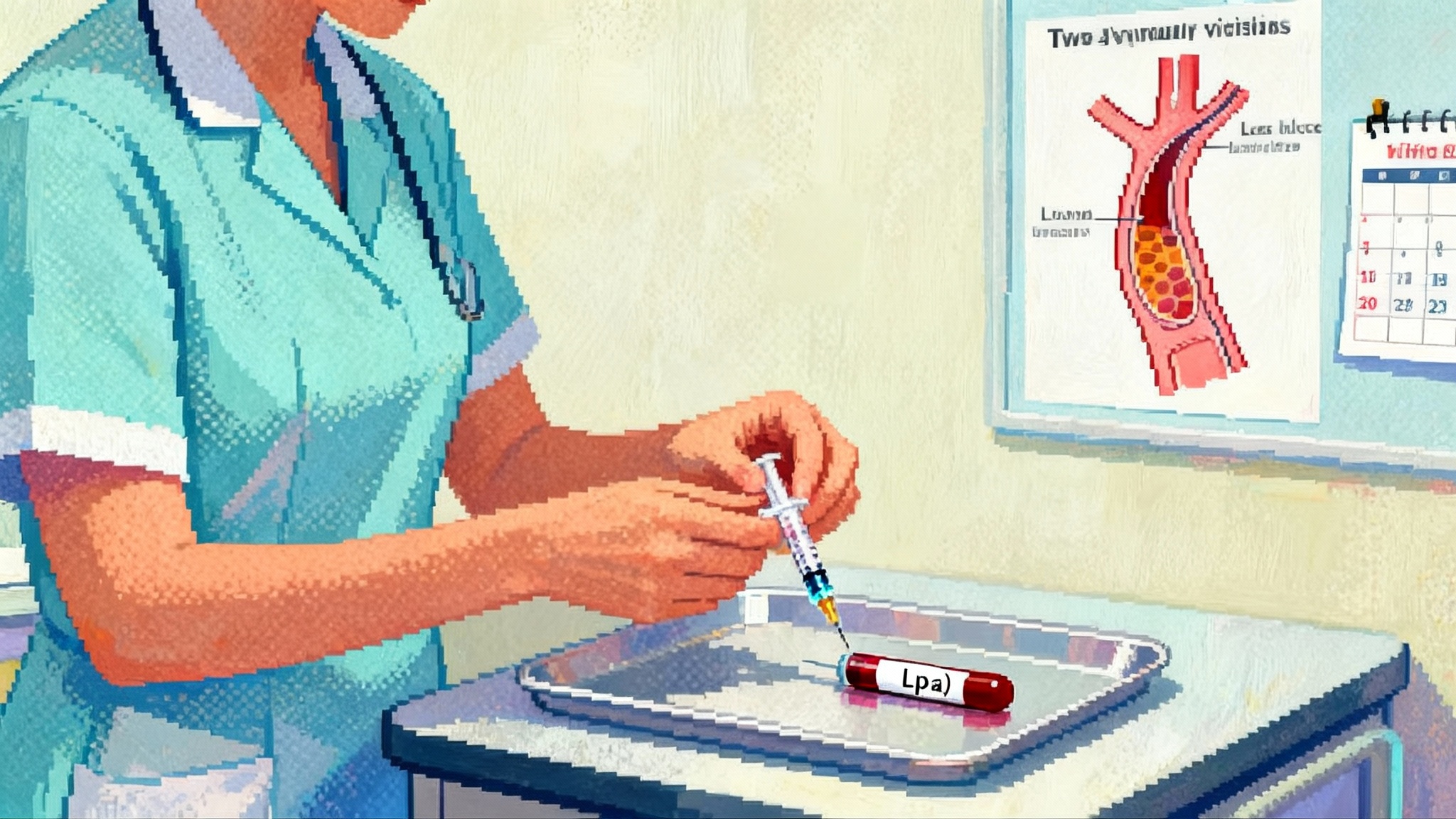
4) Genetic buffers and lipid handling
Protective variants are not a treatment, but they point to druggable pathways. Variants that favor healthier lipid profiles, improved neuronal resilience, or reduced pro-inflammatory signaling converge on lower late-life disease risk. These pathways can be targeted with medicines, diet, or microbiome engineering. For example, see our Lp(a) RNA therapies overview.
What this means for next-wave interventions
Resilience cannot be bottled in a single pill, but it can be engineered as a program. The signals above suggest several avenues:
- Tune the inflammatory thermostat: Combine lifestyle strategies that lower basal inflammation with targeted pharmacology for high-risk profiles. Diets rich in fiber and polyphenols, consistent physical activity, sleep regularity, and stress reduction remain the foundation. On top of that foundation, trials can test low-dose immune modulators that reduce chronic cytokine spill without blunting pathogen defense. Senescent cell clearance, when safe and targeted, may also reduce sterile inflammation in older tissues. For context, see the St. Jude senolytics frailty trial.
- Rebuild a youthful microbiome: Fermented dairy and other fermented foods, soluble fibers, and resistant starches are classic bifidogenic inputs. Selective prebiotics that encourage bifidobacteria and butyrate producers belong in pragmatic trials that track systemic inflammation, lipid markers, and function. Probiotic strategies should move beyond generic blends toward strain-level precision, timed to host diet. Fecal microbiota transplantation in older adults remains experimental, so protocols should prioritize safety, donor screening, and defined microbial consortia over whole-stool transfers.
- Strengthen mitochondria as habit and target: Endurance and resistance training improve mitochondrial biogenesis and efficiency across the lifespan. Nutritional strategies that support mitochondrial cofactors and promote mitophagy can be layered in. Pharmacologic candidates that enhance mitochondrial quality control or modulate redox signaling should be tested with careful safety gates. The key is not chasing a single antioxidant; it is restoring turnover and energy flexibility.
- Mimic protective genetics with pathway-guided therapies: If rare variants point to pathways that keep arteries clear and neurons resilient, go after those pathways. Lipid-lowering agents that reduce atherogenic particles, drugs that stabilize microglial tone, and small molecules that modulate stress response pathways should be tested not only for disease endpoints, but also for resilience outcomes such as preserved gait speed after a stressor, quicker recovery from infections, and maintenance of everyday function.
- Align epigenetic age with function: Epigenetic clocks are best used as composite biomarkers in trials rather than consumer trophies. The goal is not to shave points off a clock in isolation. The goal is to move the whole system toward lower inflammation, better energy management, and preserved function, then see epigenetic age fall in parallel.
Rethinking trial design around resilience
If resilience is the target, trials must move beyond static snapshots:
- Enrich the right participants: Instead of enrolling only by chronological age, stratify by inflammation, microbiome composition, and mitochondrial health at baseline. For example, a cohort with elevated IL-6, low bifidobacteria, and impaired PBMC mitochondrial respiration is more likely to show a response to anti-inflammatory, microbiome, or mitochondrial interventions.
- Use dynamic challenges to test stability: Add standardized challenges that probe how the body responds and recovers. Vaccine responses, orthostatic blood pressure recovery, heart rate variability during controlled breathing, timed up and go after a mild exertion stimulus, and recovery of grip strength after a brief bout of fatigue all capture resilience better than resting values alone.
- Build multi-omics into the core: Collect stool, blood, and saliva at baseline and predefined intervals. Track inflammatory cytokines, lipid particles, metabolites such as short-chain fatty acids, and cell-free mitochondrial DNA. Run targeted methylation panels that reflect immune and metabolic aging, then prespecify how these markers map to primary outcomes.
- Choose endpoints that matter: Hospital-free days, infection recovery time, days of preserved independence, incident cardiovascular and cognitive events, and durable improvements in mobility are the anchors. Biomarkers should explain these outcomes, not replace them.
- Adopt factorial and adaptive designs: Many resilience levers interact. Trials that orthogonally combine microbiome support, exercise, and an anti-inflammatory can uncover synergy. Adaptive randomization can shift more participants toward arms that improve resilience early while preserving statistical power.
- Plan for diversity and generalizability: Recruit across age bands, sexes, ancestries, and socioeconomic contexts. Microbiomes, diets, and exposures vary widely. Resilience programs must work outside the clinic and outside affluent zip codes.
What larger cohorts should test next
No single case, no matter how exquisitely profiled, can rewrite the biology of aging. The next steps are clear:
- Validate microbial hallmarks: Do higher bifidobacteria, greater short-chain fatty acid output, and specific consortia correlate with lower inflammaging and better functional outcomes in community-dwelling adults over 85, and in centenarians and their offspring?
- Map protective genetics into pathways: Catalog rare and common variants that associate with healthy survival past 100. Focus on lipid handling, neuroinflammation, and mitochondrial maintenance. Use human induced pluripotent stem cell models and CRISPR perturbations to test whether variants drive measurable resilience in cardiomyocytes, neurons, and immune cells.
- Resolve telomere paradoxes with context: Short telomeres in this case coexisted with health. Larger cohorts should test whether telomere length is more of a timekeeper than a health meter at extreme age, and whether epigenetic and mitochondrial measures better predict function after 90.
- Quantify mitochondrial fitness in the wild: Move beyond proxies. Standardize assays of PBMC oxygen consumption, mitochondrial membrane potential, and mitophagy markers in large cohorts, then tie these to resilience outcomes and mortality.
- Track inflammation as a curve: Longitudinal cytokine panels can map the stability of an individual’s inflammatory set point. Add trigger events, such as vaccinations, to gauge the amplitude and decay of responses as people age.
- Build living biobanks with consent for multi-omics: High-quality, minimally invasive sampling at regular intervals, with explicit consent for post-mortem tissue donation when possible, will allow deeper tissue-level validation.
A candid word on limitations
This was a single individual, and an extraordinary one. Survivorship bias looms large. Sampling windows were limited to minimally invasive collections during life, and there was no post-mortem tissue analysis. Lifestyle, environment, and psychosocial context are difficult to quantify, yet likely contributed to the protective pattern. Even so, the case is not a curiosity. It is a practical blueprint that suggests what to measure, where to intervene, and how to judge success.
The practical takeaway for longevity science
Maria Branyas Morera’s biology suggests that healthy survival to extreme ages is not an accident. It is a negotiation between damage and defense, between time and the systems that ride it out. If we design interventions to lower the inflammatory set point, restore youthful microbiome functions, keep mitochondria in good working order, and mimic protective pathways revealed by genetics, then we may not need to slow time to add healthy years. We can teach the body to take a punch and bounce back.
That shift in mindset matters for patients and families. It moves the conversation away from exotic anti-aging promises and toward measurable gains, such as recovering faster from a winter virus, staying out of the hospital, or maintaining the strength to shop for groceries without help. The 117-year-old case does not end the story. It gives us a clear first chapter: build resilience, test it with real-world challenges, and measure the biology that makes it possible.