FDA LDT rollback: how longevity biomarkers return to clinics
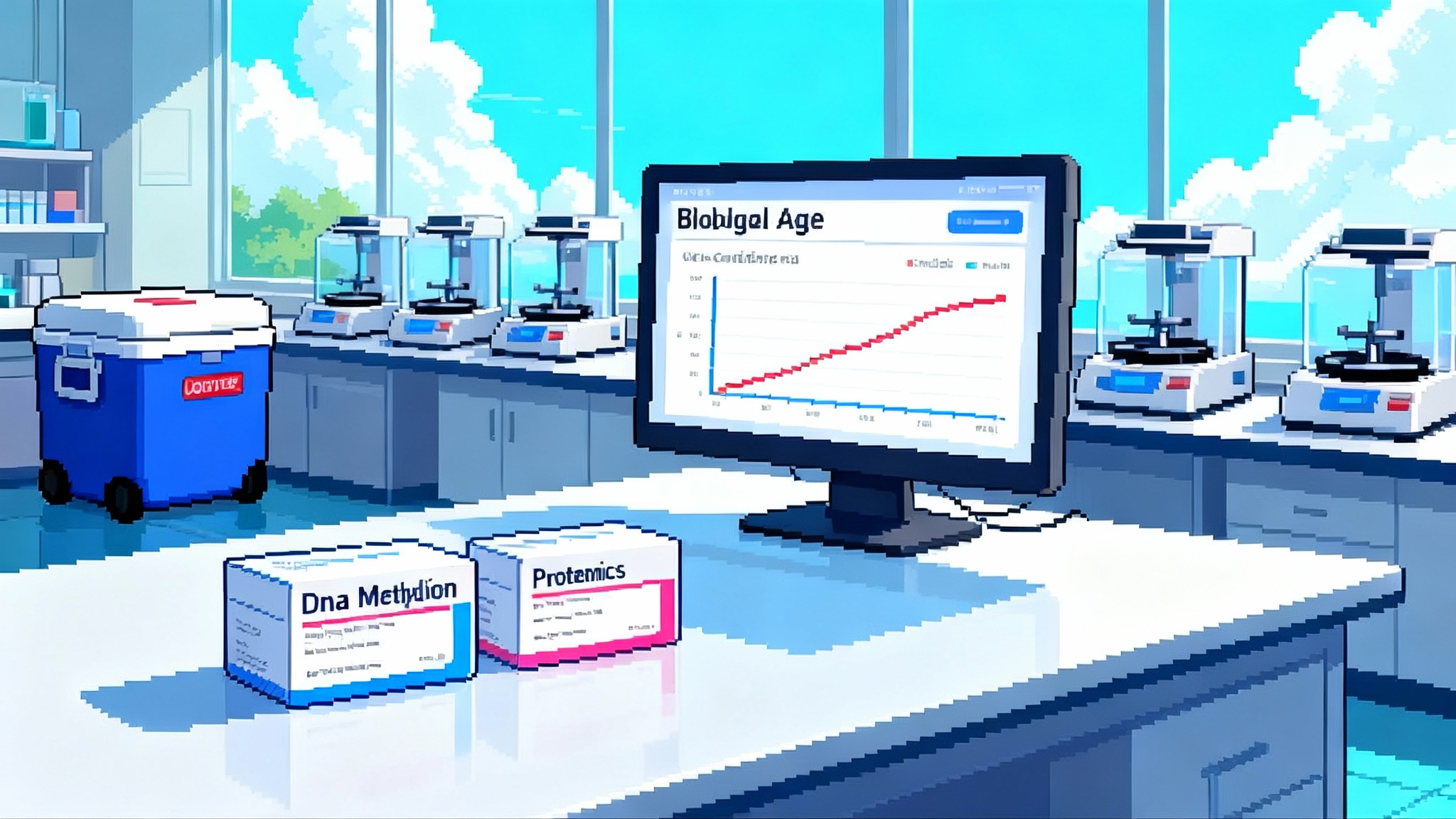
After a March 31, 2025 court ruling, FDA formally rescinded its 2024 LDT rule on September 19, 2025. Epigenetic clocks and proteomic biological age panels shift back under CLIA. Here is what is defensible now, how to validate, and what to watch next.
The decision that reset the longevity biomarker market
On September 19, 2025, the Food and Drug Administration formally rescinded its 2024 rule that would have brought most laboratory developed tests into the medical device framework. The agency acted after a March 31, 2025 federal court decision vacated the rule in its entirety. Reuters reported the planned rollback the day prior, with the agency restoring its prior enforcement discretion posture and returning LDTs to the CLIA regime. See the Reuters coverage of the FDA rollback and timing.
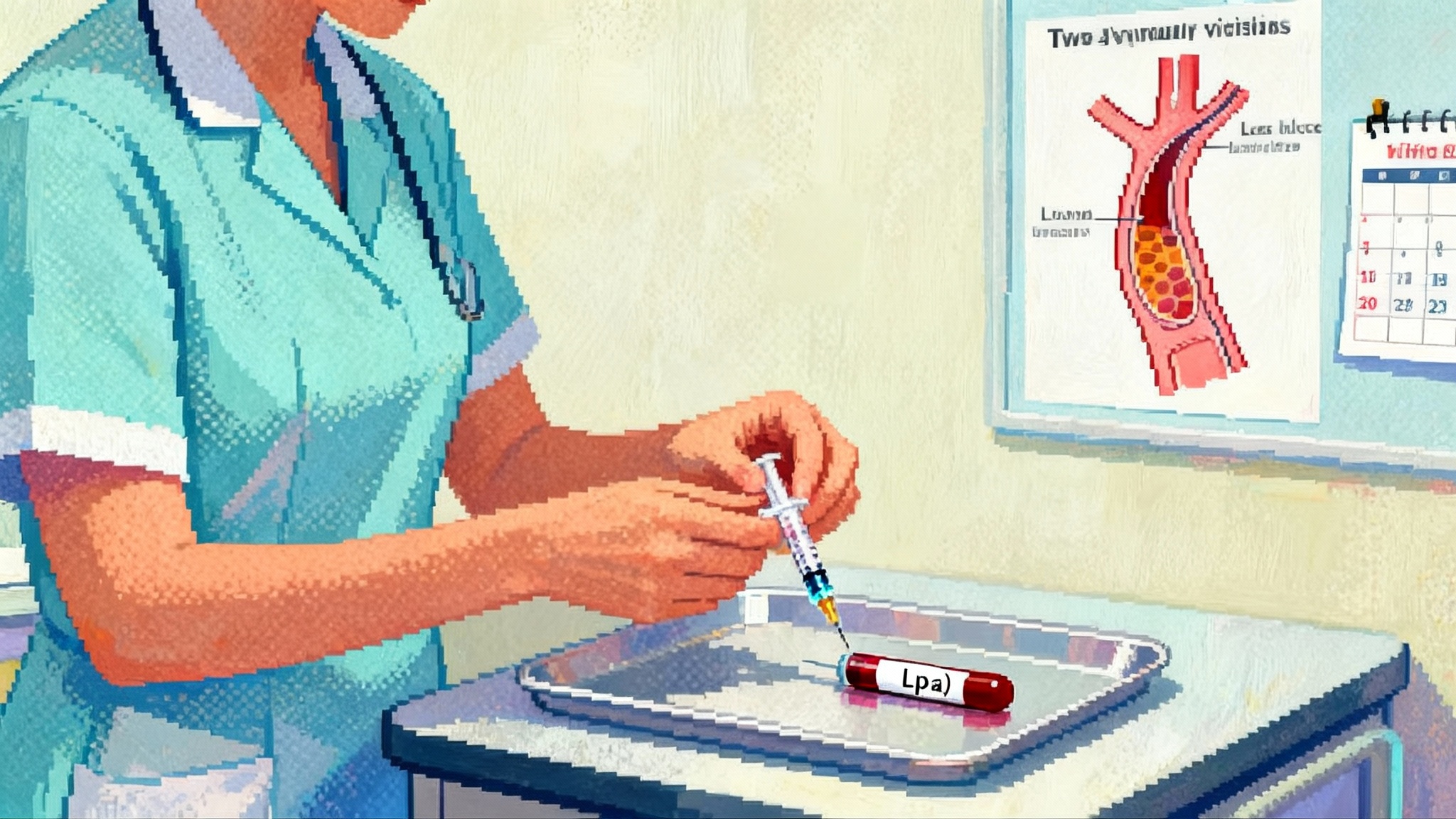
For longevity medicine, the result is operational clarity. If you order biological age testing, you will again evaluate vendors on CLIA credentials, analytical validation packages, and transparent methods, not device submissions. This is not a free pass. CLIA still requires laboratories to establish performance specifications before clinical use, and medical boards and payers will hold clinicians to standards of care when interpreting results. For related diagnostics entering routine care, see our look at pTau217 blood tests arrive and how lipid genetics is shifting treatment with RNA shots reset heart risk.
What changed, and what did not
What changed
- FDA’s 2024 final rule is rescinded, so staged device compliance deadlines are off the table.
- Labs can continue to develop, validate, and market LDTs to clinicians under CLIA and relevant state programs.
- The immediate compliance burden for longevity biomarker vendors shifts back to CLIA method validation, proficiency testing where available, and postanalytic quality controls.
What did not change
- CLIA requires documentation of accuracy, precision, analytical sensitivity and specificity, reportable range, and reference intervals before clinical release.
- State oversight still matters, including New York State’s Clinical Laboratory Evaluation Program and state medical practice rules on ordering and use.
- Payers will continue to scrutinize medical necessity, and courts will expect prudent interpretation with informed consent.
Which biological age assays are scientifically defensible now
Not all biological age tests are created equal. When selecting or offering assays, anchor on three pillars: predictive validity for hard outcomes, test–retest reliability within individuals, and responsiveness to clinically meaningful change.
Epigenetic clocks
- Mortality and morbidity prediction: Second generation methylation clocks trained to clinical phenotypes or mortality endpoints have the strongest evidence base. These tools often stratify risk for cardiovascular events, incident cancer, and all-cause mortality beyond age and basic risk factors.
- Pace of aging measures: Pace scores that estimate physiologic change per unit time can be more sensitive to short term interventions than static age gaps and often show higher short term repeatability.
- Platform matters: DNA methylation data quality depends on the assay and array. Illumina EPIC array versions are not interchangeable with older arrays without careful normalization and probe selection. Cross reactive probes, batch effects, and bisulfite conversion efficiency can bias results. Labs should publish probe sets, normalization pipelines, and batch correction strategy.
- Preanalytic stability: Whole blood methylation profiles are generally robust to shipping when stabilized, but delays, temperature excursions, and hemolysis can shift certain loci. Choose vendors with controlled logistics and document chain of custody.
Proteomic biological age panels
- Signal versus noise: Proteomic clocks trained on hundreds to thousands of proteins capture inflammatory tone, cardiovascular risk, and metabolic stress. They can predict disease and mortality risk in population cohorts, yet are susceptible to acute illness, hydration status, and fasting state. Excellent within person precision is possible, but interpret results in clinical context.
- Platform stability: Aptamer based and proximity extension assays have different dynamic ranges and susceptibility to matrix effects. Lot to lot variability, drift, and calibration require monitoring with reference materials. For longitudinal care, prefer vendors that lock assay chemistry and document version changes in the report. For cardiometabolic context, see our coverage of GLP-1 muscle-sparing therapies.
Other modalities
- Glycomics: IgG glycan derived age scores correlate with inflammation and cardiometabolic risk. Evidence is promising for population risk stratification, with moderate repeatability. Preanalytic handling and lab specific pipelines remain important.
- Metabolomics and lipidomics: These capture lifestyle and metabolic status. Today they function best as risk signatures rather than precise biological age meters and need careful normalization across batches.
- Telomere length: Leukocyte telomere length shows high biological and technical variability and weak short term responsiveness. It is generally not suitable as a standalone marker for individual clinical decisions.
Bottom line on scientific defensibility: favor assays with published cohort level validity against hard outcomes, documented analytical validation on the exact platform used, and transparent versioning. Be wary of proprietary indexes that provide a single age number without an uncertainty estimate.
How to validate and report responsibly under CLIA
Analytical validation checklist for aging assays
- Precision and reproducibility: Demonstrate within run and between run coefficients of variation on clinical samples across the measurement range. For multiomics panels, include repeat extractions and dual technicians to capture total process variability.
- Accuracy and method comparison: Use orthogonal methods where feasible, or compare to a well characterized reference cohort and published benchmarks. For proteomics, include reference standards and spike recovery experiments. For methylation, use control DNA and interlaboratory comparisons when possible.
- Limit of detection and quantitation: For panels that include low abundance proteins or metabolites, establish LoD and LoQ, and define how values below thresholds are handled.
- Reportable range and linearity: Confirm linear response in the range that drives the composite score. Nonlinear regions can distort index values if not modeled.
- Interferences and matrix effects: Evaluate hemolysis, lipemia, bilirubin, and common medications that might alter measured signals or aptamer binding. Document assay specific interferences in the report.
- Stability and shipping: Validate stability across realistic shipping times and temperatures with the actual collection kit. Include freeze thaw robustness if specimens may be stored for retesting.
- Bioinformatics and version control: Treat the computational layer as part of the test. Lock code commits, maintain audit trails, and version the model and normalization steps. If you update the algorithm, include the version change in patient reports and provide a crosswalk for longitudinal results.
Clinical reporting principles
- Present both the composite score and an uncertainty interval or repeatability estimate. If the standard error of measurement is two years, a reported five year change in three months is likely noise.
- Contextualize the number. Provide population centiles by age and sex and the degree to which the score predicts outcomes after adjusting for risk factors. Avoid implying diagnostic status.
- Show component domains where available, for example cardiometabolic, inflammatory, and pulmonary components of a proteomic panel. This helps clinicians map results to interventions.
- Disclose preanalytic flags. If a sample arrived warm or was processed late, note this in the report and caution interpretation.
- Version transparency. Clearly list assay chemistry version, array version, and algorithm version. State any material changes since the prior test.
Documentation to keep on file
- CLIA validation summary with study design, sample numbers, statistical methods, and acceptance criteria.
- Standard operating procedures for collection, processing, analysis, and reporting.
- Proficiency testing or alternative assessment results where formal PT is unavailable. Use split sample exchanges or blinded repeats.
- Adverse result investigation logs, including root cause analysis for outliers.
Payers, coding, and liability
Coverage and coding
- Many payers classify biological age testing as investigational for routine care. Expect limited coverage outside of trials, structured care pathways, or narrow medical necessity indications.
- Use appropriate CPT codes. Some panels have unique PLA codes, others rely on molecular pathology unlisted codes. Expect payer requests for documentation of analytical validity and clinical utility.
- Medicare contractor policies differ. If your patients are Medicare beneficiaries, check your MAC’s local coverage decisions and consider Z code registration where applicable. Preauthorization may be required by commercial plans.
- Pricing strategy: Be transparent with cash pricing, and do not bundle testing with multi year subscription models that obscure per test cost.
Liability and scope of practice
- Biological age reports influence lifestyle counseling and may influence therapy choices, for example lipid lowering or sleep apnea evaluation. Document that these tests inform risk stratification and behavior change, not diagnosis of disease.
- Use shared decision making. Obtain consent that explains uncertainties, potential for false improvement or deterioration, and the possibility of incidental findings if omics panels reveal unexpected data.
- Avoid deterministic language. Replace definitive phrasing with probabilistic framing and clear confidence intervals.
- Do not use a biological age score alone to start, stop, or intensify prescription therapies that otherwise require guideline based indications. Corroborate with standard clinical tests.
Risks of overreach and direct to consumer hype
Expect a marketing surge. Counter with discipline.
- Beware of single number syndrome. Biological age simplifies complex biology. Show component signals and the uncertainty, and resist turning it into a personal scoreboard.
- Respect regression to the mean. A high result often improves on retest even without intervention. Use baselines with two draws when feasible before making claims about change.
- Standardize preanalytics. Fasting status, timing, and recent illness can move proteomic and metabolomic scores. Set rules, for example morning draws after a rest day and a symptom free week.
- Guard against novelty bias. New algorithms may look better on training data than on your patients. Insist on external validation in diverse cohorts.
- For direct to consumer offerings, require physician oversight for interpretation and clear escalation pathways when results are concerning.
A practical roadmap for clinics and startups
Phase 1, next 90 days
- Vendor due diligence: Request CLIA validation documents, precision studies, and algorithm version histories. Verify CLIA certificate type and any state approvals.
- Pilot workflow: Run a small internal pilot with staff volunteers to test logistics, turnaround time, and report clarity. Confirm that EHR integration does not misclassify the result as a diagnostic finding.
- Consent and reporting templates: Build consent language that explains purpose, limits, and data use. Create a one page addendum that translates the report into concrete lifestyle and follow up steps.
Phase 2, next 6 months
- Standard operating procedures: Lock preanalytic instructions, including fasting, activity, and illness windows. Train phlebotomy staff and coaches.
- Quality monitoring: Use blinded duplicates at a low frequency to monitor drift. Track lot numbers and algorithm versions alongside patient results.
- Outcome tracking: Define a minimal clinical dataset, for example blood pressure, atherosclerotic risk scores, HbA1c, waist circumference, and sleep measures, to correlate with biological age shifts.
- Equity and access: Offer financial assistance or sliding scale options. Ensure materials are readable and culturally competent.
Phase 3, trials and gerotherapeutics
- Fit for purpose endpoints: If you plan a gerotherapeutic trial, specify whether the biomarker is a primary mechanistic endpoint, a secondary outcome, or an exploratory signal. Align sample size with the assay’s standard error and expected effect size.
- Multiplicity controls: If you run multiple clocks, prespecify the hierarchy and the primary analysis. Avoid unblinded selection of the most improved index.
- Replication plan: Commit to confirmatory measurement in an independent lab for pivotal claims, especially if the trial aims to support payer coverage or guideline recommendations.
- Data governance: Protect raw omics data and derived scores with consent that covers secondary research use. Be explicit about data sharing and algorithm updates during the study.
What to watch next
Congressional action
The court ruling created a regulatory vacuum that Congress may choose to fill. Prior legislative proposals attempted to create a unified framework for in vitro clinical tests. If new legislation gains traction, it could reintroduce a premarket pathway for higher risk LDTs, create risk based tiers, or formalize data registries. Vendors should stay close to trade associations and be prepared to submit data on clinical validity and real world performance if lawmakers solicit input.
FDA biomarker qualification
Independently of LDT oversight, FDA’s drug centers continue to run the Biomarker Qualification Program. For developers who want biological age to influence drug development decisions, define a narrow context of use and work through qualification or seek a Letter of Support. Qualification applies to the biomarker and its context, not to a specific clinical test device. See the FDA’s Biomarker Qualification Program for stages, contexts of use, and transparency on qualified tools.
Signals to look for over the next year
- Federal Register notices or guidance that clarify rescission implementation details, especially how FDA will handle novel high risk diagnostics if safety concerns arise.
- New payer policies referencing biological age testing. Some plans may pilot coverage when tests are embedded in proven care pathways.
- Publication of interventional studies showing biomarker changes tracking with improvements in hard outcomes, for example fewer hospitalizations or improved VO2max.
- Emergence of multicenter proficiency programs for omics based aging assays, building trust through interlaboratory comparability.
Bottom line
FDA’s rescission resets the longevity biomarker market to CLIA rules, not a free for all. Epigenetic clocks that predict morbidity and mortality and proteomic panels with clear validation are reasonable to use today when paired with careful reporting, preanalytic discipline, and guarded clinical interpretation. Payers will demand evidence of utility in care pathways, and clinicians should present results with uncertainty, not certainty. Startups should double down on analytical rigor, longitudinal repeatability, and real world outcome tracking. If you aim to support drug development or reimbursement level claims, plan for fit for purpose studies and, where appropriate, biomarker qualification. The LDT rollback gives the field room to innovate and raises the bar for responsibility.