Mitochondria’s Moment: 2025 Turns Cellular Energy Into Care
Four milestones in 2025 moved mitochondria from metaphor to medicine: the first FDA approval for a mitochondria‑targeted drug, eight healthy births after mitochondrial donation, in vivo base editing in animals, and a fast‑tracked cell therapy for an aging disease.
The year cellular power became a clinical target
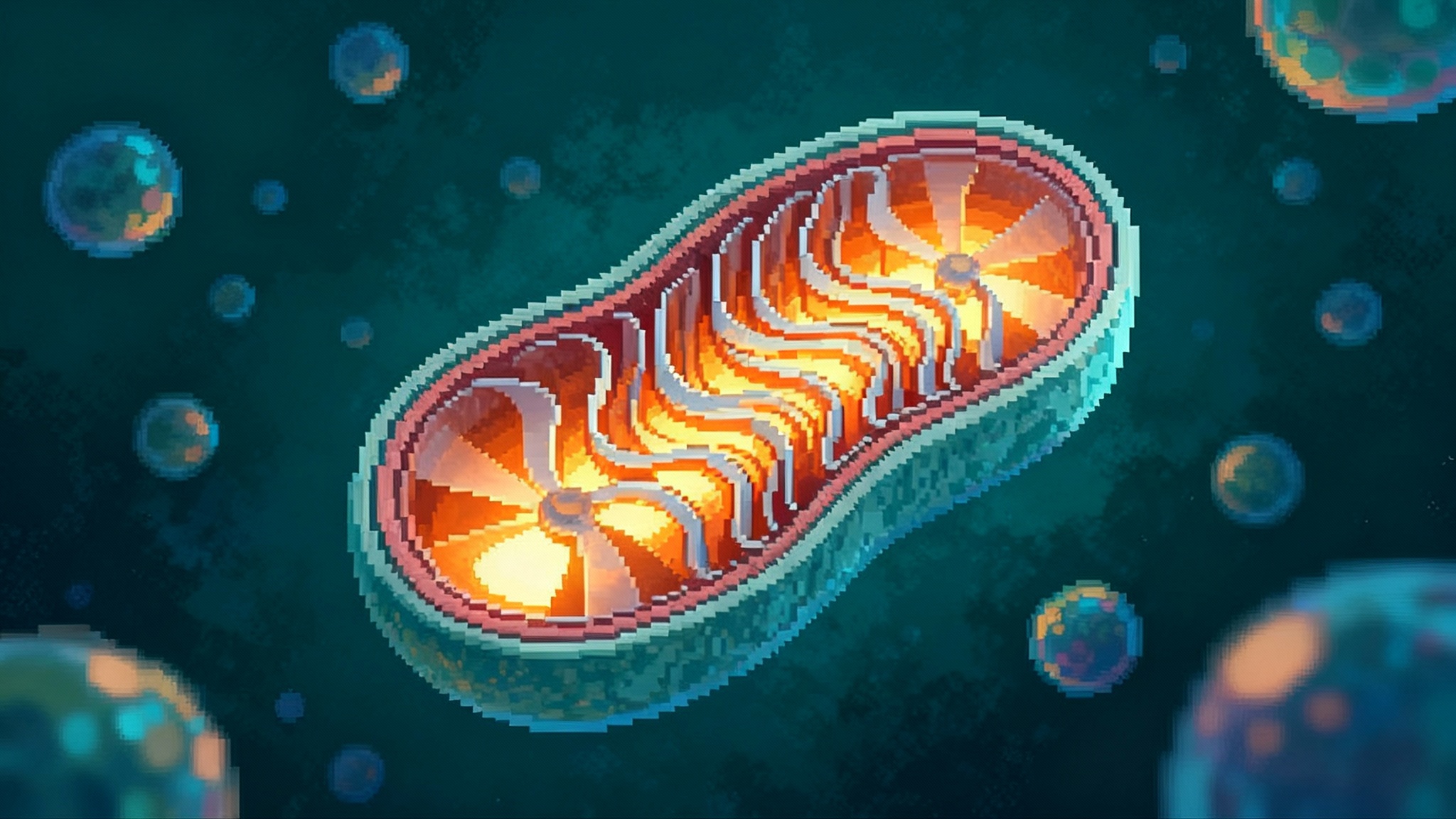
For a century, mitochondria were cast as biology’s power plants and little more. In 2025, they stepped onto the main stage of medicine. Four milestones reframed these organelles from background actors to modifiable levers for disease and aging:
- The United States Food and Drug Administration granted accelerated approval on September 19, 2025 to Forzinity, an elamipretide injection for Barth syndrome, the first approved therapy designed to improve mitochondrial structure and function. See the agency’s notice in the FDA grants accelerated approval.
- The New England Journal of Medicine reported eight healthy births after mitochondrial donation via pronuclear transfer, showing that a regulated pathway can block transmission of mitochondrial DNA disease. Review the NEJM clinical outcomes.
- Science Translational Medicine reported in vivo mitochondrial base editing in a mouse model, demonstrating feasibility while highlighting dose related off target edits that require better control.
- The FDA granted Fast Track designation to Minovia’s MNV‑201 mitochondrial augmentation therapy for myelodysplastic syndrome, pulling mitochondrial medicine toward mainstream diseases of aging.
Together, these events mark a crossing of the chasm. Mitochondria are no longer only a pathology seen in rare syndromes or a buzzword in wellness marketing. They are a therapeutic target with a regulatory pathway, a reproductive medicine decision tree, a genomic surgery challenge, and a cell therapy platform.
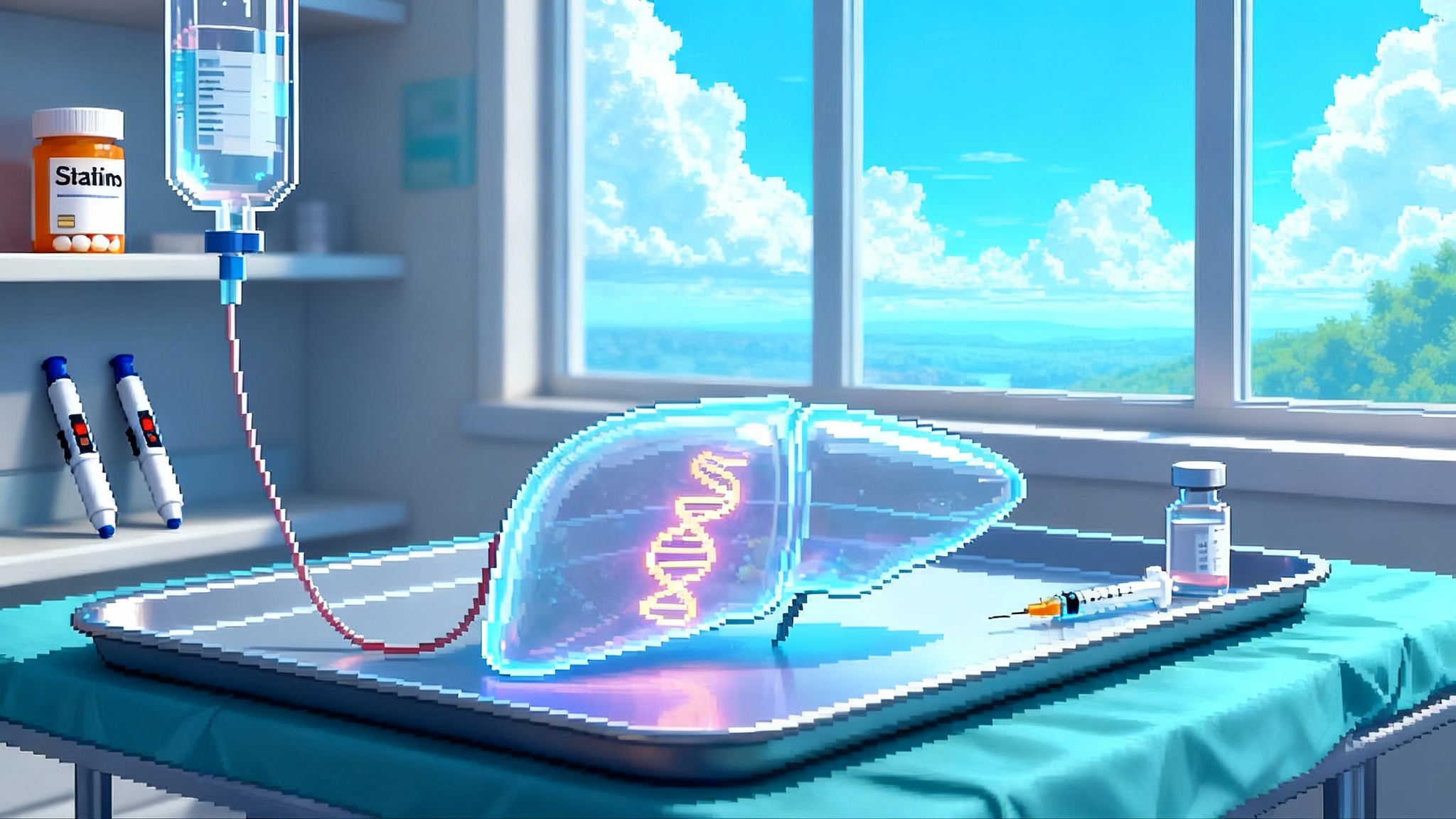
Milestone 1: An approval that validates mitochondria as an endpoint
Forzinity targets cardiolipin, a phospholipid that shapes the inner mitochondrial membrane into cristae, the ridges where the electron transport chain operates. In Barth syndrome, disrupted cardiolipin remodeling flattens those ridges and starves cells of adenosine triphosphate. Elamipretide binds and stabilizes cardiolipin, improving ultrastructure and electron transport efficiency.
The approval rested on an intermediate functional endpoint: improvement in knee extensor muscle strength that is reasonably likely to predict patient benefit. This matters because it shows regulators will accept a mitochondria‑proximal mechanism when downstream function is measurable and meaningful. It also gives trial designers a template for energy limited conditions where survival or hospitalization endpoints would take too long.
Practical takeaways:
- Pair mechanistic biomarkers of mitochondrial quality or output with patient relevant functional measures. For example, phosphocreatine recovery on phosphorus‑31 magnetic resonance spectroscopy alongside a 6 minute walk test or stair climb power.
- Plan confirmatory studies early. Accelerated approval creates urgency and scrutiny, so connect strength or endurance changes to daily function.
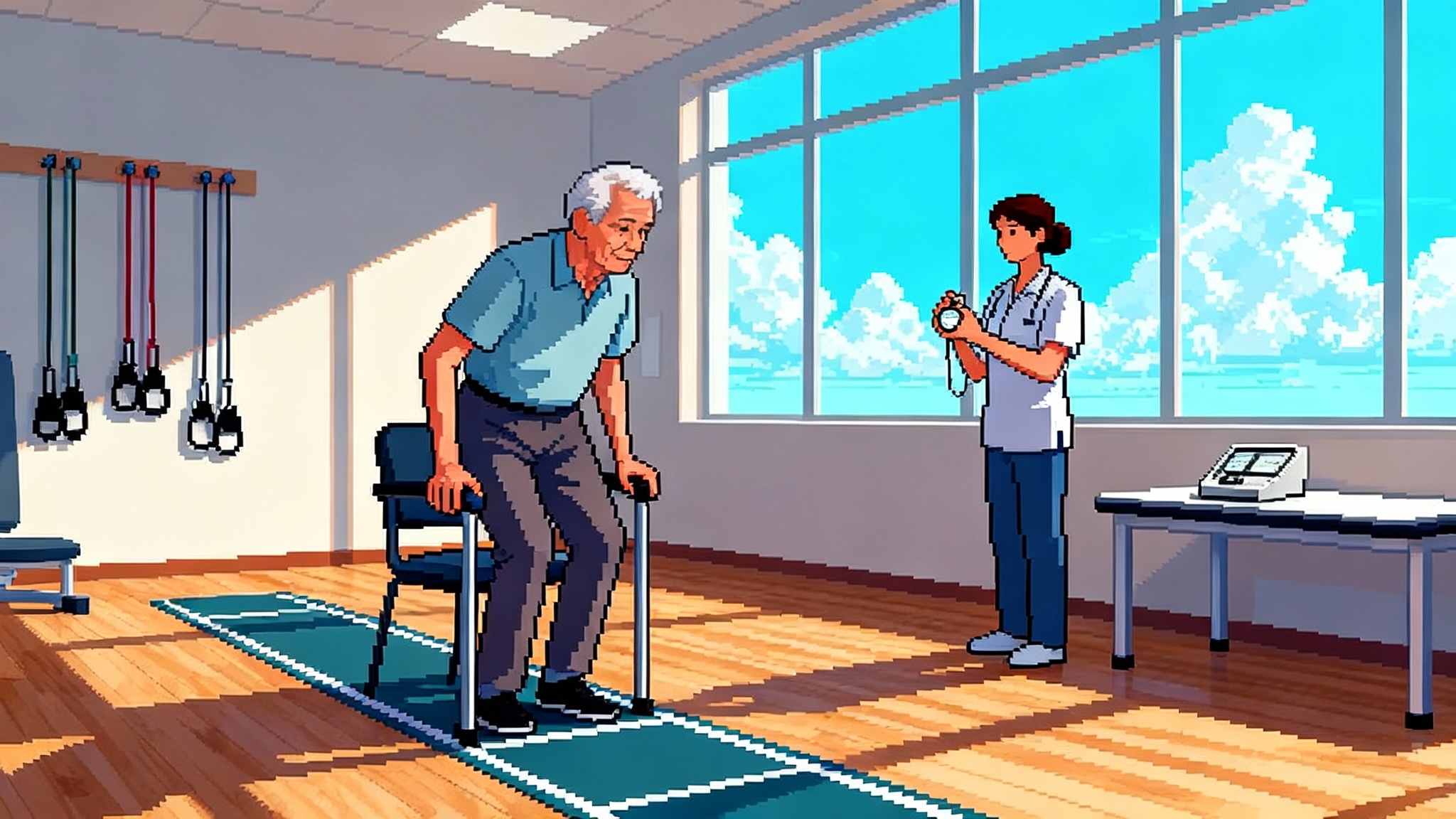
Milestone 2: Eight healthy births and a real clinical pathway
Germline mitochondrial disease is a generational trap. Mothers with high burdens of pathogenic mitochondrial DNA risk passing devastating disorders to children. In 2025, a Newcastle team reported that pronuclear transfer in an integrated pathway produced eight healthy births among twenty two women who could not benefit from preimplantation genetic testing alone. Heteroplasmy at birth ranged from undetectable to low teens, below disease thresholds at the time of reporting, with planned multiyear developmental follow up.
Policy realities in the United States:
- Congress continues to attach an appropriations rider that prevents the FDA from reviewing clinical applications involving heritable genetic modification, which blocks mitochondrial donation domestically.
- The Dickey‑Wicker amendment bars federal funding of embryo research, discouraging capacity building.
Why this matters for healthspan:
- Families at highest risk now have a credible, regulated alternative that can end a lineage of disease.
- The labs and quality systems built for pronuclear transfer will support future germline risk reduction tools.
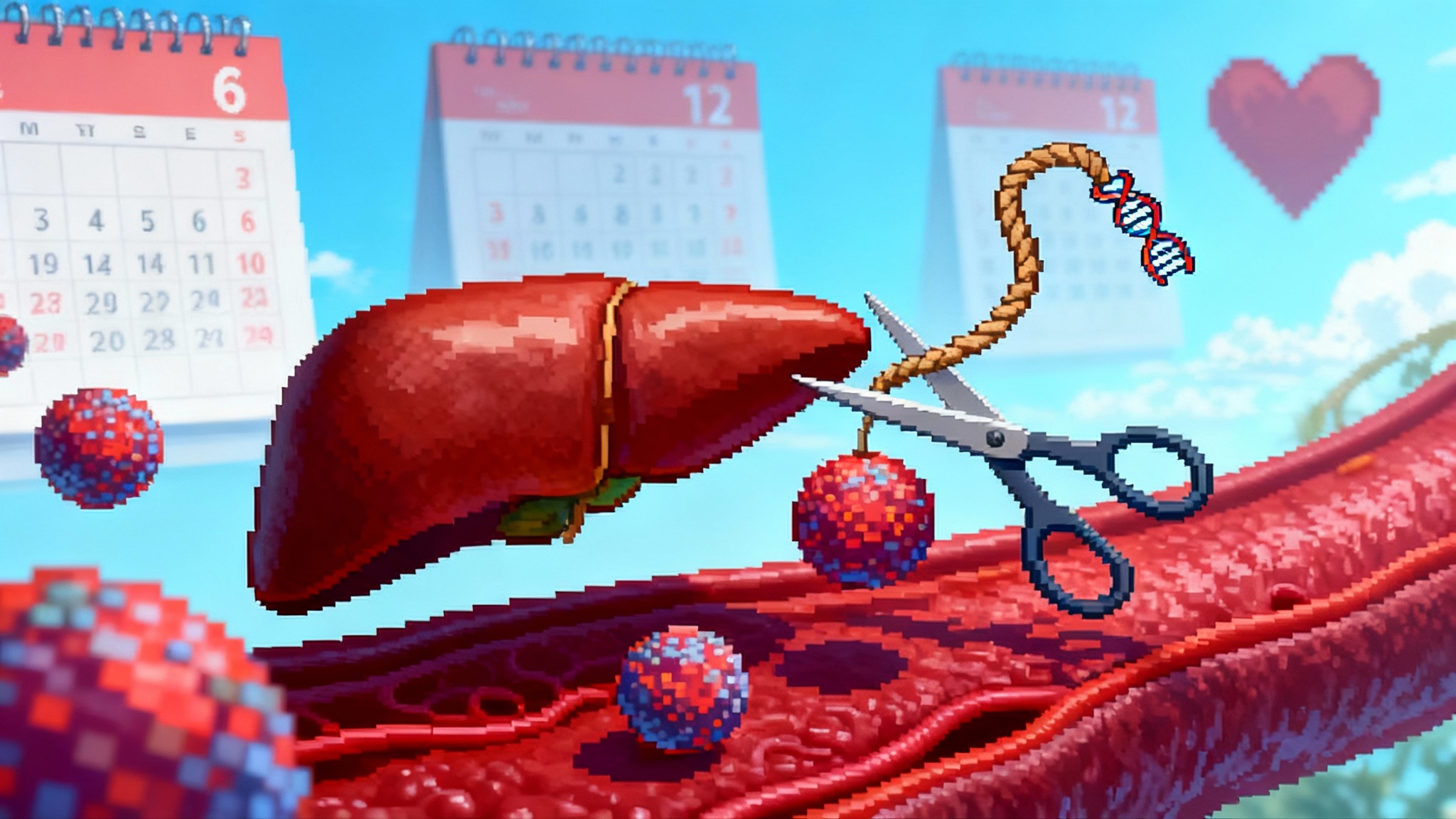
Milestone 3: In vivo mitochondrial base editing clears feasibility
A year ago, editing the small, multicopy mitochondrial genome in vivo faced a delivery stalemate. In 2025, researchers used mitochondrial DddA derived cytosine base editors to install a compensatory change in a mouse model of a transfer RNA mutation. The edit restored transfer RNA levels in heart and skeletal muscle and lowered elevated lactate. At the highest adeno associated virus dose, however, the editor triggered substantial off target mitochondrial edits, underscoring the need for tighter control of exposure in space and time.
What needs to happen next:
- Shift from viral DNA delivery to transient RNA delivery via lipid nanoparticles or hybrid systems that degrade after editing.
- Improve mitochondrial localization signals and import strategies to raise on target editing while lowering systemic exposure.
- Build assay panels that detect low frequency off target mitochondrial edits across tissues, not just in blood or the injected organ.
For broader editing context, see our coverage of base editing’s translation path in PCSK9 base editing leap.
Milestone 4: A fast tracked cell therapy targets an aging disease
Minovia’s mitochondrial augmentation therapy augments a patient’s hematopoietic stem cells with healthy mitochondria ex vivo, then reinfuses them. In September 2025, the FDA granted Fast Track designation for MNV‑201 in myelodysplastic syndrome, a common age related bone marrow failure.
Why this matters:
- It signals regulatory interest in mitochondrial biology for acquired, age related disorders, not only rare inherited syndromes.
- Fast Track enables more frequent agency interaction, rolling submissions, and potential priority review, accelerating iteration on endpoints and manufacturing.
Execution challenges to resolve:
- Standardize potency assays that predict benefit, such as mitochondrial membrane potential, adenosine triphosphate output per cell, mitophagy flux, and durability of organelle copy number after reinfusion.
- Scale sourcing and manufacturing while balancing autologous timelines against allogeneic immunogenicity tradeoffs.
- Track durability, since hematopoietic stem cells turn over and long term benefits will drive cost effectiveness.
Crossing the chasm: from rare disease to healthspan
Each milestone chips away at the wall separating rare disease work from healthspan impact.
- Regulatory validation: A mitochondria targeted mechanism with a functional endpoint can earn approval. That invites programs in heart failure with preserved ejection fraction, chemotherapy induced fatigue, sarcopenia, and post viral fatigue where energy handling is a bottleneck. For muscle centric implications, see our 2025 sarcopenia race analysis.
- Clinical maturity: A regulated reproductive pathway with documented outcomes creates precedent for careful, monitored use of germline risk reduction technologies.
- Technical feasibility: In vivo editing shows that repairing mitochondrial DNA is possible, with safety dependent on delivery and dose.
- Indication expansion: Fast Track in myelodysplastic syndrome places mitochondrial strategies in the diseases that burden healthcare systems.
A helpful metaphor is the city and its power grid. In rare mitochondrial disease, a neighborhood substation fails and homes go dark. In aging, the city keeps the lights on but runs brownouts at peak demand. 2025 showed we can repair a broken substation, add portable batteries to neighborhoods under strain, and upgrade the grid’s wiring.
The 12 to 24 month watchlist
Delivery, indications, and policy will determine whether mitochondrial medicine becomes standard care.
- Delivery that is safer and more precise
- Transient RNA and lipid nanoparticle systems for mitochondrial editors, with large animal readouts across heart, skeletal muscle, and liver. Success looks like high on target editing in a primary tissue with undetectable off target edits elsewhere.
- Tissue targeting without viral DNA using peptide ligands or charge tuned lipids to bias uptake to metabolically active tissues.
- Trials that move into common age related conditions
- Heart failure with preserved ejection fraction, defined by energetic inefficiency and impaired relaxation.
- Frailty and sarcopenia, where strength and endurance endpoints align with mitochondria targeted agents and functional labels. Related context in our 2025 sarcopenia race analysis.
- Neurodegeneration, where mitochondrial quality control and metabolic stress appear early.
- Policy debates that shape the reproductive pathway
- Appropriations riders that block FDA review of heritable embryo interventions may be renewed or reconsidered in the next budget cycles.
- Longitudinal registries for mitochondrial donation, including tissue specific heteroplasmy tracking and 3 to 5 year neurodevelopmental outcomes, will be prerequisites for any policy change.
- Measurement that regulators and payers can trust
- Imaging and spectroscopy, including phosphorus‑31 MRS recovery times, creatine kinase dynamics, and oxygen extraction fractions.
- Digital function composites that blend daily step counts, stair climb power, 6 minute walk distance, and patient reported fatigue. For how measurement is returning to clinic use, see aging clocks return to the clinic.
- Standardized mitochondrial panels, from membrane potential to mitophagy flux.
- Manufacturing and access
- Cell therapies will need potency, identity, and stability release criteria, plus closed system manufacturing to control cost.
- Small molecules must address drug drug interactions and chronic dosing safety in older, polypharmacy populations.
How different players should move now
- Biotech founders: Build a crisp causal chain. Show how your mechanism changes a mitochondrial parameter, how that parameter shifts a patient relevant function, and how your endpoint captures that change within 6 to 12 months.
- Clinicians: Standardize energy relevant measures in clinic. For heart failure with preserved ejection fraction, collect exercise capacity. In geriatrics, add grip strength and gait speed with a mitochondrial lens.
- Regulators: Encourage paired mechanistic and functional endpoints. Require off target mitochondrial editing panels for any in vivo editor. For germline interventions, insist on transparent registries and pre committed follow up milestones.
- Payers: Pilot outcomes based contracts tied to functional gains for mitochondria targeted therapies.
- Researchers: Treat delivery as the product. A transient, tissue selective editor or mitochondria seeking nanoparticle with clean histology unlocks entire indication classes.
The bottom line
In 2025, mitochondria became a set of knobs that medicine can turn. An approval put function on the label. Eight healthy births transformed a century old inheritance problem into a clinical pathway. Base editing in living animals made repair a question of delivery and dose. A fast tracked cell therapy pulled mitochondrial medicine into the diseases that fill hospitals and shorten lives. Over the next two years, safer RNA delivery, expansion into heart failure with preserved ejection fraction and frailty, and real policy debates over mitochondrial donation will decide whether cellular energy joins blood pressure and cholesterol as a routine target of care.