Inside 2025's Ovary Revolution: The Menopause-Delay Decade
Three 2025 breakthroughs reframed ovarian aging: a Science-level 3D map of the ovary as an ecosystem, a low-dose rapamycin pilot moving toward multicenter testing, and OHSU’s mitomeiosis milestone. The fastest healthspan gains may come from delaying menopause at the source.
A year that moved the goalposts
In 2025, the ovary stepped from backstage to center stage. Three headlines did the heavy lifting. First, researchers reframed ovarian aging as an ecosystem problem, not just an egg problem, with a study highlighted by UCSF that appeared in Science and mapped nerves, glia, fibroblasts, blood vessels, immune cells, and eggs interacting across time. That work recast menopause as a tissue choreography that can be measured and modulated, not a single clock that just runs down. See reporting on the Science study revealing the ovarian ecosystem.
Second, Columbia University’s VIBRANT pilot advanced an idea long tested in animals: use a low weekly dose of rapamycin to slow follicle activation and preserve ovarian reserve. The first cohort ran in midlife women with careful hormone and imaging readouts, and the team signaled plans for a larger multicenter follow-up. A small trial is not a cure. It is a bridge from basic biology to practice if the signals hold and safety stays clean.
Third, Oregon Health and Science University reported a proof of concept that used mitomeiosis to create functional human eggs from skin cell nuclei placed into donor oocytes. The embryos stopped early and chromosomal errors were common, but the method worked far enough to count as a genuine milestone. Read OHSU’s description of the mitomeiosis egg-creation breakthrough.
Put these together and you get a new thesis. If you want the biggest near-term gains in healthspan, do not start with the heart or the brain. Start with the ovary. It ages early and fast, it signals to the rest of the body, and we now have tools to track and test change within two to three years, not decades.
Why the ovary is the speed lane for healthspan
Every organ ages. The ovary just does it first and loudly. In most women, menopausal transition begins in the mid to late forties and completes near the early fifties. That transition is not only about fertility. As estrogen and other hormones fall, risks for cardiovascular disease, osteoporosis, metabolic syndrome, and neurocognitive change rise. Treating those downstream problems after menopause is like mopping up water while the tap is still open. The ovary is the tap.
Two biological levers explain why ovarian interventions might change healthspan faster than other approaches.
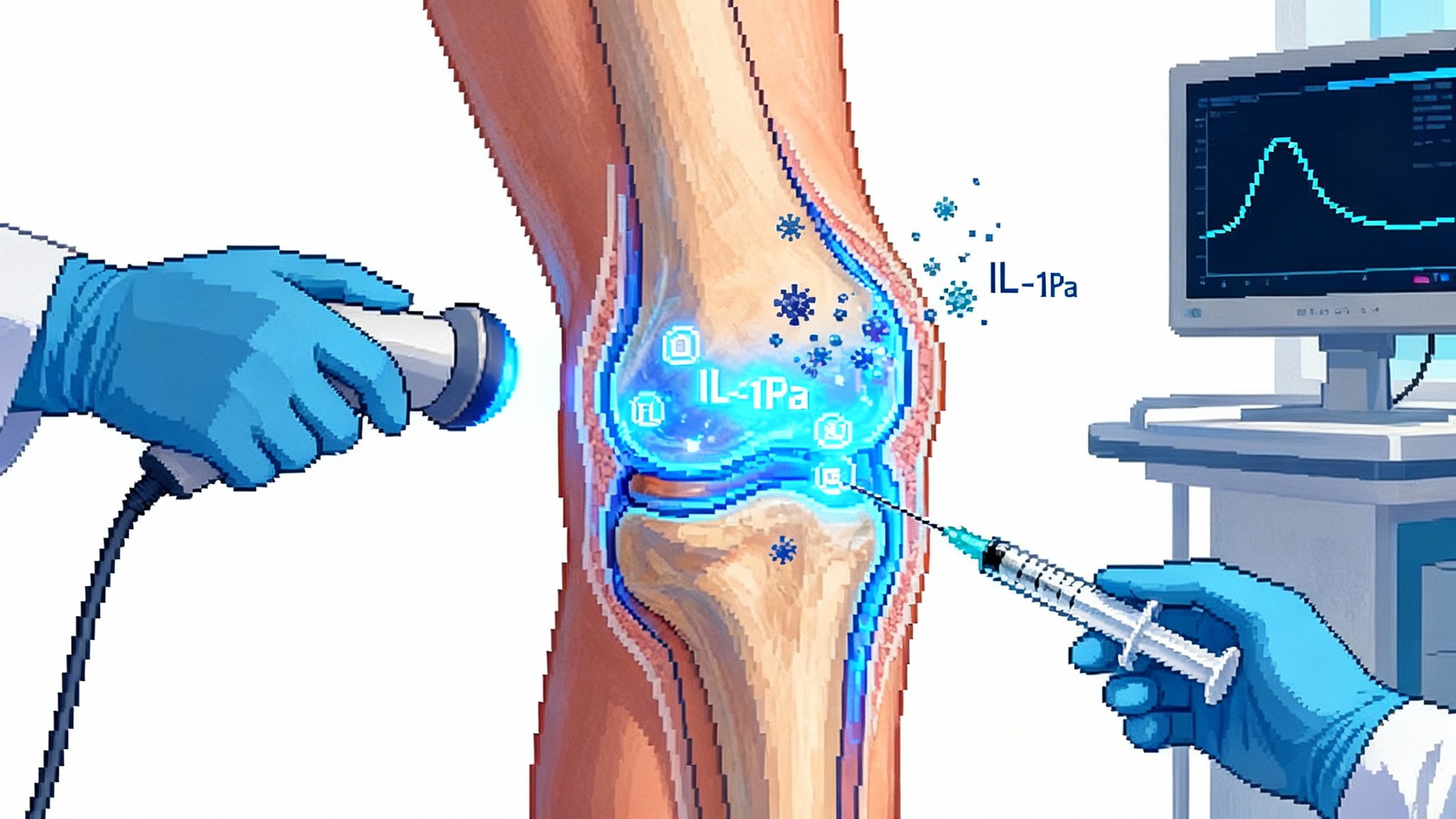
- The mTOR switch. The mechanistic target of rapamycin is a nutrient and growth sensor. When chronically high, mTOR pushes cells to grow and divide instead of maintaining themselves. In ovaries, high mTOR signaling accelerates the monthly activation of resting follicles. That depletes reserve sooner. Rapamycin turns the dial down. In animals, short courses preserve follicles, improve ovarian histology, and extend reproductive function. In people, the right dose and schedule must balance three goals at once: keep cycles regular, avoid contraceptive effects, and maintain immune safety.
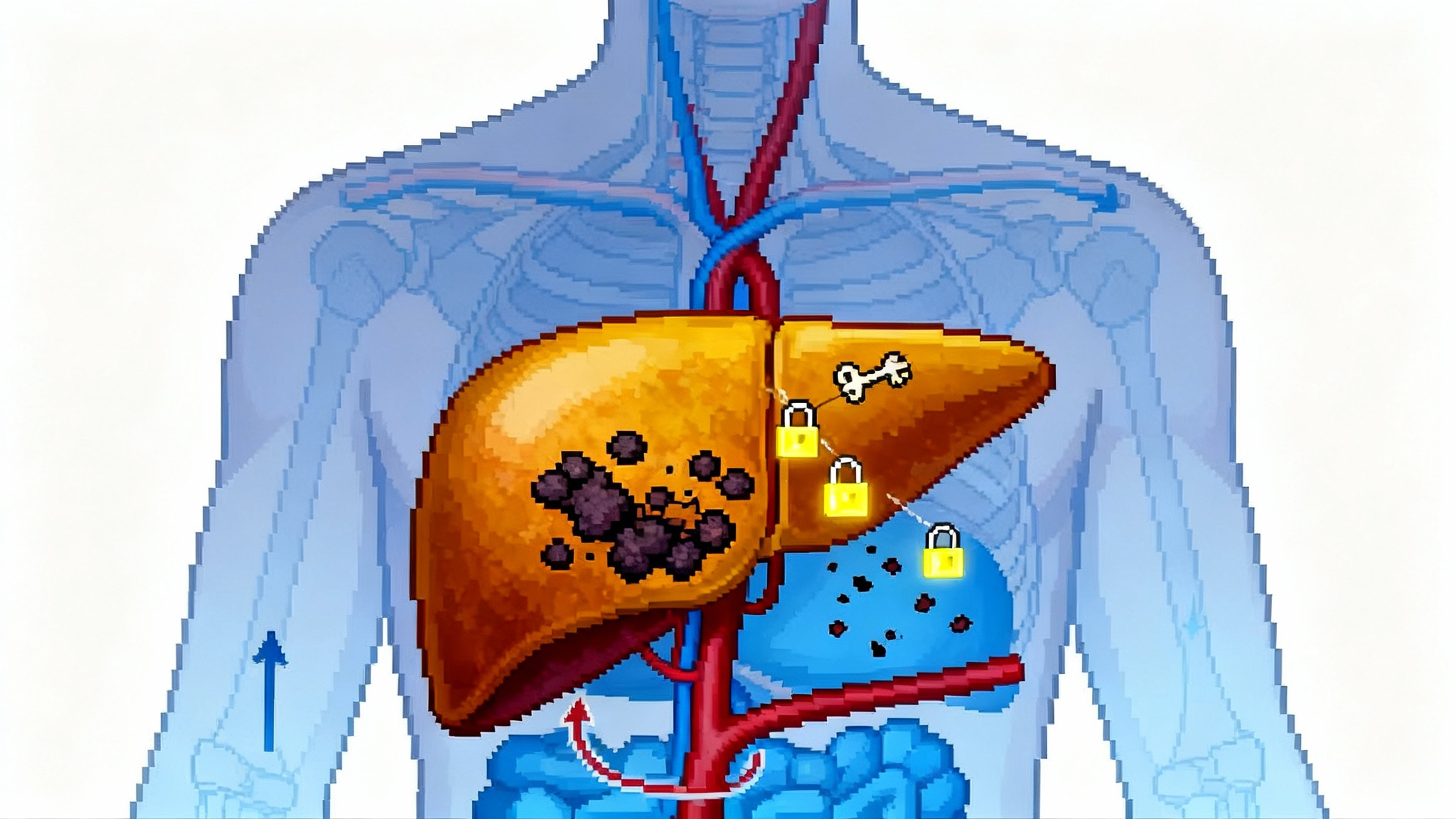
- The ecosystem drift. Ovarian tissue hardens and inflames with age. Fibroblasts become pro-fibrotic, collagen crosslinks accumulate, macrophages shift states and can fuse into giant cells, nerves remodel, and blood vessels and stromal cells change their signals to eggs. The 2025 Science reporting makes that visible in three dimensions. Eggs age, but they also live in a neighborhood that ages. If you soften the neighborhood, normalize immune tone, and rebalance the nerve signals that govern growth versus rest, then the eggs experience a friendlier, less stressful environment. That could preserve both quantity and quality. For a systems view of immune tone in midlife, see the 2025 race to reboot immunity.
The fastest near-term healthspan gains may flow from slowing this ecosystem drift before it hits the point of no return.
Rapamycin, clearly explained
Rapamycin is best known as an immunosuppressant for transplant patients at daily doses. At low weekly doses it hits mTORC1 enough to boost autophagy and ease the overactive growth signals that creep up with age, but without the deep immune suppression seen at transplant regimens. Ovaries are highly sensitive to mTOR. Think of mTOR like a thermostat for follicle activation. When the set point creeps up, too many follicles wake each month, and the reserve runs down faster. Dial the set point back a notch and you keep more follicles asleep without turning the system off.
A few concrete points that matter in the clinic:
- Dose and schedule matter more than the molecule itself. A weekly 5 milligram oral dose aimed at partial mTORC1 inhibition is a very different medicine than a daily dose for transplantation.
- Contraception during dosing windows is essential in trials until the field proves that brief exposure has no effect on embryo development. The point is to preserve future options, not to complicate a near-term pregnancy.
- Safety monitoring should focus on mouth ulcers, lipid changes, and infection risk. These are known, quick to track, and reversible with dose holds.
If VIBRANT and similar pilots show slower decline in ovarian reserve with preserved cycle regularity and clean safety, the path to larger studies opens.
Ovarian aging as a tissue ecosystem
The Science reporting revealed a network. Sympathetic nerves densify with age. Glial-like cells appear where few expected them. Fibroblasts tilt toward collagen production and scarring. Immune cells shift toward a state that clears debris but may amplify inflammation if left unregulated. Eggs do not scatter evenly. They cluster in pockets that likely share microvascular and stromal features. Aging reduces egg density inside those pockets and may stiffen the surrounding matrix. In mice, cutting back sympathetic input increased reserve but reduced the number of eggs that matured, which hints that nerves help tune the balance between saving for later and investing in now. That is a lever worth learning to use.
Clinically, this reframing changes the questions we ask. Instead of only asking how many eggs remain, we should also ask how stiff is the stroma, how inflamed is the microenvironment, how are the nerves and blood vessels patterned, and what are macrophages doing this month.
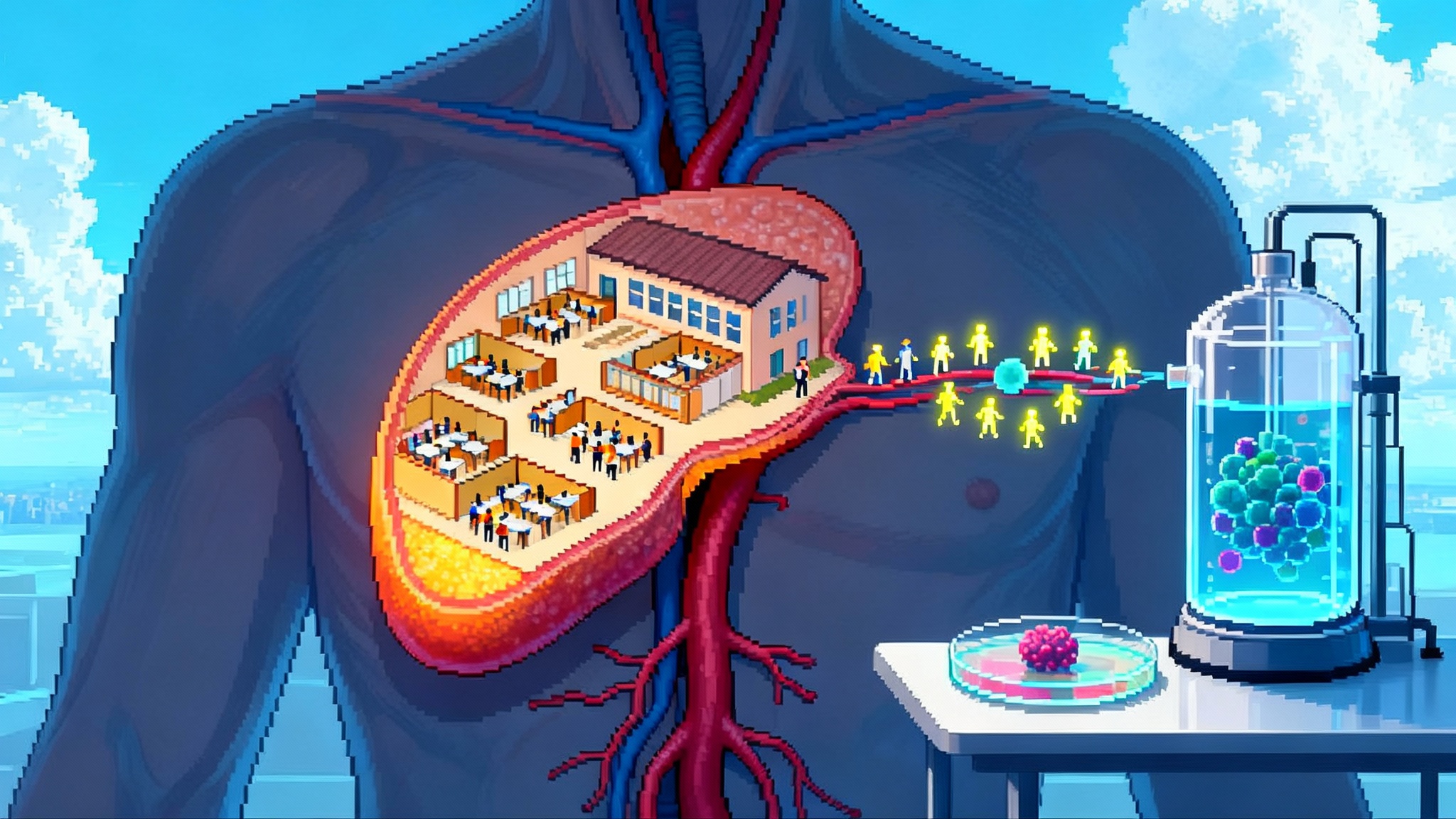
The mitomeiosis milestone
Mitomeiosis is a hybrid choreography of cell division. OHSU investigators removed the nucleus from a donor human egg, inserted a skin cell nucleus, and then triggered a process that shed half the chromosomes. The result was eggs that could be fertilized and reach the blastocyst stage in a minority of cases. The embryos were not transferred. Chromosomal errors were common and the team is clear that the road to any clinical use is long.
Why it matters now: even a distant possibility of creating eggs for women who lack them changes how we think about ovarian reserve. It suggests a future where preserving and restoring the ovarian endocrine ecosystem may be as important as preserving egg number. It also pushes the field to improve how we measure egg quality, spindle integrity, and mitochondrial function, because those will be the first practical gates. For context on mitochondria’s role in aging, see how cellular energy becomes care in 2025.
What counts as success in the clinic
The field needs endpoints that regulators, clinicians, and patients all trust. The good news is that ovarian biology gives us multiple dials to read within one to two years.
Short horizon endpoints for early trials
- Anti-Müllerian hormone, antral follicle count, and follicle stimulating hormone. These three track reserve from different angles and respond within months.
- Cycle regularity and length distribution. Subtle changes can signal ovarian-pituitary communication shifts.
- Ultrasound features of stromal health. Follicle counts are not the only readout. Stromal echogenicity and blood flow patterns carry information about fibrosis and angiogenesis.
- Menstrual blood biomarkers. Cells and proteins collected at home can report on inflammatory tone and extracellular matrix remodeling month by month.
- Safety signals. Oral lesions, lipids, infections, and any cycle disruptions. Safety is an endpoint, not a footnote.
Medium horizon endpoints for pivotal trials
- Euploidy rate in embryos for patients who go through in vitro fertilization during or after treatment. Even small improvements are meaningful.
- Time to menopause for peri-menopausal participants. A delay of one to two years would be a landmark outcome if safety holds.
- Vasomotor symptoms, sleep, mood, and cognition across the transition. The ovary talks to the brain; we should listen.
- Bone mineral density and cardiovascular risk markers. Menopause shifts these systems. Slowing the shift should show up in dual-energy X-ray absorptiometry scans and lipid panels. For the vascular angle, see how arteries emerge as aging's command hub.
Exploratory biomarkers
- Serum and stool proteomics and metabolomics to capture systemic effects of ovarian signaling.
- Circulating cell-free mitochondrial DNA and extracellular vesicles from the reproductive tract as windows into cellular stress and turnover.
- Elastography of the ovary to quantify stiffness noninvasively, analogous to liver fibrosis staging.
An accelerationist, safety-first roadmap
Here is a concrete plan to move fast without cutting corners.
1) Start in fertility clinics, not primary care
- Who: healthy women 35 to 45 with regular cycles who are not trying to conceive for at least a year. This matches inclusion windows where change is measurable but risks are low.
- What: low weekly rapamycin or matched placebo for three months, then nine months of follow-up. Layer in standardized ultrasound, hormone panels, and digital symptom diaries. Contraception is required. Vaccination status is checked. A prespecified algorithm pauses dosing for any concerning lab value or infection.
- Why: these clinics already deliver sensitive imaging and hormone testing. They can detect small changes that trials in general clinics would miss.
2) Formalize the ecosystem readout
- Add Doppler measures of ovarian blood flow and quantitative ultrasound scores of stromal patterns.
- Bank menstrual blood monthly for proteomics and immune profiling. This is cost effective and scalable.
- Run a sub-study with magnetic resonance elastography or emerging ultrasound elastography to measure stiffness as a proxy for fibrosis.
3) Bring anti-fibrotic and pro-resolution biology into the queue
- Target product profile A: a local ovarian anti-fibrotic microdose, delivered during egg retrieval for in vitro fertilization patients who already undergo transvaginal access. The dose is low, local, and reversible. The endpoint is change in stromal stiffness and inflammatory markers over three months, plus standard fertility outcomes in patients who proceed to transfer later.
- Target product profile B: a systemic short-course immune tone modulator that nudges macrophages away from a giant cell fusion state and toward homeostatic debris clearance. Safety monitoring mirrors rapamycin trials. The primary endpoint is a tissue immune signature in menstrual blood.
4) Build a menopause-delay stack
- Combine low weekly rapamycin with lifestyle interventions that also shift mTOR and inflammation in the same direction: time-restricted eating aligned to the individual’s schedule, resistance training that keeps bone and muscle responsive to hormones, and sleep protocols that regularize circadian signals. The stack is not hand-waving. Each element has a measurable readout.
5) Keep guardrails visible
- No use in anyone actively trying to conceive until high-quality data show no risk to embryos. Negative pregnancy tests are documented before each dosing block.
- Independent data safety monitoring. A stoppage rule lives in the protocol and triggers review if infections, cycle disruption, or lab changes pass a preset threshold.
- Equity by design. Recruitment includes coverage for transportation and childcare. Results are shared in plain language with participants.
6) Spill over into broader aging care
- As soon as endocrine benefits are detected, integrate ovarian metrics into midlife health visits. A practical package might include antral follicle count, anti-Müllerian hormone, lipid panel, hemoglobin A1c, and a short symptom index. The visit ends with a personalized plan: hormone therapy options when appropriate, bone protection, cardiovascular prevention, and sleep and mood support.
- If menopause delays by even one to two years in safe trials, the downstream cost savings in fractures, cardiovascular events, and work absence are large. That makes payer pilots realistic.
Where companies fit right now
- Drug developers can pursue short-course, low-burden agents that act on fibrosis, immune tone, or nerve signaling inside the ovary. The winners will offer clean safety, simple dosing, and endpoints that move within a year.
- Fertility tech companies can productize ecosystem imaging and menstrual blood assays as part of ovarian wellness programs, not just fertility cycles. Think standardized scans and kits with validated lab partners.
- Startups in in vitro gametogenesis should double down on quality control and safety science. Mitomeiosis will need better error-checking, better spindle assessment, and better mitochondrial quality measures before any clinical path is plausible. The scientific story is already reshaping how we study egg quality for standard in vitro fertilization.
What to watch in 2026
- The readout from the first VIBRANT cohort and clarity on the size and sites for the multicenter follow-up.
- A wave of ecosystem papers that test whether nerve density, fibroblast programs, and macrophage states predict time to menopause better than reserve alone.
- Early elastography and menstrual proteomics pilots that give clinics new noninvasive dials to read.
- Responsible progress in mitomeiosis. The goal is not pregnancy. It is a steady drop in chromosomal errors and a rise in healthy cell division dynamics under strict oversight.
The bottom line
The 2025 headlines are not hype. They are signals that ovarian biology is now measurable, actionable, and central to healthspan. Rapamycin trials test a thermostat that sets how quickly the reserve drains. Ecosystem mapping shows where fibrosis, immune tone, and nerves push the ovary off course and where that drift can be corrected. Mitomeiosis stretches our imagination about egg supply and forces higher standards for measuring egg quality.
The fastest way to move the needle on midlife health may be to treat the ovary as both an organ and a neighborhood. If we track the neighborhood, modulate the thermostat, and test local fixes with the same care we bring to fertility procedures, then delaying menopause by even a small amount becomes a realistic goal. The consequence is bigger than timing. It is a shift toward longer, steadier hormonal health that makes every downstream prevention tool work better. That is how a single organ becomes a lever for the decade.