Pig Kidneys Arrive: 2025 Trials and the Healthspan Shift
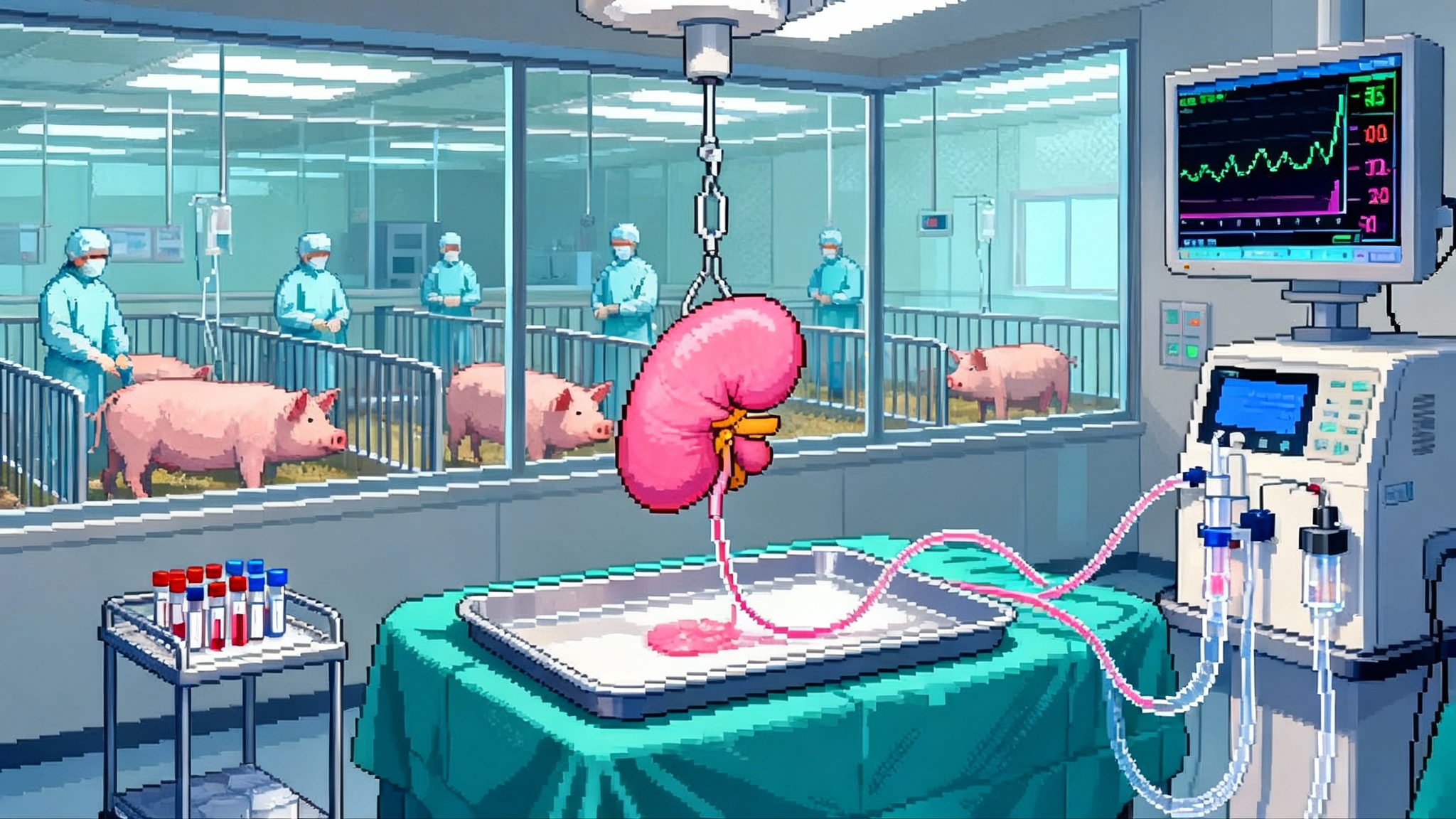
In 2025, the FDA cleared the first clinical trials of gene-edited pig kidneys and patients set record survival times. Here is what those milestones mean for healthspan and when xenokidneys could reach routine care.
The year pig kidneys stopped being hypothetical
For decades xenotransplantation felt like a moonshot: always ten years away. Then 2025 arrived with two facts that changed the conversation. First, the United States Food and Drug Administration cleared the first formal clinical trials of pig-to-human kidneys, including studies designed to support market approval rather than one-off exceptions. That signal, delivered in early February, turned a research frontier into a regulated development path and defined who would go first: older adults with end-stage kidney disease who are unlikely to get a human organ in time FDA clears first kidney trials.
Second, living recipients began to set records measured in many months rather than days. In late October a New Hampshire man reached 271 days with a working pig kidney before returning to dialysis, a span that would have sounded impossible two years ago record 271-day recipient.
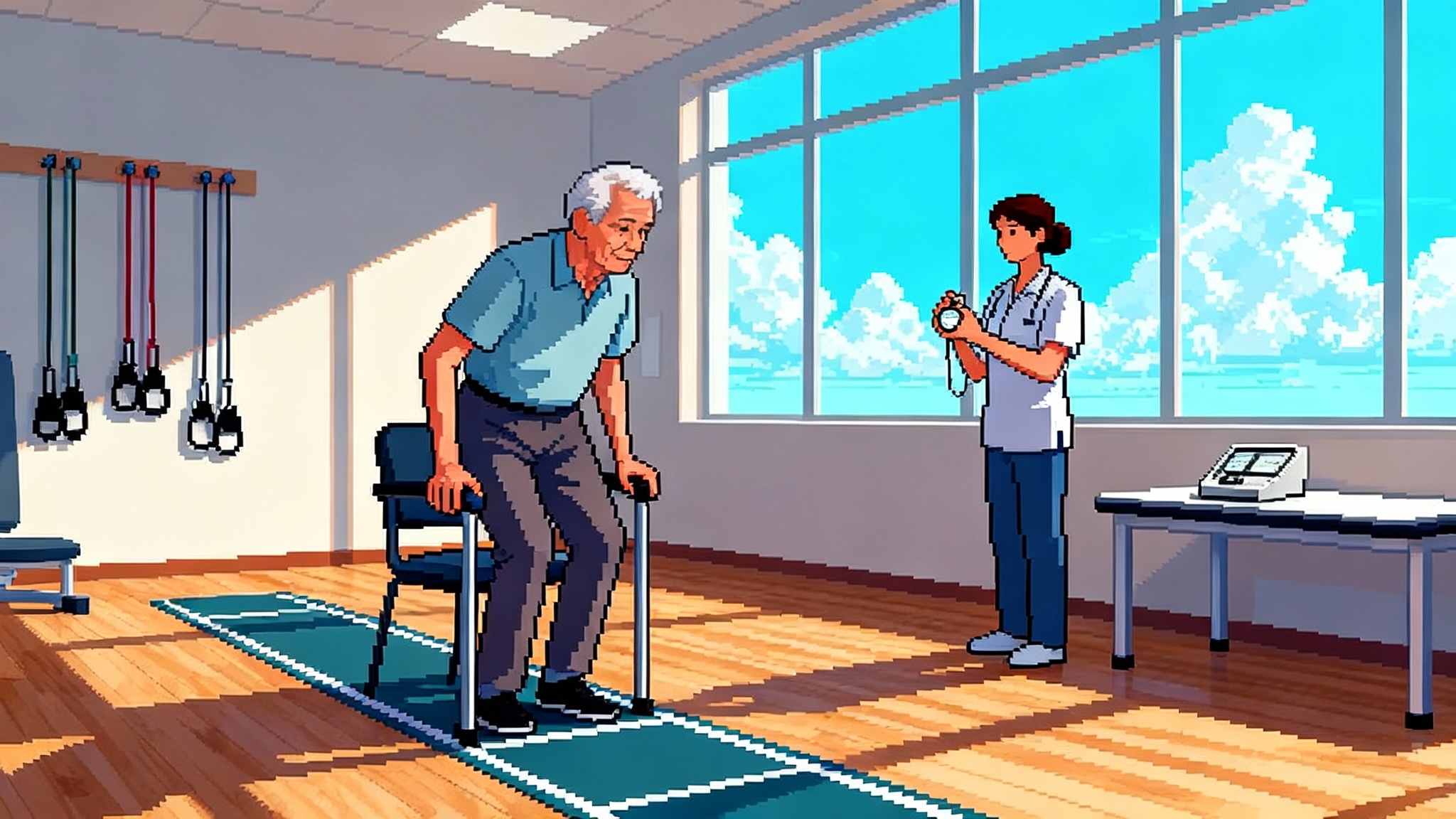
Those developments matter because kidneys are the bottleneck of modern transplantation. Most of the more than 100,000 Americans on the transplant list need a kidney, and thousands die each year while waiting. Dialysis can keep people alive, but it often traps older adults in a narrow life defined by clinic schedules, fatigue, and repeated hospitalizations. If we can safely deliver a kidney that buys even one to three good years off dialysis for people in their sixties and seventies, that is not just longer life. That is more life that feels like life.
What changed inside the lab
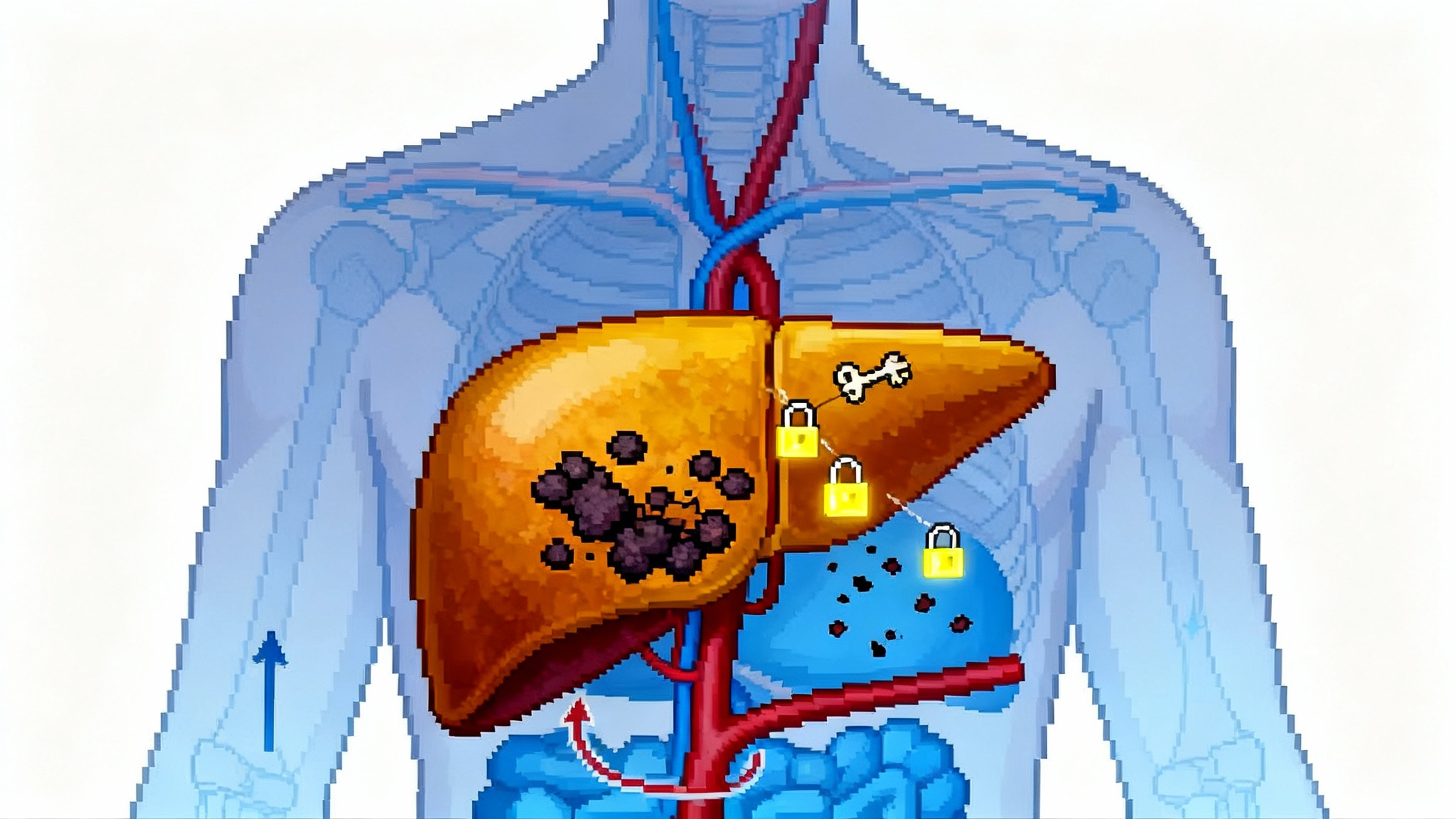
A pig kidney must do three things to work in a human: avoid immediate immune destruction, avoid clotting to death inside foreign blood, and avoid slow chronic rejection. Think of it like fitting a foreign plug into a wall socket. You need an adaptor for the shape, a transformer for the voltage, and surge protection for unpredictable spikes.
The adaptor is genetic editing to remove surface sugars that human antibodies attack at first contact. Today’s donor pigs usually lack the enzymes that create three major carbohydrate antigens: Gal, Neu5Gc, and SDa. Remove those, and the organ is no longer covered in bright targets.
The transformer is a set of human genes added to the pig to quiet the complement system and the clotting cascade. Common inserts include human CD46 and CD55 to control complement, thrombomodulin and endothelial protein C receptor to keep the microvasculature from clotting, and CD47 to signal do not eat me to macrophages. Some programs add HLA-E to discourage natural killer cells. Many also delete the pig growth hormone receptor so the organ does not keep growing after it is transplanted into an adult.
Surge protection comes from the drug stack patients receive. The field is moving away from calcineurin-heavy regimens and toward costimulation blockade, which targets the handshake between T cells and antigen-presenting cells. Belatacept is one option. Anti-CD40 pathway agents are another. Centers usually add mycophenolate and steroids, plus targeted antivirals when needed. The aim is to minimize the specific pathways that make xenografts thrombose and scar, while keeping overall infection risk manageable in older patients. Immune recalibration is a recurring theme across aging medicine; compare these approaches to thymus reboot strategies in 2025.
A final piece of the engineering stack tackles a viral risk that sits inside the pig genome. Porcine endogenous retroviruses, or PERVs, are ancient viral sequences that could, in theory, infect human cells. Modern donor pigs are bred in pathogen-controlled facilities and their genomes are edited to inactivate PERV sequences across many sites. That is like removing every match and lighter from a room rather than simply posting a no open flames sign. Regulators still require extended monitoring of recipients and their close contacts for signs of unusual infections. So far there is no evidence of PERV transmission in people.
Safety, explained plainly
Two risks dominate the safety conversation.
-
Rejection and clotting: Hyperacute rejection is the instant destruction that doomed older experiments. Carbohydrate edits and human complement regulators turned this from an automatic failure into a manageable event. The remaining concern is a mix of antibody mediated injury and microvascular clotting that can accumulate over weeks to months. That is why trial endpoints include not just survival but kidney function, biopsy findings, and markers of endothelial injury.
-
Zoonosis: The worry is not seasonal flu. It is a low-probability risk of a pig virus adapting to humans. Donor herds live in designated pathogen-free facilities, with air handling, sterilized feed, strict personnel flow, and routine surveillance by polymerase chain reaction panels and culture assays. Organs are tracked from animal to recipient, and recipients are enrolled in long-term virology monitoring. It is similar to how the blood supply is screened and traced, only with whole genomes and lifetime follow-up.
For readers seeking a mental model, think of the safety stack as Swiss cheese. Each layer has holes. Stack enough layers, and the holes no longer line up.
The trials that will decide the future
Here is how the first wave of trials is structured.
-
Who gets in: Mostly adults over 50 on dialysis who are either medically ineligible for a standard kidney transplant or unlikely to receive one in time. Some protocols prioritize patients with hard-to-match blood types or highly sensitized immune systems. The goal is to test xenokidneys where the benefit is clearest and the alternative is years of dialysis with poor quality of life.
-
What success looks like: Primary endpoints focus on safety and function at 24 weeks. That window captures early rejection patterns, drug side effects, infections, and whether patients can live off dialysis with steady creatinine and acceptable estimated glomerular filtration rate. Secondary endpoints extend to 12 months, including hospital days, infections like cytomegalovirus or BK virus, biopsy-proven rejection, and measures of daily functioning.
-
How the studies progress: Sponsors are using adaptive designs that start with small cohorts and add patients if predefined safety and efficacy signals are met. Importantly, at least one program is set up as a phase 1 to 3 continuum. If the grafts perform for a year with consistent safety, the dataset can support a biologics license application. That is different from one-off compassionate use cases. It is a path toward labeling and reimbursement.
-
What the regulators watch: Beyond the usual transplant risks, regulators will scrutinize donor herd biosecurity, chain-of-custody for organs, hospital infection control, and recipient monitoring plans that extend for years. Sites will need protocols for sample banking so that any signal of unusual infection can be traced back and investigated.
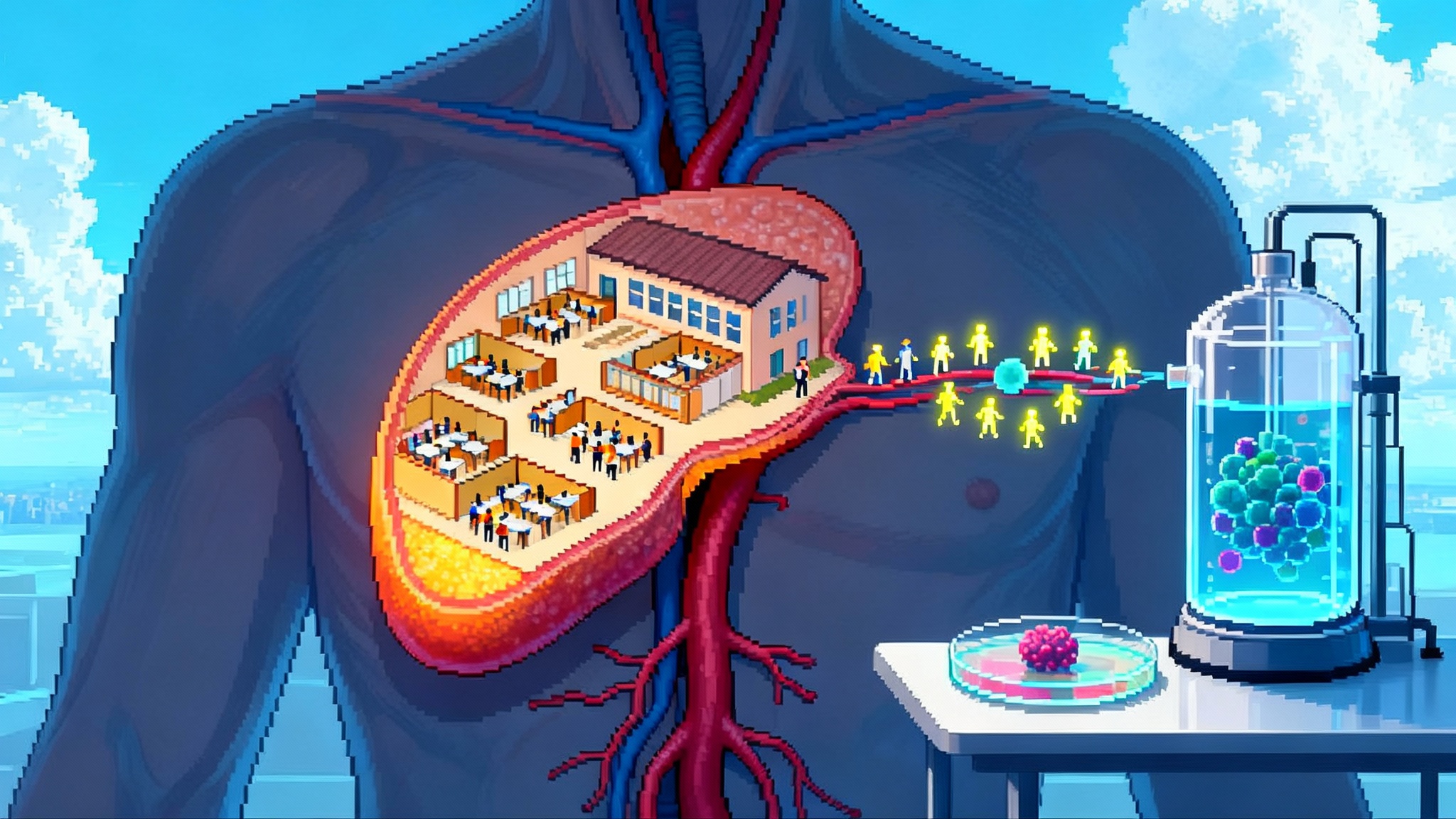
Manufacturing organs at scale
Gene-edited organs require a supply chain that looks more like a semiconductor fab than a farm.
-
Founders and breeding: It starts with a small number of genetically defined founder pigs. Those founders are screened to the base pairs and kept in biosecure rooms with positive pressure airflow. Their offspring become the donor herd.
-
Quality control: Every donor pig is genotyped to confirm all required edits and verify that no off-target changes affect safety. Health status must be documented for a long list of pathogens. Necropsy and histology check for silent disease.
-
Organ recovery and preservation: Harvest uses sterile operating rooms inside the facility. Kidneys are flushed and connected to machine perfusion to minimize cold ischemia time. Then they move in sealed containers to the hospital, under temperature and time control.
-
Cost today, cost tomorrow: Early on, costs will reflect boutique manufacturing. A single transplant can easily run several hundred thousand dollars when you include the organ, surgery, perfusion technology, and intensive monitoring. The critical question is the slope of the cost curve. As donor herds expand and dedicated recovery teams standardize processes, fixed costs spread across more organs. Early modeled scenarios suggest that the organ component can fall dramatically with volume because the biology is reproducible and the per-pig variable costs are low. Compare that to dialysis, which accrues costs every month for staff, consumables, and hospitalizations. If a pig kidney delivers one to two years off dialysis with acceptable quality of life, it has a credible path to cost parity for payers within a few years of scale.
-
Who pays: In the United States, Medicare covers end-stage renal disease regardless of age. That accelerates health technology assessment. Expect coverage to begin with narrow criteria in centers of excellence. As data mature, indications can widen and bundled payments can evolve to reward one-time interventions that replace years of chronic care.
What better looks like for older adults
Healthspan is not a slogan. It is the distance between being alive and being well. Consider a realistic case.
A 68-year-old on thrice-weekly dialysis wants to attend a granddaughter’s graduation in another state. Travel is complicated by dialysis schedules, fluid restrictions, and the fatigue after treatments. A xenokidney that functions for even 12 to 18 months turns that calendar into something flexible again. The risk is not zero, and the drug regimen needs monitoring, but daily living changes from defensive to proactive. Walks become longer. Meals feel less choreographed. Hospital time drops. If the organ ultimately fails and dialysis resumes, those months still count as life lived. For a broader view on turning aging biology into care, see our overview of mitochondria-driven healthspan advances.
This is the near-term promise: not a fantasy of permanent replacement, but real years off machines for people old enough that the human donor waitlist is a dead end.
The immune engineering stack, in plain English
-
Carbohydrate edits: Remove the three mailbox flags that make the human immune system deliver rejection letters to pig tissue the moment blood flows. Less instant attack means time for drugs to work.
-
Human complement regulators: Install brakes so complement proteins do not punch holes in cells that look foreign. This reduces the fireworks that cause hyperacute rejection.
-
Thromboregulation: Add proteins that keep the endothelium, the inner lining of vessels, from lighting up the clotting system. That prevents the slow shutdown of the kidney’s fine filters.
-
Growth control: Stop the pig kidney from growing after the transplant by deleting the growth hormone receptor. A stable size is kinder to the human abdomen and its blood supply.
-
PERV inactivation and biosecurity: Remove the viral matches from the pig genome and keep the herd in a clean room. Then watch recipients for years, with a plan if any odd virus appears.
-
Drug stack tuned for xenografts: Use costimulation blockers to quiet the precise T cell handshake that triggers xenograft inflammation. Layer mycophenolate and steroids as needed. Adjust for infections with preemptive monitoring rather than waiting for symptoms. For more on immune system resets, see thymus reboot strategies in 2025.
What to watch next
You can gauge the field’s progress with a simple dashboard.
-
Six-month function with no dialysis: The number of recipients who hit this mark is the day-to-day scoreboard. It shows that early rejection and clotting are under control.
-
Biopsy and proteinuria trends: Less microvascular injury and stable or falling protein in urine signal that the filters are staying healthy.
-
Infection rates and severity: Cytomegalovirus and BK virus are known issues. Look for protocols that prevent rather than chase these infections.
-
Repeatability across centers: Success at one site could be magic. Success at three sites starts to look like a product.
-
Manufacturing throughput: How many donor pigs reach transplant-grade status each quarter. Supply matters because organ access determines real world impact.
Timelines without wishful thinking
-
2025: First cohorts dosed under Food and Drug Administration cleared protocols. Recipients are mostly older adults on dialysis with poor prospects for a human organ. Milestone recipients cross the six to nine month mark and some beyond. Record-setting cases prove possibility, not certainty.
-
2026: Enrollment expands at a small number of centers. The key unknown is durability. If a sizable fraction of grafts reach 12 months with acceptable quality of life and manageable safety, payers begin to model coverage for narrow use. Manufacturing ramps and costs begin to slide. Similar one-and-done strategies are emerging in other areas, including one-shot osteoarthritis gene therapy.
-
2027 to 2028: If one program achieves consistent 12-month outcomes and reproduces them at multiple sites, a biologics license application becomes credible. Expect early, center-limited routine use for select older adults who are unlikely to receive a human kidney in time. Hospital teams refine care pathways and discharge plans.
-
2029 and beyond: With label approval, coverage policies, and scaled supply, xenokidneys become a real option in many transplant centers. The focus shifts from whether it works to how to optimize drug regimens, minimize infections, and extend graft life to multi-year horizons.
These dates are conditional on the data. The gating item is not a headline. It is the necessary work of collecting enough consistent outcomes to convince regulators, clinicians, and payers that the risk-benefit balance holds.
Practical takeaways for different readers
-
Patients and families: Ask your nephrologist if your center participates in xenotransplant studies and whether your profile fits early cohorts. Keep an updated list of comorbidities and infections. If you are interested, prepare for intensive follow-up and travel to a participating center.
-
Clinicians: Build multidisciplinary teams now. You will need transplant surgery, nephrology, infectious disease, virology, pathology, and pharmacy aligned on protocols for biopsies, prophylaxis, and data capture. Define who you would consider for early referral and why.
-
Health systems: Invest in biosecure specimen handling and long-term follow-up infrastructure. Xenograft recipients generate unique data obligations that can be a differentiator for your program if you plan ahead.
-
Policymakers and payers: Design coverage with evidence development models that reimburse early use while funding the monitoring needed to make population risk transparent. Tie payments to predefined outcomes like dialysis-free days and infection control milestones.
-
Builders and investors: The fragile point is not gene editing. It is industrial biosecurity and logistics. Companies that can scale clean-room animal husbandry, verify edits, and deliver organs with minimal ischemia will create value regardless of which genetic recipe wins.
The bottom line
In 2025, pig kidneys moved from audacious experiment to regulated medicine in progress. The first trials are targeted, the engineering is specific, and the early human stories are long enough to count. Do not expect magic. Expect a steady expansion of dialysis-free life for people who otherwise had little to hope for, with safety watched closely and manufacturing built like a modern industry. If the next few years match the early signal, older adults could see pig kidneys become a routine option before the decade closes. That is what a real healthspan breakthrough looks like: not a slogan, but a calendar that opens back up.