Retro’s Alzheimer’s Pill Bets Big on Autophagy and Aging
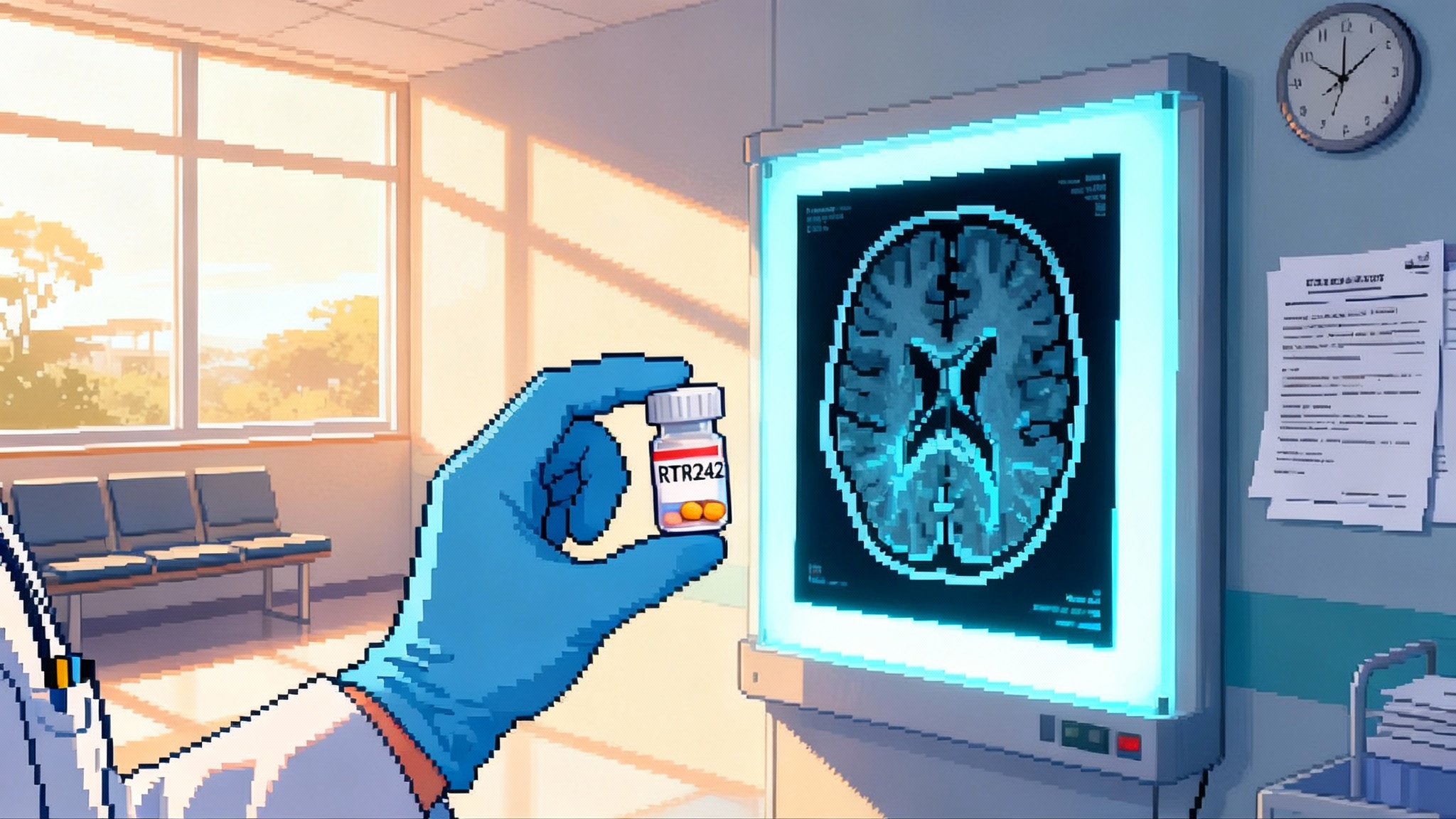
Retro Biosciences plans to dose its first human study of RTR242, an autophagy-boosting Alzheimer’s pill, in Australia by late 2025. Here is why the pathway matters, the biomarkers to watch, and how this bet could reshape longevity biotech.
The first real-world test of autophagy as a longevity lever
Retro Biosciences is turning a classic longevity hypothesis into a clinical bet. The company says it will begin dosing its first human trial of RTR242, an autophagy-targeting oral drug for Alzheimer’s disease, in Australia by late 2025, citing the country’s relatively fast first-in-human setup for early studies. That timeline, and the choice of Alzheimer’s as the opening indication, is a deliberate wedge into a larger ambition: extend healthy human lifespan by fixing cellular clean-up that declines with age. Retro discussed the plan publicly alongside a scale-up push and identified Alzheimer’s as the first proving ground for this approach (RTR242 dosing in Australia by late 2025). For more context on the strategy, see our coverage of Retro's first trial overview and how autophagy and AI in aging are converging.
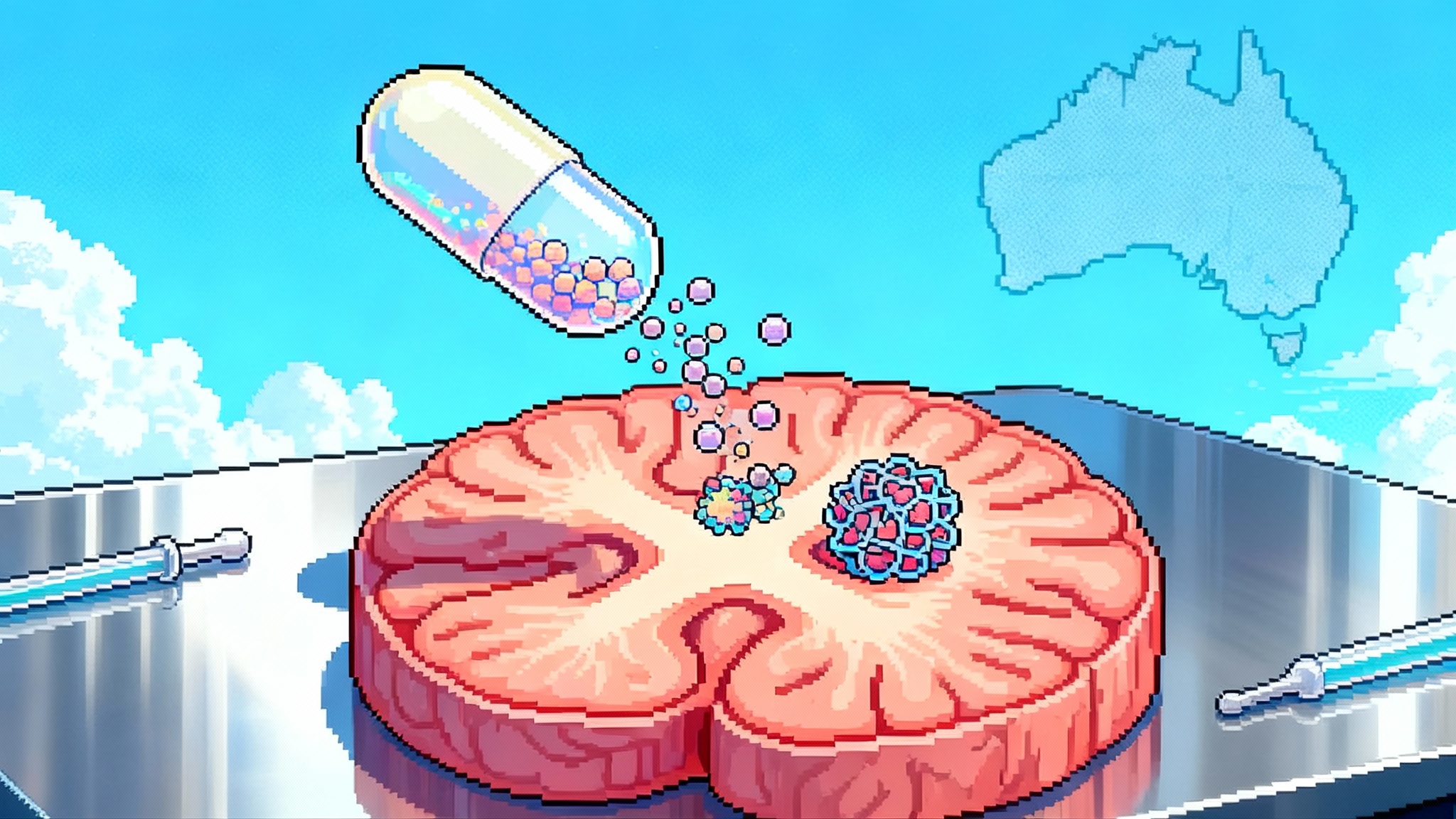
The logic threads together three ideas. First, autophagy is the cell’s recycling system, and its efficiency drops with age. Second, autophagy failure shows up across neurodegenerative diseases where toxic proteins and damaged organelles pile up. Third, if a drug safely restores autophagic flux in the human brain, it could clear protein clutter, calm inflammatory signaling, and potentially slow or reverse functional decline. If that works in Alzheimer’s, it strengthens the case for using the same pathway in other age-linked conditions.
Why autophagy is a credible target
Autophagy is not a single on-off switch. It is a pipeline. Cells identify cargo, form autophagosomes, fuse with lysosomes, and then degrade and recycle their contents. With age and in neurodegenerative disease, that pipeline stalls. Autophagosomes accumulate, lysosomes acidify less effectively, and cargo like misfolded proteins and broken mitochondria persists. A broad research base across models and human tissue supports this picture and links improved autophagy to healthier brain aging. A recent Neuron review synthesizes this evidence and underscores how restoring autophagic flux can reduce toxic protein burden, clear dysfunctional organelles, and dampen senescence and neuroinflammation in the nervous system (autophagy in age-related neurodegeneration).
Autophagy is attractive for longevity because it sits upstream of several failure modes. Rather than tune one protein target, a drug that restores flux can influence multiple hallmarks at once: proteostasis, mitochondrial quality control, and inflammatory tone. In practical terms, a successful autophagy modulator could be useful across diseases where pathological protein and organelle accumulation matter, not just in Alzheimer’s.
Alzheimer’s as the aging adjacent wedge
There is no regulatory pathway to approve a drug for aging. Companies that want to test aging biology pick diagnosable diseases where the same pathways are at play. Alzheimer’s is a logical wedge if your thesis is that cellular housekeeping failure drives pathology, because it contains three intersecting problems: amyloid and tau pathology, microglial dysfunction, and overall proteostasis collapse. The disease also has established clinical endpoints and a maturing toolbox of fluid and imaging biomarkers, which lets a company show pharmacodynamic activity and clinical signal in a way regulators recognize.
Australia is a sensible choice for first-in-human work because startup timelines can be shorter for Phase 1, and early safety and pharmacokinetics can be studied before expansion into larger efficacy trials elsewhere. If Retro begins with a multiple-ascending-dose safety study, the earliest readouts will not be memory scores. They will be safety, tolerability, pharmacokinetics, and exploratory pharmacodynamic signals that suggest autophagy is being nudged in the intended direction. For longevity market context, see our take on GLP-1 longevity math.
What would count as compelling proof
For a drug that claims to revive autophagy and improve cognition, it is important to separate near-term proof of mechanism from longer-term proof of benefit.
Near-term pharmacodynamic evidence
- Markers of autophagic flux in peripheral blood cells. Increases in LC3-II turnover with concurrent decreases in p62/SQSTM1, interpreted with inhibitors or pulse-chase designs to capture flux, not just static levels.
- Lysosomal function indicators. Changes in lysosomal pH or cathepsin activity in ex vivo assays of patient-derived cells, or transcriptomic signatures consistent with TFEB activation and lysosome biogenesis.
- Proteostasis stress signals. Reduction in ubiquitinated protein load or heat-shock response markers in accessible compartments like PBMCs, interpreted as flux.
- Inflammatory tone linked to proteostasis. Shifts in cytokine profiles and microglial activation markers that are plausibly downstream of improved clearance rather than nonspecific immunosuppression.
Central nervous system signals
- Plasma and CSF neurodegeneration biomarkers. Decreases in neurofilament light chain and GFAP suggest reduced ongoing neuronal and astrocytic injury. These are not autophagy-specific, but they move in many neuroprotective contexts and are sensitive in short studies.
- Alzheimer’s proteinopathy markers. Favorable shifts in plasma or CSF p-tau species and Aβ42/40 ratio would be encouraging. They would not prove autophagy was the mechanism, but they show movement on core disease axes.
- Imaging biomarkers. While amyloid and tau PET are established, microglial activation via TSPO PET or other tracers could help connect improved proteostasis to inflammation reduction. A drug that claims to clean up could eventually be asked to show less accumulation or faster clearance of pathology in vivo.
Cognitive and functional endpoints
- Early-phase studies can include sensitive cognitive composites that move faster than traditional outcomes. Examples include PACC-like composites or computerized episodic memory tasks that detect subtle change over weeks to months.
- Later-phase Alzheimer’s trials often use endpoints such as CDR-SB and ADAS-Cog. A therapy that claims to restore cellular housekeeping will ultimately need to show patients function better for longer, not only look better on molecular readouts.
The most persuasive package would show a chain of evidence: target engagement and flux restoration in peripheral assays, concordant movement in brain injury or proteinopathy biomarkers, and a trend in a sensitive cognitive composite. That does not prove rejuvenation in a philosophical sense, but it would validate a mechanism that can be reapplied in other age-linked indications.
How autophagy modulators compare to senolytics and mTOR inhibitors
Autophagy upregulators, senolytics, and mTOR inhibitors all connect to aging biology, but they aim at different nodes and carry different trade-offs.
- Autophagy modulators. The goal is to restore flux and improve cellular housekeeping directly. Advantages include the potential to touch multiple hallmarks at once and a direct link to proteostasis in neurons and glia. Risks include hitting the wrong part of the pathway and causing stalled autophagosomes or lysosomal stress, or overshooting and triggering unwanted catabolism. The best versions should tune flux rather than flip it fully on.
- Senolytics. These aim to remove senescent cells that secrete inflammatory factors and disrupt tissue function. In the brain, early studies suggest senescent glia and vascular cells may contribute to pathology. Small clinical pilots in Alzheimer’s with combinations like dasatinib and quercetin have shown central penetration and acceptable safety over short periods, but no clear cognitive or biomarker efficacy yet in small samples. The approach could still complement autophagy drugs by reducing inflammatory noise, but the evidence base is early and dosing paradigms are intermittent by design.
- mTOR inhibitors. mTORC1 inhibition, as with rapamycin analogs, indirectly upregulates autophagy as part of a wider metabolic reset. This may help multiple tissues at once and has strong animal data for lifespan and healthspan. The trade-off is breadth. mTOR affects protein synthesis, immune function, and metabolism, so chronic dosing in older adults demands careful titration to avoid immunosuppression and frailty. For Alzheimer’s, it is appealing mechanistically, but the clinical path has been cautious.
If your primary goal is to fix the clearance machinery in neurons and microglia without global metabolic braking, a first-in-class, brain-penetrant autophagy modulator has a clean story. That is likely why Retro chose it as the lead program for a neurodegenerative disease.
Designing endpoints that travel beyond Alzheimer’s
Retro’s strategy only pays off if the data can travel. If RTR242 shows a coherent package of autophagy flux restoration and brain injury reduction, the same biomarker palette could be ported into other indications where proteostasis failure matters. That includes frontotemporal dementia subtypes, Parkinson’s disease with prominent protein aggregation, and perhaps age-related cognitive decline without clear amyloid or tau drivers.
For this to work, the biomarker suite must be both mechanistically specific and operationally practical. The company will need robust, reproducible assays for LC3, p62, and lysosomal function in human samples, with standardized collection windows relative to dosing to capture flux rather than static levels. They will likely need a small, brain-relevant pharmacodynamic signature that can be used in rapid dose finding. On the clinical side, digital cognitive endpoints and passive functional measures from wearables can detect subtle changes faster than clinic visits alone and could help derisk larger Phase 2 designs.
Reading Retro’s ambitions on financing and scale
Retro launched with an unusually large seed and is now signaling a push to raise a very large Series A. If successful, that capital lets them run parallel bets: a small-molecule autophagy program for Alzheimer’s, plus cell-based approaches for blood and CNS disorders, and early work on in vivo reprogramming. It also changes trial strategy. With enough runway, a company can afford biomarker-intensive Phase 1b studies, adaptive Phase 2 designs with multiple doses and early futility looks, and global site activation that avoids long enrollment stalls.
A $1 billion raise, if it materializes, also sends a message to regulators and payers. It says longevity biology is not a fringe hobby. It is a platform that expects to deliver drugs that meet conventional standards in conventional diseases. The Alzheimer’s wedge makes that argument concrete. If an autophagy modulator can safely improve outcomes in a high-burden disease with validated endpoints, it is easier to argue that the same mechanism deserves attention in other aging-linked conditions.
What to watch between now and first dosing
- Chemistry and selectivity. How does RTR242 achieve brain penetration and pathway specificity. Does it target upstream sensors, autophagosome formation, or lysosomal function. Selectivity will matter for safety.
- Flux, not snapshots. Expect study designs that actually measure turnover. Static elevations of LC3-II without co-interpretation can indicate blocked degradation rather than improved cleanup.
- Concordance across layers. The most convincing early signal will be mechanistic biomarkers and brain injury markers moving together. A single cognitive measure is unlikely to shift in a short Phase 1, but consistent movement across multiple domains can justify a larger efficacy study.
- Safety in older adults. Many Alzheimer’s patients take multiple medicines, and some have frailty, diabetes, or vascular disease. Drug interactions and metabolic side effects will be closely watched.
The bigger picture for longevity biotech
The aging adjacent indication strategy is pragmatic. It forces longevity claims to meet the standards of disease medicine. It also creates an evidence loop. If a longevity pathway improves a disease outcome that matters, the case for using it prophylactically or in adjacent conditions strengthens. If it fails, the field learns where the mechanism does not translate.
Autophagy has one of the clearest mechanistic stories in this space. It connects to core failures in aged cells, it is druggable, and it touches endpoints that can be measured in months rather than years. Alzheimer’s is a hard first test, but it is also a visible stage to prove that a housekeeping pathway can move the needle in human brain aging.
Bottom line
Retro is using Alzheimer’s as a proving ground for a longevity pathway with broad relevance. The scientific case for autophagy is strong, the biomarker toolkit is ready, and the business plan is set up to scale if the first signals are convincing. From September 2025 through late 2025, the focus will be turning a clean narrative into clean data, then expanding to efficacy readouts in 2026 if early markers line up.