Alzheimer’s Blood Tests Hit Main Street in 2025: An Inflection Point
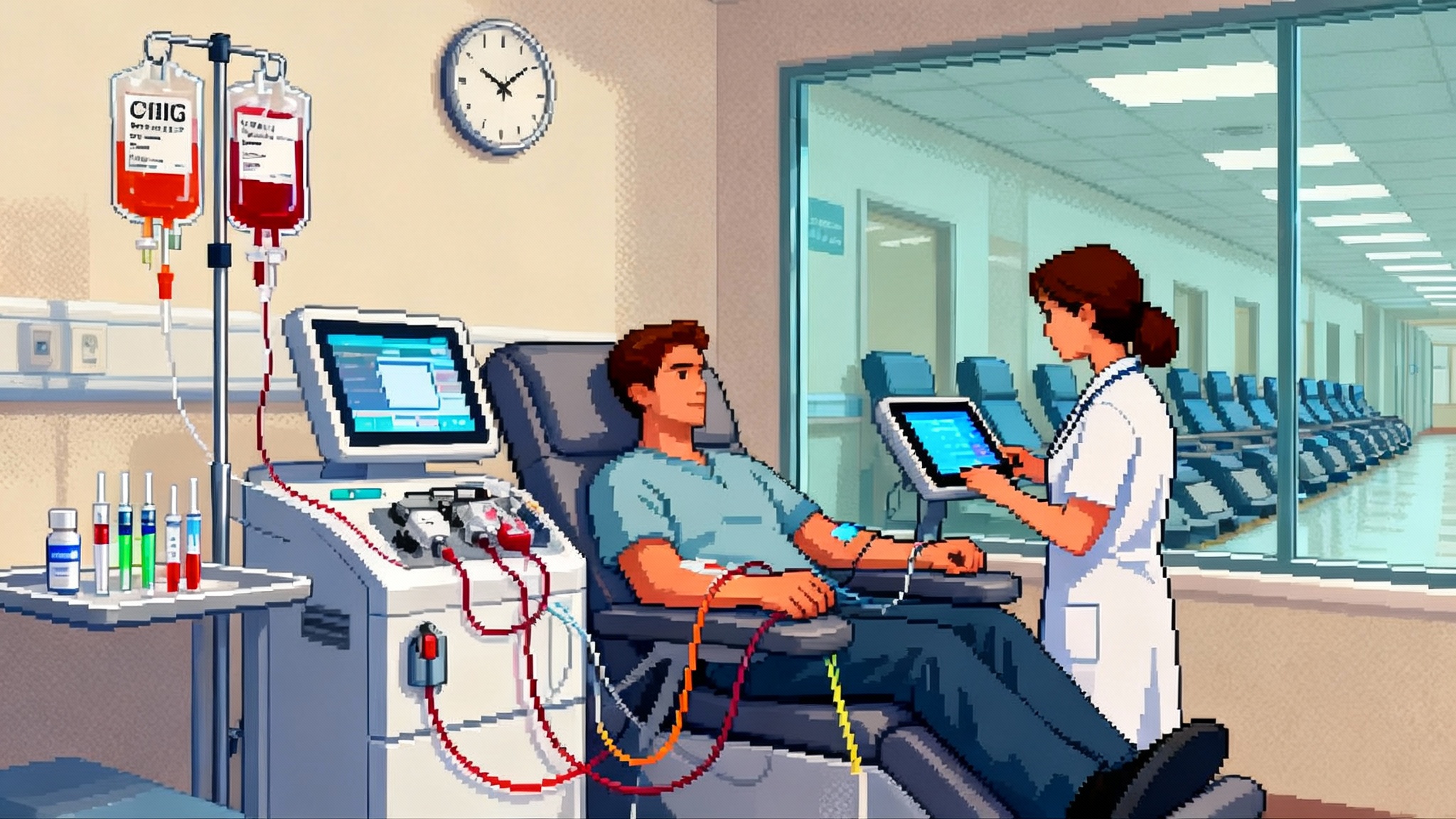
After 2025 FDA clearances of plasma p‑tau assays, Alzheimer’s detection is moving from PET scans and spinal taps to a simple blood draw in primary care. Here is how this shift will change diagnosis, coverage, and prevention for aging brains in the United States.
Breaking: a blood draw replaces the spinal tap moment
In May 2025, the United States turned a corner on how we find Alzheimer’s disease. The Food and Drug Administration cleared a blood test that measures phosphorylated tau 217 and beta amyloid 1-42 in plasma to help identify Alzheimer’s pathology. In one swoop, a process that used to require a radioactive brain scan or a spinal tap became possible with a tube of blood drawn at a local lab. The same year, another assay joined the party, designed to help primary care doctors rule out Alzheimer’s pathology so they can refer the right patients to specialists.
Two details matter most. First, the new tests can be ordered by front-line clinicians caring for adults with memory complaints. That brings diagnosis out of the specialist bottleneck and into the exam rooms where most older adults already are. Second, blood biomarkers are good enough, in carefully selected patients, to make the next steps faster and more precise. Instead of spending months ping-ponging between referrals and wait lists, patients can be triaged in days.
To be concrete: on May 16, 2025 the agency FDA cleared the first blood test to aid in diagnosing Alzheimer’s in symptomatic adults 55 and older. In October, Roche announced that its pTau181 blood test had United States clearance for use in the initial assessment in primary care, with data showing a very high negative predictive value in a real-world, early-stage population. Later in the year, Roche’s Elecsys pTau181 received clearance for that use.
These approvals do not turn a blood test into a stand-alone diagnosis. But they do turn it into a faster, cheaper, and more scalable gateway to a confident answer.
Why this is a longevity story
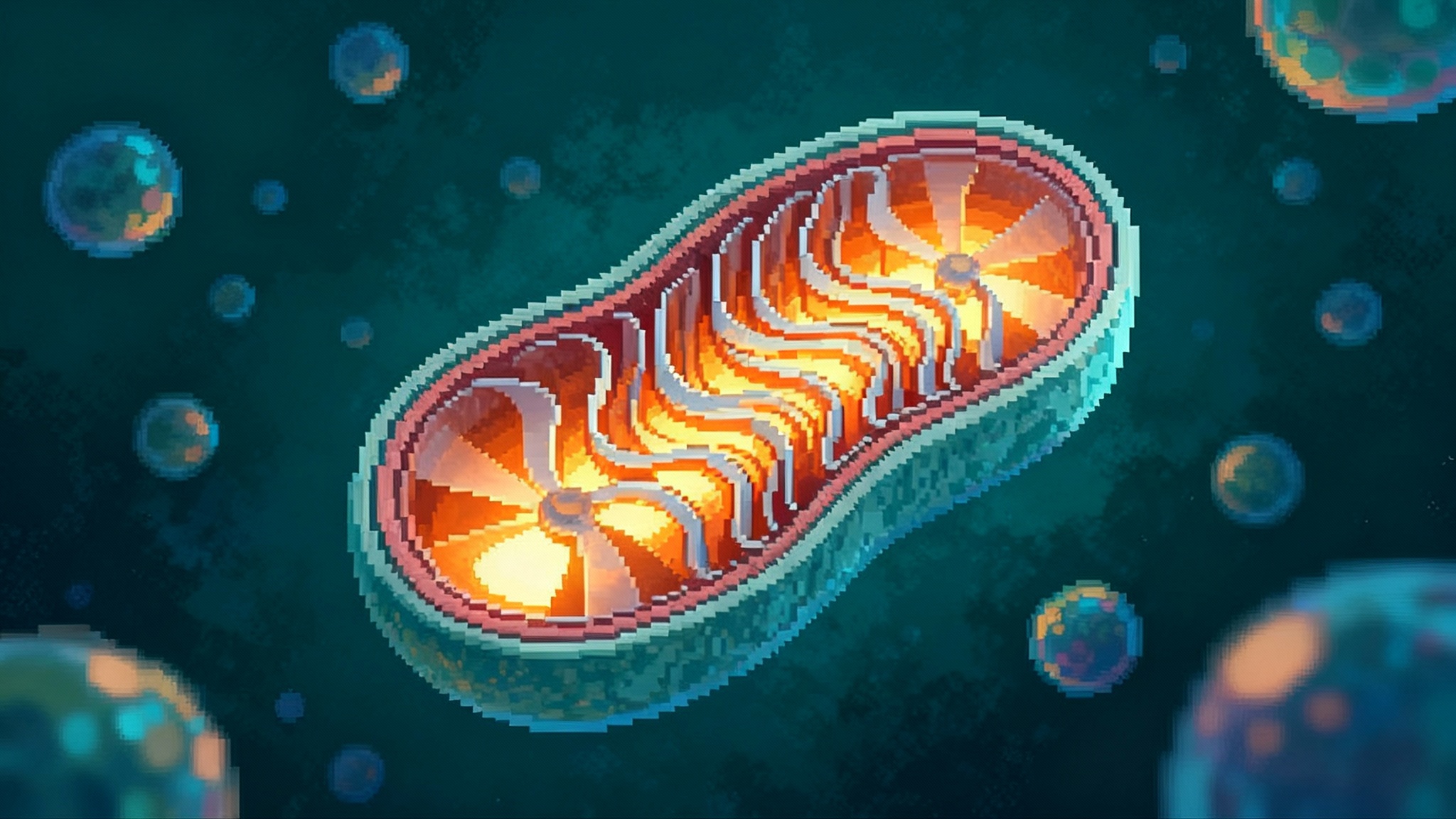
Longevity is not just about how long we live; it is about how long we live with our minds intact. Alzheimer’s is a decades-long biological process. For most people, amyloid and tau changes begin years before daily function slips. If we want to extend healthspan, we need to detect risk and early disease while people are still managing finances, driving safely, and staying employed. For a broader view of how upstream biology becomes clinical care, see how cellular energy becomes care.
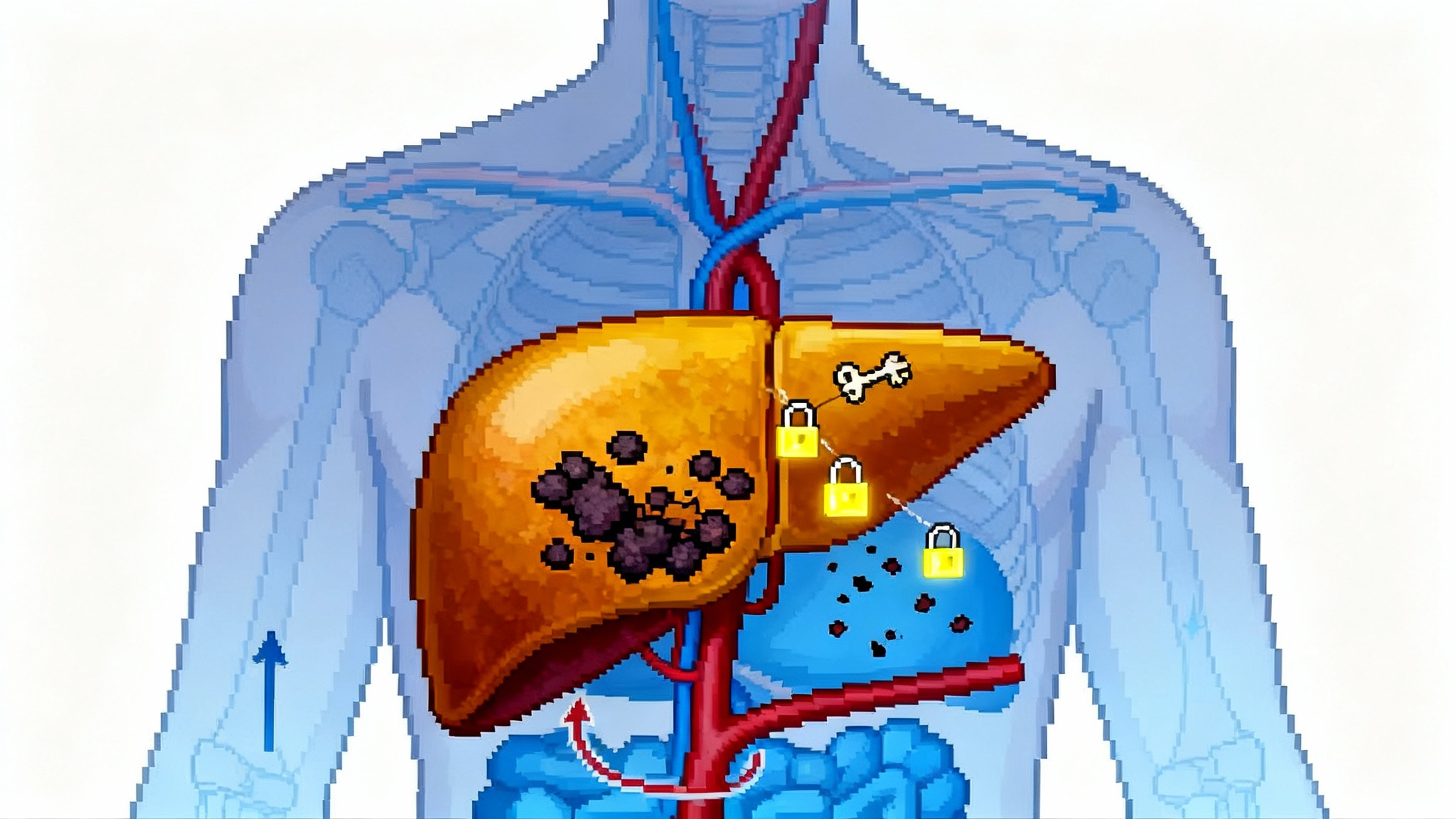
Blood biomarkers let primary care physicians identify who is unlikely to have Alzheimer’s pathology and who likely does. That alone reduces wasted time. The faster someone gets clarity, the faster they can adjust medications, address vascular risks, plan for safety, and, when appropriate, start disease-modifying therapy that targets amyloid.
Think of it like smoke alarms. A reliable alarm does not put out fires by itself, but it tells you when to call the fire department and when to stop worrying. For millions of older adults, a simple blood draw can be that alarm.
How the new tests change the diagnostic pathway
Before 2025, a typical journey for a 68-year-old with mild memory complaints might look like this:
- Wait weeks for a neurology appointment.
- Receive screening and labs to rule out depression, thyroid problems, or vitamin deficiencies.
- Join a queue for a spinal tap or a positron emission tomography scan.
- Finally get a result that either rules in Alzheimer’s pathology or points elsewhere.
With mainstream blood testing, the pathway becomes shorter and more rational:
- Primary care orders a plasma p-tau assay during the initial workup.
- If the result makes Alzheimer’s pathology unlikely, the doctor pivots to other causes and addresses reversible risks. If it suggests pathology, the patient moves quickly to confirmatory testing and specialist care.
- When treatment is on the table, that confirmatory step can be tailored to local access and insurance, which today often means amyloid positron emission tomography or cerebrospinal fluid testing.
The practical effect is triage. Specialists spend more time with patients who likely need them. Primary care keeps ownership of cognitive health, just like it does for blood pressure and cholesterol.
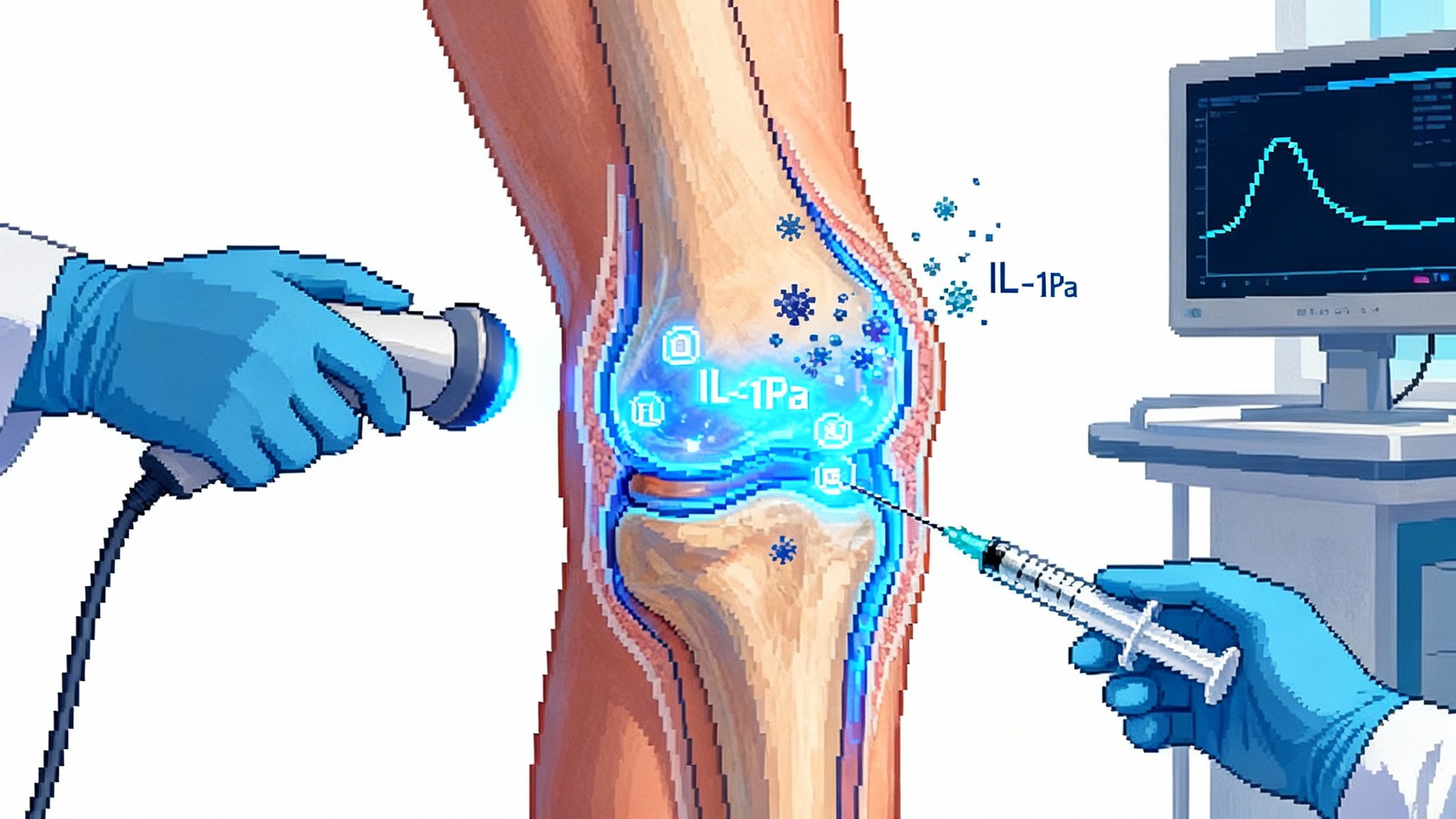
Faster access to disease-modifying drugs
The new Alzheimer’s drugs are not cures, but they matter. They slow decline in properly selected patients with early symptomatic disease and confirmed amyloid. Every month shaved from diagnostic delays is valuable time preserved for managing money, driving, and social life.
Blood tests help in three ways:
- Earlier flagging: Patients can be identified when symptoms are mild and potentially more responsive to treatment.
- Better targeting: People without Alzheimer’s pathology are spared time, worry, and side effects from treatments that will not help them.
- Smoother logistics: Programs that require evidence of amyloid can use a blood test as an efficient first filter before a confirmatory test.
For patients and families, the upshot is practical: less runaround, quicker answers, and a clearer path to therapy if it is appropriate.
What payers and health systems will do next
Coverage follows infrastructure. Three pieces are falling into place in 2025:
- Coding: New laboratory billing codes for phosphorylated tau and beta amyloid in plasma went into effect this year. That gives insurers standardized ways to reimburse these tests rather than treating them as miscellaneous.
- Prior authorization rules: Expect payers to require basic clinical documentation. Most will cover testing in adults over 55 with cognitive symptoms and without obvious reversible causes. Many will not cover screening in people without symptoms until stronger evidence emerges.
- Networks and volume: Large reference labs already run these assays. Health systems will decide whether to send-out to national labs or install platform analyzers in-house. The fastest path to scale is using the analyzers that hospitals already own for routine tests, which is exactly where some of the cleared assays run.
Costs matter. A blood-based workup is vastly less expensive than nuclear imaging and far easier to schedule. When used to rule out Alzheimer’s pathology in low-risk cases, the savings compound because fewer people proceed to costly confirmatory scans. Insurers understand that math. The result will be standard coverage in symptomatic adults within mainstream plans.
Guardrails: false positives, false negatives, and the art of pretest probability
No test is perfect. What changes with blood biomarkers is the balance of convenience and accuracy. Two rules can make or break results in practice:
- Test the right people. These assays are intended for adults with symptoms suggestive of cognitive impairment. Using them in people without symptoms will produce more false alarms, because the chance of disease is lower to begin with. A rule of thumb: your result is only as good as your reason for ordering the test.
- Interpret in context. A negative result in someone with mild complaints can be powerful. A positive result should be paired with a clinical exam and, when it would change treatment, a confirmatory test. That is not a burden; it is smart medicine that prevents mislabeling and over-treatment.
Think like a pilot reading multiple instruments. No single gauge decides whether to land. The combination points the way.
Data privacy and ethical use
Cognitive data is personal. Blood tests introduce results that could affect employment, driving, and family planning. There are concrete protections and practical choices to keep in mind:
- Medical data from clinical labs is protected by federal privacy law. Employers and insurers cannot simply pull lab results without authorization.
- Patients can choose where results are shared. If you want a second opinion, allow your records to be sent to the specialist. If you do not, you can keep them within your primary care system.
- Avoid casual testing. Self-directed or direct-to-consumer ordering without a clinician can create orphaned results that lack context and follow-up. These new assays are designed for clinician use. That is a feature, not a bug.
Health systems also have responsibilities. They should use de-identified analytics for quality improvement and maintain strict controls on who can access identifiable results. Clinicians should document the reason for testing, the counseling provided, and the next steps, so that results are not misinterpreted years later.
What about home sampling and population screening at 55 plus
Two next steps are already visible on the horizon:
- Home sampling: Researchers are evaluating whether dried blood spot cards or small-volume capillary draws can reliably measure p-tau217 outside the clinic. If stability and accuracy match venous samples, expect home kits supervised by clinicians. That would push testing into pharmacies and living rooms.
- Population-level screening at 55 plus: Because the new tests are low-cost and scalable, some health systems will pilot age-based screening in primary care, much like colon cancer scanning at 45. The case for this will depend on two questions: does early detection change outcomes in asymptomatic people, and do the benefits outweigh anxiety and downstream testing. Expect careful, phased pilots tied to research registries before any broad rollout.
Both directions are promising, but should be done inside guardrails. A home kit is only useful if the system catches people with worrisome results and gets them into care. Screening only makes sense if it leads to better function over time, not just more labels.
Blood biomarkers as surrogate endpoints: speeding prevention trials
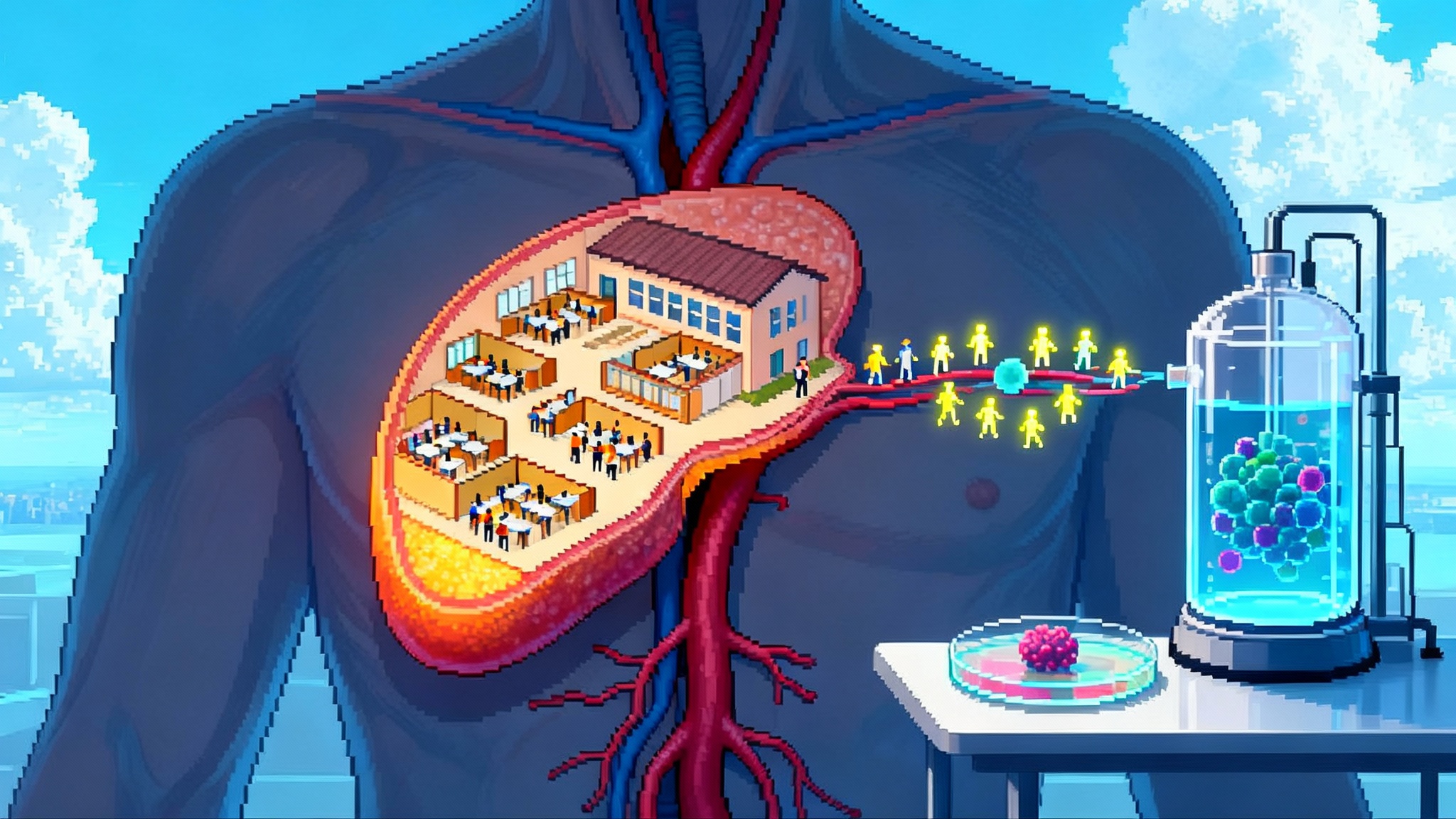
The biggest win from mainstream blood testing may be research. Trials that used to take years and thousands of participants can be done faster when a blood marker stands in, at least in early phases, for expensive scans or invasive procedures.
For prevention studies, that means three advantages:
- Recruitment: Identify at-risk participants earlier and at scale through primary care networks.
- Enrichment: Enroll people whose blood markers indicate active amyloid or tau biology so that a preventive therapy has a fair test. For a related prevention frontier, see the 2025 thymus reset race.
- Early readouts: Use changes in p-tau or related markers as early signals of biological effect, then follow with clinical outcomes.
Regulators have frameworks for surrogate endpoints and will continue to require that biomarkers connect to real-world function. That is the right bar. The practical effect is still major: a world where true prevention trials are faster to start and faster to finish.
The rollout playbook for health systems
If you run a clinic or a health plan, here is a simple blueprint:
- Define who can order: allow internists, geriatricians, and neurologists to order plasma p-tau tests for adults 55 and older with cognitive symptoms.
- Build a reflex pathway: negative results trigger risk-factor management and follow-up in primary care; positive or indeterminate results trigger referral to cognitive clinics and confirmatory testing.
- Standardize consent language: include a one-page explanation that results are part of a larger assessment and may prompt further testing.
- Track equity: measure who is getting tested by age, sex, race, zip code, and language to avoid unequal access.
- Integrate billing: use current codes, avoid miscoding as experimental, and publish patient cost estimates up front.
These steps reduce friction and keep testing useful rather than noisy.
What individuals and families can do now
- If you are 55 or older and notice new problems remembering recent events, ask your primary care clinician whether a blood-based workup is appropriate.
- Bring a spouse or friend to describe changes they see at home, which can be more telling than a five-minute memory screen.
- If a blood test is negative, do not stop there. Use the visit to address sleep apnea, hearing loss, blood pressure, diabetes, exercise, and medication side effects, all of which affect brain health. For a cardiovascular parallel on preventive blood tests, see how Lp(a) siRNA resets heart aging.
- If a blood test suggests Alzheimer’s pathology, ask about confirmatory testing and whether you might be a candidate for disease-modifying therapy. Also ask about the plan to monitor safety.
Small, practical steps taken early matter more than heroic measures taken late.
The bottom line
In 2025, Alzheimer’s blood tests moved from research posters to routine ordering. The first clearance established that a simple blood draw can reliably signal Alzheimer’s biology in the right patients. The primary care indication opened the front door for large-scale triage. Together, they promise earlier clarity, more targeted use of new therapies, and a faster path to prevention science.
There is real work ahead on coverage details, data privacy, and avoiding overuse in people without symptoms. But the direction is set. Cognitive aging is finally getting the same playbook that transformed heart disease, where cheap, scalable blood tests moved the system from guesswork to measurement.
That is the inflection point. The decade ahead will be defined by how well we use it.