Lp(a) Revolution: One dose siRNA could reset heart aging
In March 2025, a single injection of Eli Lilly’s lepodisiran cut lipoprotein(a) by about 94 percent and kept it low for a year or longer. Here is how Lp(a) screening and long-interval siRNAs could become cardiology’s next prevention lever, plus the path to outcomes and coverage.

Breaking through a stubborn risk factor
On March 30, 2025, cardiology got a glimpse of a different future. In a multinational phase 2 trial presented at the American College of Cardiology meeting and published the same day, a single injection of Eli Lilly’s lepodisiran cut lipoprotein(a) by about 94 percent and kept it low for a year or more. The longest follow up showed durable reductions beyond one year with mild injection site reactions. These are not incremental improvements. They look like a new control knob on cardiovascular aging. See the NEJM lepodisiran phase 2.
If that signal holds through outcomes trials, lipoprotein(a) testing plus long-interval small interfering RNA therapy could sit alongside statins and glucagon-like peptide 1 drugs as a standard prevention trio. That sounds ambitious, so let’s ground it in what Lp(a) is, why it matters, what exactly siRNA is doing inside the liver, and what stands between today’s data and tomorrow’s routine care. For broader context on vascular aging, see arteries as aging's command hub.
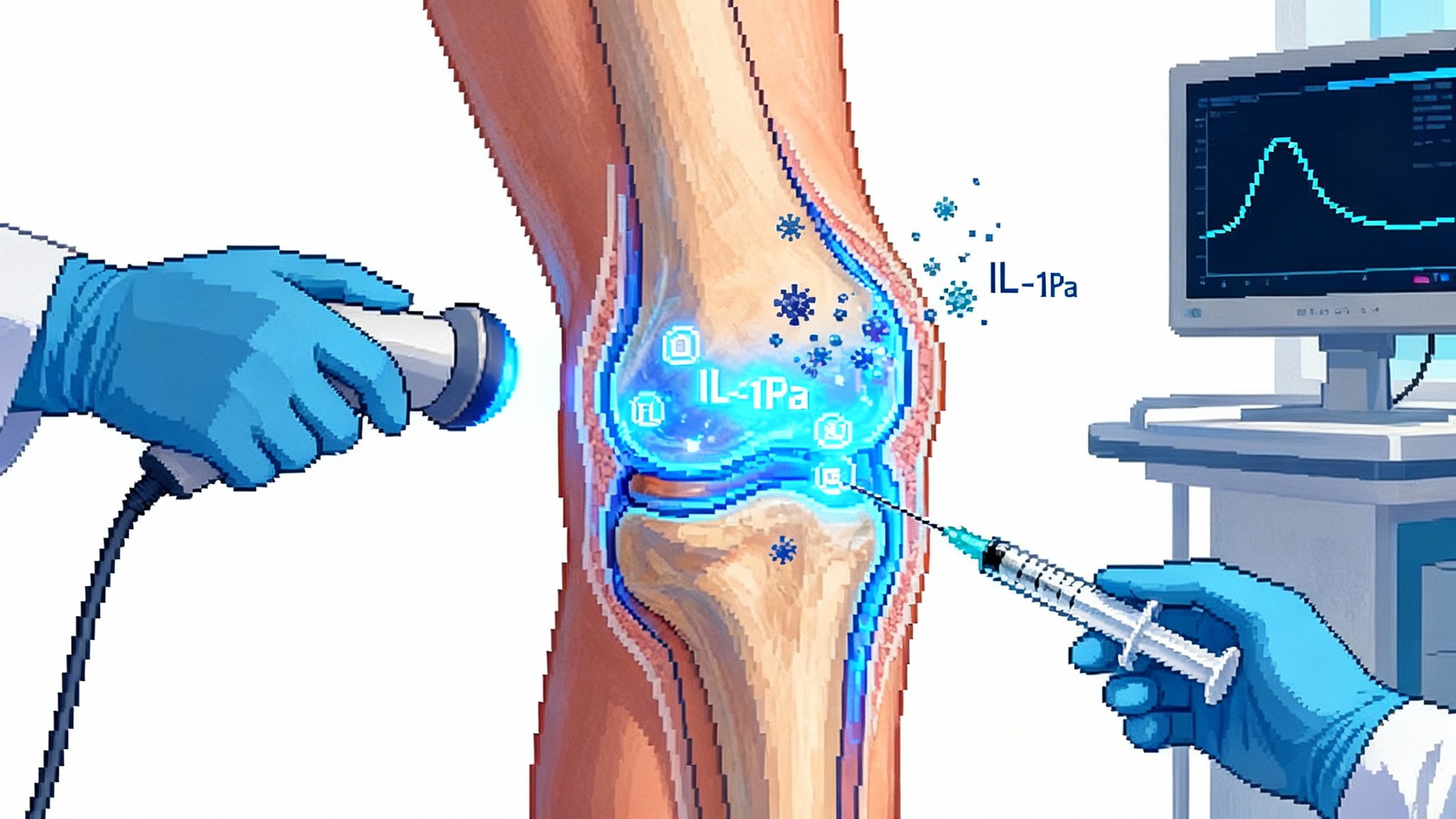
Lp(a) in plain English
Lipoprotein(a), often written as Lp(a), is a cholesterol-carrying particle that behaves like rust and glue at once. It carries oxidized phospholipids that irritate artery walls and a tail called apolipoprotein(a) that can amplify clotting. High levels raise the risk of heart attack, stroke, and calcific aortic valve stenosis even when low-density lipoprotein looks fine.
Two facts make Lp(a) different from the cholesterol we have managed for decades:
- It is mostly set by your genes and stabilizes early in life. Diet and exercise barely nudge it.
- Routine lipid panels do not include it. You must ask for a specific blood test, typically reported in nanomoles per liter. A common high-risk threshold is 125 nanomoles per liter or higher.
Think of Lp(a) as a silent, inherited accelerator pedal on vascular wear and tear. Many people do not feel anything until a first event. That is why testing matters and why long-acting therapies are attractive. You want to identify the people with that hidden accelerator and then keep a foot on the brake for years at a time.
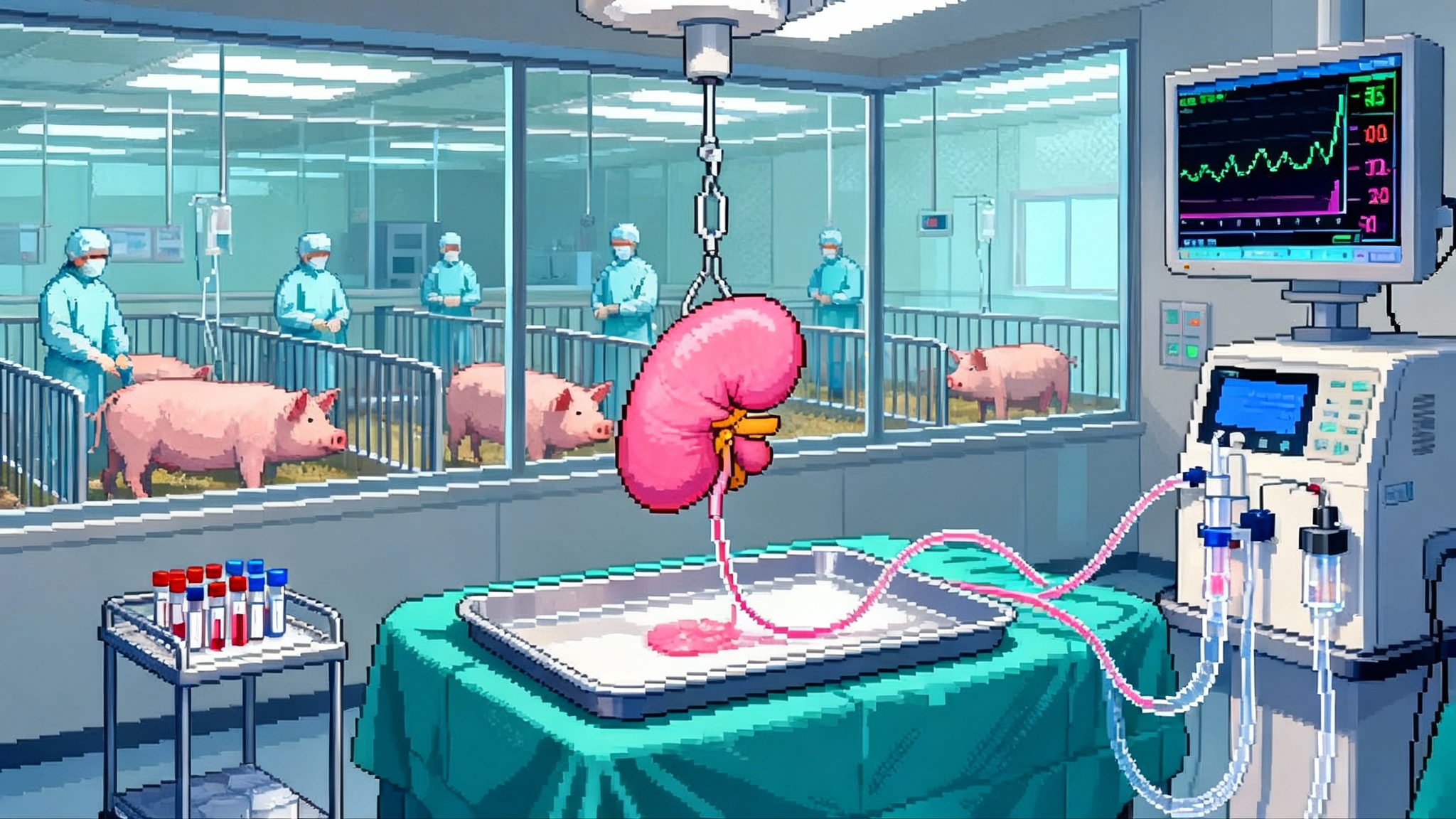
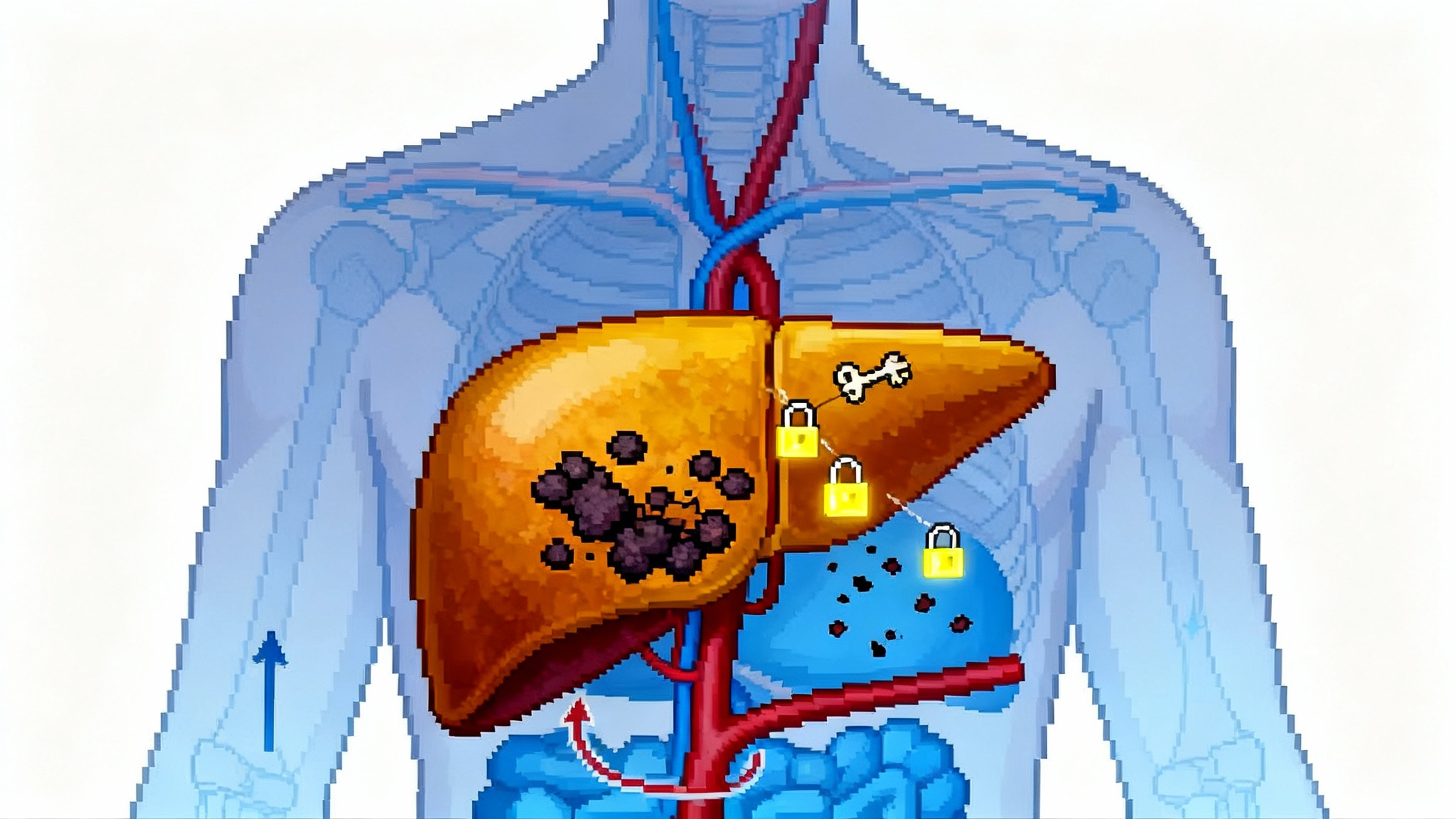
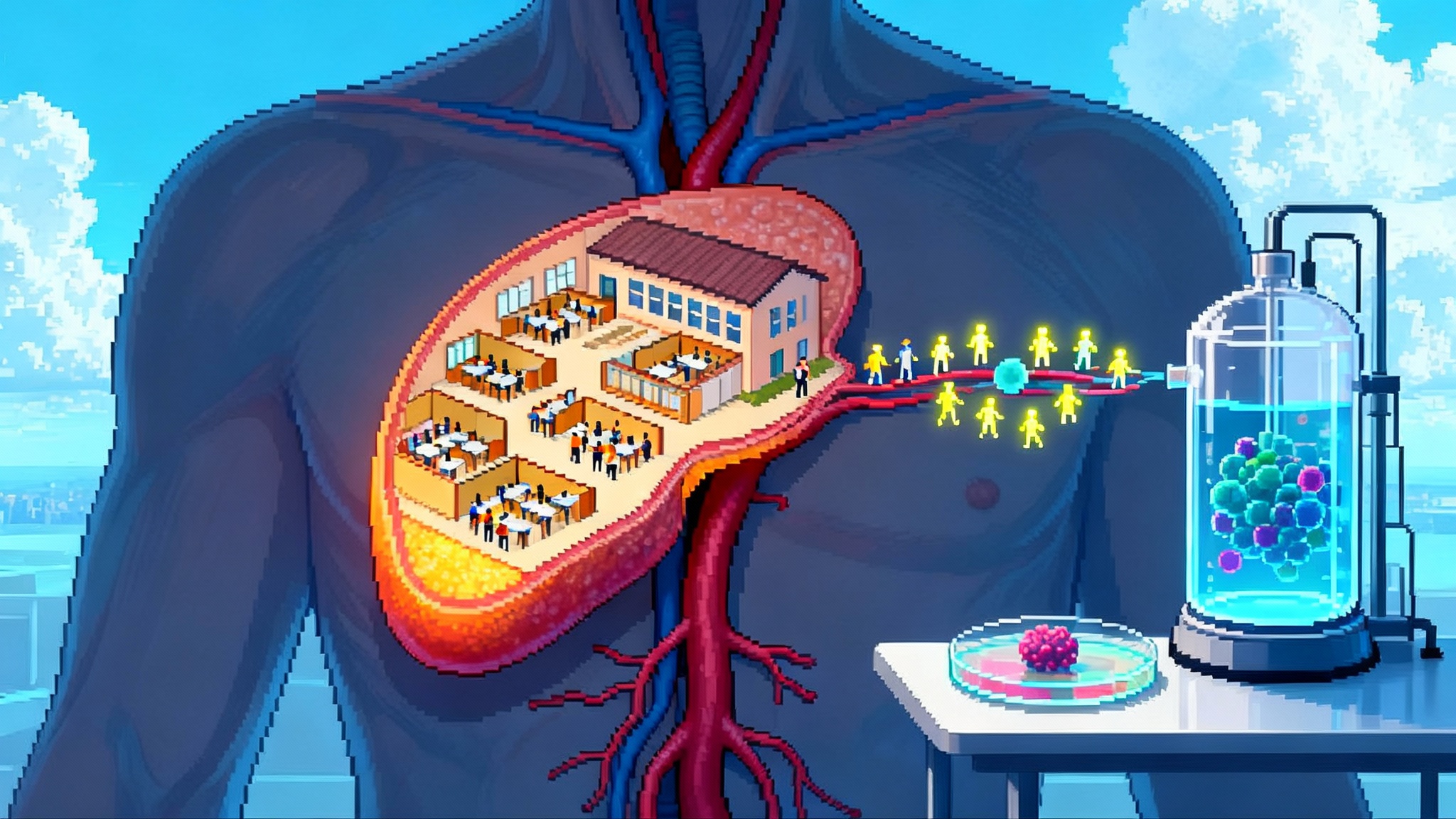
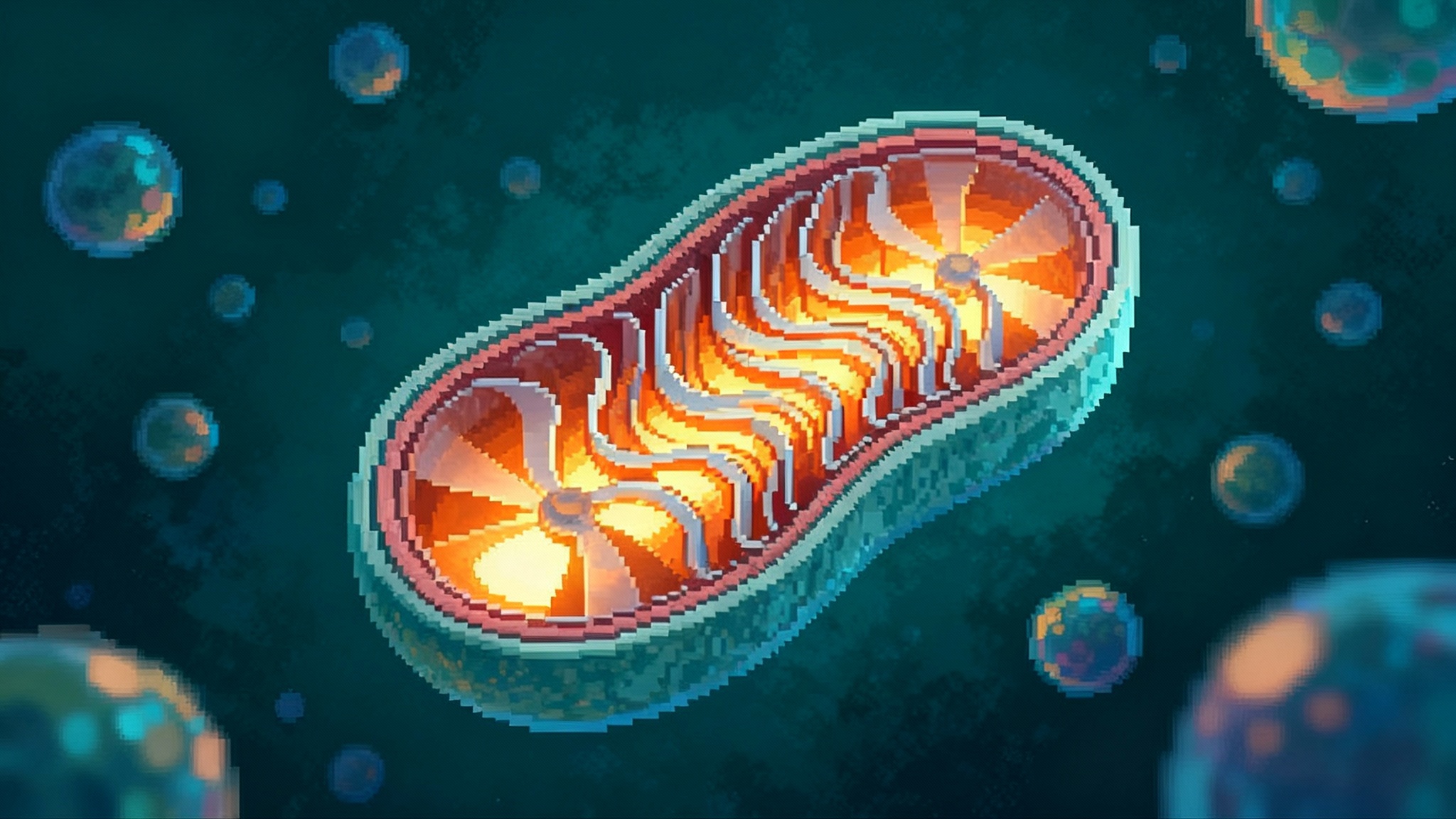
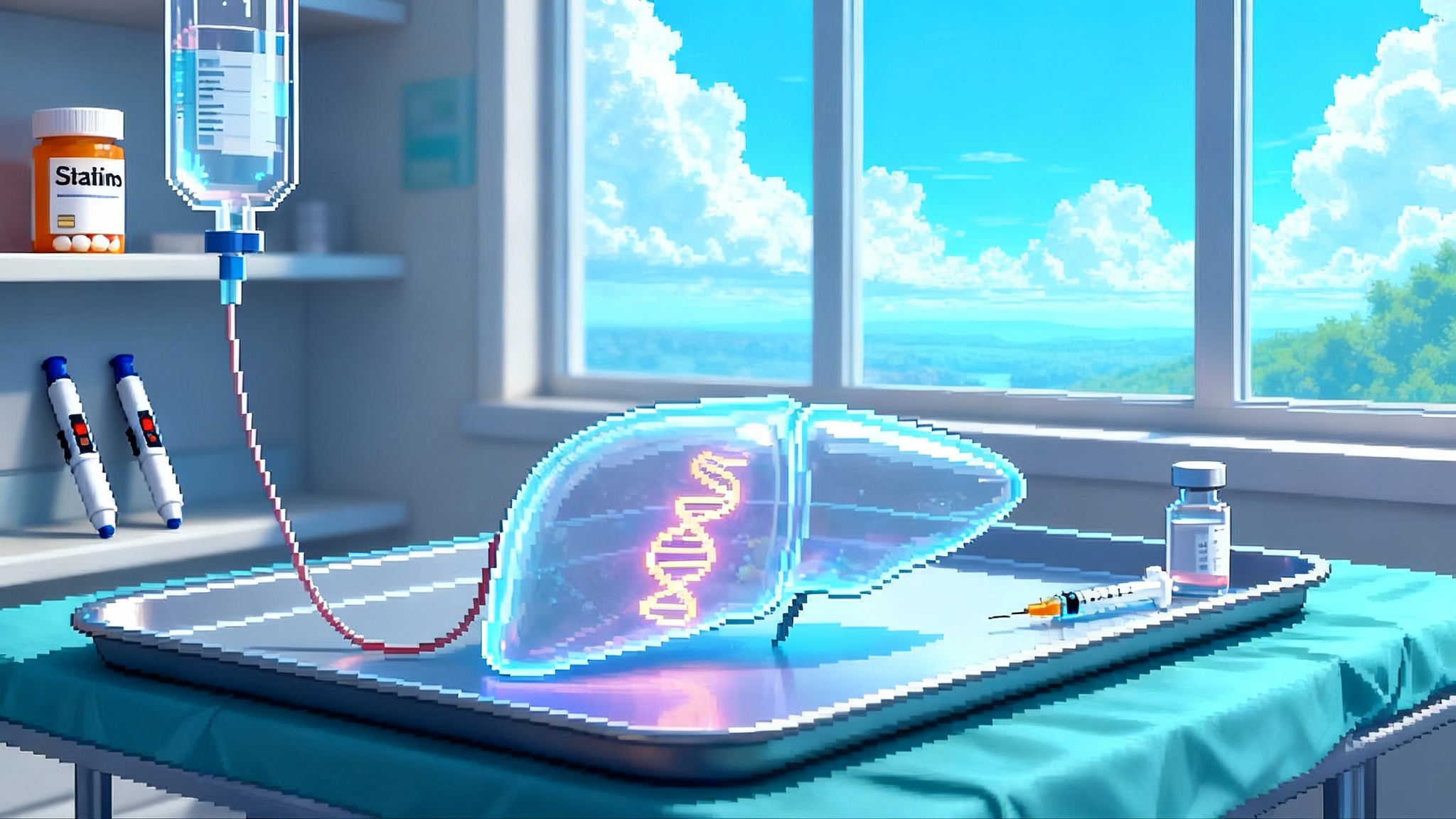
What siRNA does inside the liver
Small interfering RNA therapies work like a precise mute button for a single instruction sheet in a factory. In this case, the factory is the liver. The instruction sheet tells hepatocytes how to build apolipoprotein(a), the core of Lp(a). The siRNA is packaged with a sugar tag that guides it to the liver, enters the cell, and recruits a protein complex that shreds the matching message. Fewer messages mean less apo(a), which means less Lp(a) released into the bloodstream.
The magic is not just potency. It is duration. Because the liver keeps reusing that shredding complex, the muting effect lasts for months. With lepodisiran, one injection at the highest tested dose dropped Lp(a) dramatically and stayed effective through a year and beyond in many participants. That opens the door to annual or twice-yearly dosing. Patients who can remember two dates a year for an injection are far more likely to stay on therapy than those who must remember a pill every day.
Meet the front-runners
-
Lepodisiran by Eli Lilly: a long-duration siRNA with phase 2 data showing roughly 94 percent average reductions in Lp(a) over weeks 8 to 26 after a single high dose, and sustained reductions over a year in many participants. A large outcomes program is moving forward.
-
Olpasiran by Amgen: a quarterly or twice-yearly siRNA that in phase 2 drove deep Lp(a) reductions and maintained meaningful effects long after dosing stopped in extension follow up. A global outcomes trial called OCEAN(a)-Outcomes began in 2022 with event-based endpoints; many sites list an estimated primary completion in late 2026, with readout likely to follow. You can scan the OCEAN(a) Outcomes trial record for core details.
-
Zerlasiran by Silence Therapeutics: an siRNA with phase 2 data showing more than 80 percent time-averaged reductions across dosing regimens and maximum drops near 90 percent, with infrequent injections. Phase 3 planning is underway.
These three share a design principle: target apo(a) production in the liver, achieve deep knockdown, and stretch dosing intervals so adherence becomes the default. Their differences center on dose, interval, and the fine points of chemistry that determine how long the mute button stays pressed.
How this could change prevention in practice
Statins made LDL the first lever. Glucagon-like peptide 1 drugs are now bending weight and glycemia curves. An Lp(a) lever does something the others cannot. It removes a genetically programmed signal that makes arteries more inflammatory and more thrombosis-prone regardless of LDL.
Here is how care could look within a few years if outcomes trials are positive:
-
Everyone gets one Lp(a) test in early to midlife. That could be at a first cholesterol screen in your 30s or at a midlife exam by your primary care physician or obstetrician-gynecologist. The result is durable for most people and guides how aggressively you manage other risks.
-
If your Lp(a) is elevated, you get two care packages. First, you intensify today’s tools: optimize LDL lowering with a high-intensity statin, add ezetimibe or a PCSK9 pathway agent if needed, control blood pressure, and treat sleep apnea, smoking, and metabolic disease. For perspective on the pipeline, see PCSK9 base editing advances. Second, you schedule long-interval Lp(a) therapy when it becomes available, likely once or twice per year in a clinic.
-
Families use cascade testing. If you have very high Lp(a), first-degree relatives get tested once as well. Primary care and cardiology clinics can automate this with electronic health record prompts and patient messages.
The net effect is a shift in the prevention curve. You identify a fixed, inherited driver that standard panels miss and you turn it down for years with minimal friction.
Timelines: when preventive cardiology might get a new lever
-
2025: The lepodisiran phase 2 results established the durability story and sparked broad interest. An outcomes program is underway. In parallel, the antisense oligonucleotide pelacarsen, which also targets Lp(a) production, has a large phase 3 outcomes trial with results anticipated around 2025. Those results are important because they can validate the idea that lowering Lp(a) reduces cardiovascular events.
-
2026 to 2027: OCEAN(a)-Outcomes for olpasiran is event driven and many public listings show an estimated primary completion by late 2026. Allow time to adjudicate events, analyze, and publish. A 2027 readout is plausible. If positive, this would give the first siRNA outcomes proof.
-
Late decade: Lepodisiran’s long-interval profile could become highly attractive once outcomes data exist for the class and for the program itself. If the class effect is validated and safety remains favorable, annual or twice-yearly dosing is positioned to scale.
Why the caution on dates? Cardiovascular outcomes trials are controlled by nature and statistics. Event rates, background therapy, and post-pandemic care patterns can speed or slow the clock.
FDA and payer hurdles that matter
Two questions decide how fast patients feel the benefit.
-
What counts as proof of benefit? Regulators want to see that lowering Lp(a) prevents heart attacks, strokes, and revascularizations. That is why outcomes trials are the gatekeepers. Surrogate approval that relies on Lp(a) lowering alone would require the Food and Drug Administration to accept Lp(a) as a surrogate reasonably likely to predict clinical benefit. Given the agency’s recent tightening of accelerated approval expectations, sponsors are building robust confirmatory trials from the start.
-
Who pays, for testing and for therapy? The laboratory test already exists and uses a standard billing code. Many plans cover it when there is a clear clinical reason, but policies vary and some insurers treat Lp(a) measurement as investigational outside specific scenarios. Expect payer coverage to expand if outcomes data are positive and if diagnostics improve standardization. Roche, for example, is advancing an assay calibrated in nanomoles per liter that can be deployed on widely used analyzers. That kind of standardization helps payers write simple rules and helps clinicians manage thresholds consistently.
Practical takeaway for clinics right now: add Lp(a) to secondary prevention order sets and to midlife wellness panels, document the indication in the note, and be prepared to appeal if a claim is denied. For the first wave of Lp(a) drugs, expect coverage criteria that mirror the outcomes populations, for example established atherosclerotic disease plus an Lp(a) above a fixed threshold.
How to act on a result today
While we wait for outcomes data, an Lp(a) value should still change care. For a 52-year-old woman with a family history of heart attack who carries an Lp(a) of 210 nanomoles per liter and an LDL of 92 milligrams per deciliter:
-
Raise the intensity of LDL lowering now. A high-intensity statin with a goal of well below 70 milligrams per deciliter is reasonable. If the response is suboptimal, add ezetimibe or consider a PCSK9 pathway drug. Lower apoB lowers event risk regardless of Lp(a).
-
Address metabolic risk early. If body mass index and glycemia are elevated, a glucagon-like peptide 1 receptor agonist can reduce weight and events in high-risk patients while we await Lp(a)-specific therapy.
-
Plan follow up. Recheck apoB and LDL in 8 to 12 weeks, and revisit blood pressure, sleep, and exercise. If and when an Lp(a) siRNA is approved, the patient is already optimized and ready for the next lever.
-
Encourage family screening. Her adult siblings and children can test once, which may reveal hidden risk and prompt earlier prevention.
What health systems and employers can do
-
Build an Lp(a) order into routine adult preventive labs at age 35 to 45 and into all cardiology new patient templates. One checkbox makes a durable difference.
-
Add Lp(a) prompts in electronic health records for any admission with myocardial infarction or ischemic stroke. Measure on admission and recheck at follow up.
-
Create a navigator script for abnormal results. Patients should leave with a clear plan for LDL lowering, blood pressure control, and family testing.
-
Prepare pharmacy and benefits teams for long-interval RNA therapies. Logistics look similar to inclisiran and other clinic-administered agents. Scheduling two dates per year is operationally simple.
-
Set up employer wellness coverage for Lp(a) testing. The cost is modest relative to imaging and procedures. Early identification can prevent both human and financial loss.
The competitive and clinical landscape, in one page
-
Mechanism: all three siRNAs mute apo(a) production in the liver with conjugates that deliver the drug to hepatocytes. The result is deep knockdown and long intervals.
-
Dosing: olpasiran has been studied at every 12 to 24 weeks, zerlasiran every 16 to 24 weeks, lepodisiran may be annual or twice-yearly at higher doses once programs mature.
-
Safety: the class profile so far shows mostly mild injection site reactions. Monitoring of liver enzymes continues, as a few participants had transient elevations in trials. No consistent systemic signal has emerged to date, but long-term follow up is crucial.
-
Outcomes: pelacarsen will likely be first to answer the big question in 2025. OCEAN(a)-Outcomes could follow, then lepodisiran’s program. Sequence matters for regulatory decisions and for payer confidence.
-
Diagnostics: assays calibrated in nanomoles per liter are becoming more common. Harmonized reporting reduces confusion and supports clear risk thresholds.
The longevity angle without the hype
Longevity is not magic. It is cumulative risk management that adds functional years. Lp(a) siRNAs fit that philosophy because they are precise, durable, and easy to adhere to. They do not replace statins or glucagon-like peptide 1 drugs. They add a new, independent control that matters most in people who look good on standard labs but carry a genetic spark for premature disease. This complements adjacent work such as anti-CH strategies for healthspan.
Universal or near-universal Lp(a) testing in midlife is the practical step that moves this from headlines to outcomes. It finds high-risk people early, it justifies deeper LDL and blood pressure control now, and it lays the runway for once- or twice-yearly silencing when approvals come.
What to watch next
-
The pelacarsen outcomes verdict, expected around 2025, which will influence regulators and payers.
-
The pace of OCEAN(a)-Outcomes event accrual and any interim safety updates, with a primary completion widely listed as late 2026.
-
Confirmation of lepodisiran’s dosing schedule in phase 3 and clarity on its outcomes timeline.
-
Diagnostic advances that push laboratories to report in nanomoles per liter across the board.
-
Payer policies that move from investigational to covered test status for broad adult screening as evidence consolidates.
A smart finish
A generation ago, we learned how to turn down LDL and saved millions of lives. In the last few years, we began to turn down obesity and diabetes with drugs that patients actually stay on. Lp(a) siRNA looks like the next lever: not a cure, but a durable, targeted way to take pressure off the vascular system for years at a time. The path from a phase 2 graph to everyday practice runs through outcomes readouts, Food and Drug Administration decisions, and payer contracts. The step you can take now is simple and powerful. Add one Lp(a) test to midlife care and, when the result comes back, use it to tighten the rest of the plan. That is how breakthroughs in journals become longer, healthier lives in clinics.