PCSK9 base editing and primary prevention rewrite LDL care
Two signals in 2025 mark a new era in cholesterol care. AHA VESALIUS-CV shows PCSK9 inhibitors prevent first cardiovascular events, and early Heart-2 data for VERVE-102 suggests single-infusion, durable LDL reductions following Lilly’s Verve acquisition.
November 2025 locked the pivot
At the American Heart Association Scientific Sessions on November 8, 2025, the VESALIUS‑CV trial delivered what prevention experts have chased for decades. In high‑risk adults without a prior heart attack or stroke, adding the PCSK9 inhibitor evolocumab to intensive background therapy reduced first major events. The headline numbers matter. Over a median of 4.6 years, risk fell by 25 percent for the composite of coronary heart disease death, heart attack, or ischemic stroke, and by 19 percent for the broader composite that also included revascularization. Low‑density lipoprotein cholesterol, usually shortened to LDL‑C, dropped by about 55 percent to a median of 45 mg/dL at 48 weeks, and stayed low. The American Heart Association’s summary is clear that this is primary prevention evidence, not just another secondary prevention victory. That is a line in the sand for how early we act on cholesterol exposure in people at elevated risk. See the AHA VESALIUS‑CV press summary for the core results and context.
Earlier in 2025, Eli Lilly closed its acquisition of Verve Therapeutics on July 25, 2025, bringing in vivo base editing for LDL control into the portfolio of a company that already reshaped metabolic medicine. Lilly’s press release framed the transaction as a path to one‑time cardiovascular risk reduction. Verve’s Heart‑2 study of VERVE‑102, a single‑infusion base editor that turns off PCSK9 in the liver, reported dose‑dependent LDL‑C reductions with a mean drop of about 53 percent and a maximum around 69 percent in early cohorts, with a clean safety profile to date. With primary prevention proof for the PCSK9 target and credible one‑time editing data in hand, the pivot is locked: durable LDL control moves from theory to plan. See Lilly completes Verve acquisition for details.
From lifelong refills to edit once
Imagine LDL exposure as water filling a bathtub over time. You can open the drain a bit with healthier food, exercise, and weight control. Statins open the drain more by slowing the faucet at its source. PCSK9 inhibitors open an additional drain by preventing the liver from recycling the LDL receptor, so more receptors stick around and pull LDL from the blood. Small interfering RNA therapies such as inclisiran nudge the liver to make less PCSK9, so the same drain stays open longer. Base editing, by contrast, is the plumber replacing a pipe segment. With one precise change to the PCSK9 gene in liver cells, the body permanently makes much less PCSK9, which keeps LDL receptors on duty. The outcome looks similar on a lab report, lower LDL‑C, yet the mechanisms and durability are very different.
This shift echoes a broader move toward durable genetic tools, as covered in mitochondrial editing’s 2025 leap.
Primary prevention proof resets the timing
VESALIUS‑CV matters because it shifts the conversation from rescuing survivors to preventing first events. The participants were older on average and high risk, many with atherosclerotic cardiovascular disease in non‑event forms or with high‑risk diabetes. Yet the logic scales down the age curve when you think in terms of lifetime exposure rather than a single lab value.
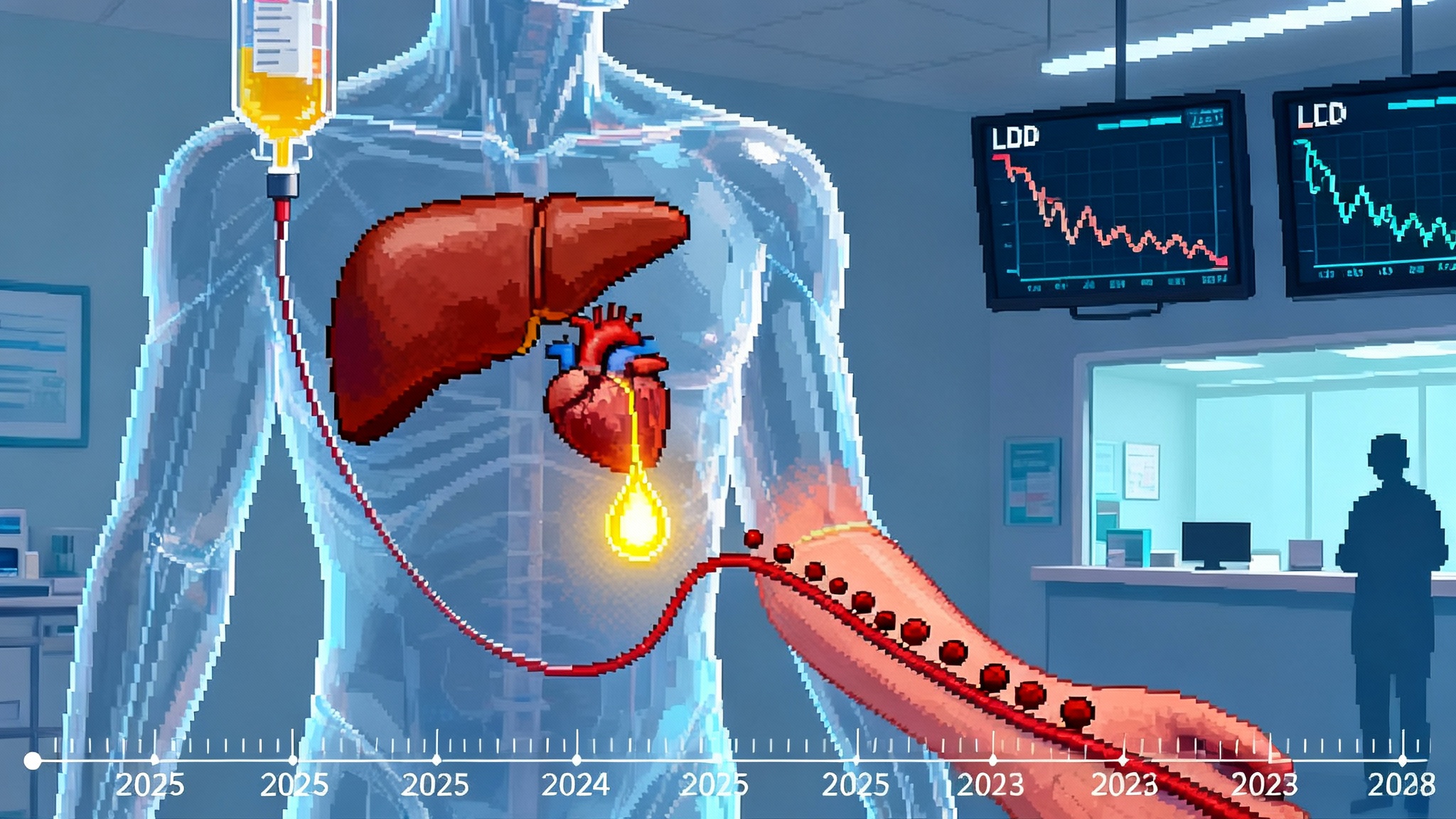
A helpful way to frame this is the LDL‑years model. Each year you spend with LDL‑C at 120 mg/dL adds more to arterial plaque than a year at 60 mg/dL. Two people can have the same LDL‑C at age 60 and very different plaque loads because one ran high in their 30s and 40s. Primary prevention proof says that if we lower LDL‑C earlier and keep it low, we are likely changing the area under the LDL‑time curve, not just the number on a given day. That is longevity in plain math. For a complementary risk lens, see why CHIP is the new LDL.
What this means for screening in the 20s, 30s, and 40s
- Start earlier, repeat smartly. A first lipid panel in the late teens or early 20s sets a baseline, and a second panel in the late 20s confirms trajectory. By the mid‑30s, add apolipoprotein B when available. If levels are stable and low risk, recheck every 4 to 6 years. If levels are borderline, recheck every 2 to 3 years.
- Measure lipoprotein(a) once. Lipoprotein(a), often written as Lp(a), is largely genetically set and adds risk independent of LDL‑C. One lifetime measurement in early adulthood, with earlier measurement for those with family history of premature coronary disease, identifies a group who may need more aggressive LDL‑C goals.
- Add polygenic risk where it changes the plan. Polygenic scores for coronary disease are not perfect, but they are useful when combined with traditional risk factors. A high score plus high Lp(a) plus elevated LDL‑C in someone in their 30s suggests earlier medication to shrink lifetime exposure.
- Map family history like a pedigree. Ask about heart attacks, angina, and strokes before age 55 in men and 65 in women. If present, test earlier and consider familial hypercholesterolemia work‑up.
The goal is not to put young adults on injections. The goal is to identify those who will bank the most years of healthy arterial life by reaching and maintaining lower LDL‑C earlier.
Payer economics of edit once versus pay forever
Health economics will decide how fast one‑time LDL control moves from specialty centers to routine primary care. The logic is straightforward, even if the spreadsheets are complex.
- Adherence is the hidden tax. Statins work, but long‑term adherence in the real world is modest. Even with copay support, chronic injectables are hard to keep on schedule for years. Every missed refill erodes the benefit. A one‑time therapy does not leak value through missed months.
- Price versus duration. Consider a simple model. A person at high risk needs LDL‑C reduction beyond statins for 20 years. If the annual net cost of a chronic PCSK9 therapy is a few thousand dollars per year, total drug cost over 20 years easily exceeds tens of thousands of dollars, not including administration visits and lost time. A one‑time therapy with durable effect could be priced against that stream. If durability is 15 to 20 years, payers can compare a known total against a likely total that depends on adherence and price changes.
- Outcomes warranties and installment payments make sense here. Gene therapies for rare diseases pioneered pay‑over‑time and outcomes‑based contracts. The same instruments can apply to common diseases if the clinical benefit is clear. A warranty that refunds part of the price if LDL‑C does not stay below a contract threshold, measured at defined intervals, aligns incentives.
- Event avoidance is the real savings. Preventing one heart attack or stroke avoids hospital stays, procedures, rehab, and lost productivity, often six figures in acute and downstream costs. If the combination of primary prevention proof and durable LDL‑C lowering shifts first events to never, the value is large even before adding quality of life.
None of this sets a price. It does outline how employers, insurers, and public payers can model break‑even points now, then update when longer‑term durability and safety data arrive.
A pragmatic 2026 to 2028 adoption roadmap
- 2026: Build the pipes. Academic medical centers and large integrated systems establish lipid clinics that can evaluate candidates for durable LDL‑C lowering. Electronic health record prompts flag patients with LDL‑C above 100 mg/dL on maximal statin plus ezetimibe, or above 130 mg/dL with high‑risk diabetes, or anyone with heterozygous familial hypercholesterolemia. Primary care practices standardize early lipid panels, Lp(a) once in a lifetime, and optional polygenic risk where available. Payers pilot outcomes‑linked contracts for chronic PCSK9 therapy in primary prevention populations identified by VESALIUS‑CV criteria, while tracking adherence and event rates prospectively.
- 2027: Expand criteria in controlled steps. As single‑infusion LDL editing advances through phase 2 and into phase 3, systems create eligibility review boards that include cardiology, lipidology, genetics, and ethics. The first non‑familial hypercholesterolemia candidates are adults with high‑risk diabetes or subclinical atherosclerosis on imaging who fail to reach LDL‑C targets with chronic therapy. Employers add cardiovascular risk reduction packages that combine obesity care, sleep apnea management, and durable LDL‑C control for those who qualify.
- 2028: Integrate into primary care workflows. If durability and safety hold, payer coverage expands to defined high‑risk primary prevention groups. Referral flows become routine, much like bariatric and structural heart pathways today. Pharmacy benefit managers and health systems align on lab schedules for sustained LDL‑C verification at six months, one year, and annually. Patient education materials explain the edit‑once approach in plain language, including options for future pregnancy and reversible contraception timing where relevant.
Throughout this period, real‑world registries should track outcomes, especially in groups often under‑represented in trials. Data here is not decoration, it is the backbone of policy.
Safety, ethics, and what still needs to be proved
- Durability and reversibility. We expect edits to persist as long as the edited liver cells live. That is the point. It also means there is no off switch. Clear consent and robust pre‑treatment counseling are mandatory.
- Off‑target edits. Modern base editors are precise, and early human data from VERVE‑102 has been reassuring, yet only multi‑year follow‑up and deep sequencing will settle the question. Independent assay labs and open registries will build confidence.
- Immune reactions and re‑dosing. Lipid nanoparticles are familiar from vaccines, but gene editing payloads can trigger immune responses. If rare serious events emerge, we need clear protocols and transparent reporting.
- Special populations. Pregnancy, children, and very old adults will require careful thought. For now, expect initial use in adults who are clearly high risk with much to gain from durable LDL‑C lowering.
Bioethics here is practical. We already accept lifelong change when we implant valves or stents. Edit‑once LDL control changes a molecule rather than a metal, yet the standard is the same. Inform, consent, measure, and publish.
How primary care can act now
- Make lifetime LDL‑C visible. Add an LDL‑years graphic to the chart, a simple running tally of exposure that starts at first lipid panel. This reframes the conversation from one lab result to lifetime trajectory.
- Standardize a prevention bundle. Three items for anyone 20 to 40, timed to major life events like college entrance or first pregnancy planning: fasting lipid panel with apolipoprotein B if available, one Lp(a) measurement, and a risk review that includes family history and optional polygenic score if it will change decisions.
- Treat the person in front of you, not an average. If a 32‑year‑old has LDL‑C of 160 mg/dL, high Lp(a), and a father with a heart attack at 48, consider earlier medication and closer follow‑up. If someone has LDL‑C of 90 mg/dL, no family history, and a low polygenic score, celebrate and emphasize sleep, diet, and activity.
- Build a short list of referral triggers. Examples include LDL‑C above 130 mg/dL despite statin and ezetimibe, confirmed heterozygous familial hypercholesterolemia, Lp(a) above a high threshold with subclinical plaque on imaging, or inability to adhere to chronic injections in a high‑risk patient.
- Prepare for shared decisions about durability. Patients should be able to compare statins, twice‑yearly small interfering RNA, every‑two‑week monoclonal antibodies, and single‑infusion editing on one page. Include expected LDL‑C reduction, monitoring needs, side effect profiles, and cost model options.
What individuals can do this year
- Get a baseline. If you are 20 to 40, ask for a lipid panel and one Lp(a) test. If you have a strong family history, do it sooner.
- Think in decades. A lower LDL‑C for longer is better than a perfect LDL‑C for a short burst. Small and steady beats sporadic perfection.
- Ask about your mix of options. Some people will do well on lifestyle plus a generic statin. Others will need additional help. If you already take chronic injections, ask how primary prevention data changes your goals.
What employers and payers can pilot
- Offer a prevention benefit that funds early screening and adherence support. Put dollars behind the first two decades of exposure.
- Test outcomes‑based contracts now. Tie payment for chronic PCSK9 therapy to sustained LDL‑C thresholds and event rates in defined primary prevention cohorts. Use that experience to design future contracts for durable therapies.
- Stand up a registry with de‑identified data. Track lipid levels, adherence, events, and costs across your population. Publish what you learn.
The signal for healthspan
Longevity is often described in years added at the end of life. Healthspan asks a better question. How many years can a person expect to live free of vascular disease that limits everything else. The combination of primary prevention proof for PCSK9 inhibition and credible single‑infusion editing puts healthspan on a more predictable footing. We can lower LDL‑C earlier, we can keep it there reliably, and we can direct the most durable tools to those who will benefit the most. For more on metabolic damage that accumulates with time, see anti‑glycation enters trials.
There is work ahead. Regulators will weigh longer follow‑up. Clinicians will refine who gets which tool first. Payers will test contracts that pay for outcomes rather than refills. Patients will decide what permanence means for them. Yet the direction is now set. The one‑shot LDL decade has begun, and with it comes a practical chance to bend the curve of cardiovascular risk across a lifetime.
The smartest conclusion is the simplest one. If you control exposure, you control risk. 2025 gave us the proof of principle and the instrument to make it stick. The task for 2026 to 2028 is to build the pathways so that primary care, cardiology, and public health can use it well. When the pipes are in place, the bathtub does not overflow.