Mitochondrial Editing’s 2025 Leap to Injectable Care
Mitochondrial base editing moved from clever biology to an injectable therapeutic candidate in 2025. See the new editors, in vivo delivery data, and a pragmatic first-in-human plan aimed at aging tissues.
The year mitochondria stopped being off limits
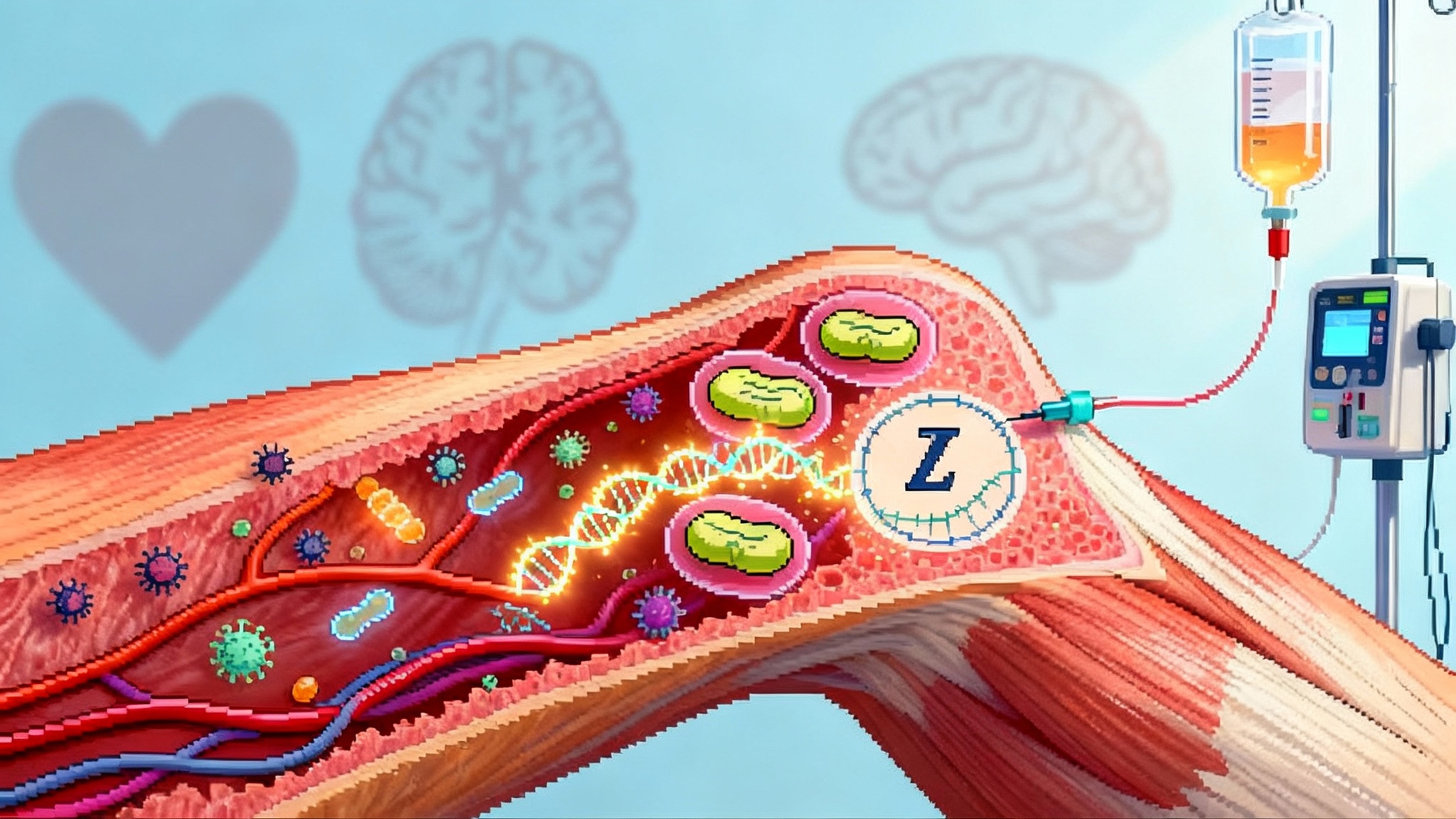
For a decade, mitochondrial DNA sat apart from the gene editing revolution. Guide RNAs could not reach the organelle. Double‑strand breaks risked catastrophic deletions. Most teams treated the mitochondrial genome like a museum artifact behind glass. That changed in 2025. Two results moved the field from clever cell biology to something that looks like modern medicine: clearer, more efficient mitochondrial base editors and real in vivo delivery at clinically relevant routes. The momentum echoes other recent inflection points in genetic medicine, including the PCSK9’s 2025 inflection.
The new editors matter because they finally explain and improve a trick many researchers suspected but could not fully control: using deaminase enzymes to rewrite single letters in mitochondrial DNA without cutting it. In March, researchers reported a refined way to install A to G changes by harnessing base excision repair inside mitochondria, and they built improved adenosine editors with fewer bystanders and lower off‑target activity. See the technical core in mitochondrial adenine base editing.
On the delivery front, January brought an equally important proof that injections can reach the organelle in the tissues that matter. A team packaged mitochondrial cytosine base editors in adeno‑associated virus 9 (AAV9), injected them systemically in mice, and corrected a disease‑relevant mutation in heart and skeletal muscle. The punchline was sobering and constructive. At high doses, the same constructs drove unwanted mitochondrial edits and severe adverse effects. The take‑home is not that the approach fails. It is that dosing and editor design are inseparable for safety. See the summary, AAV9 mitochondrial correction study.
Put those two threads together and you get a new playbook. Mitochondrial base editing is no longer a museum piece. It is an injectable candidate with a safety envelope that is becoming visible. That opens the door to the problem medicine most wants to solve: repairing the power systems of aging tissues.
Why aging care runs through mitochondria
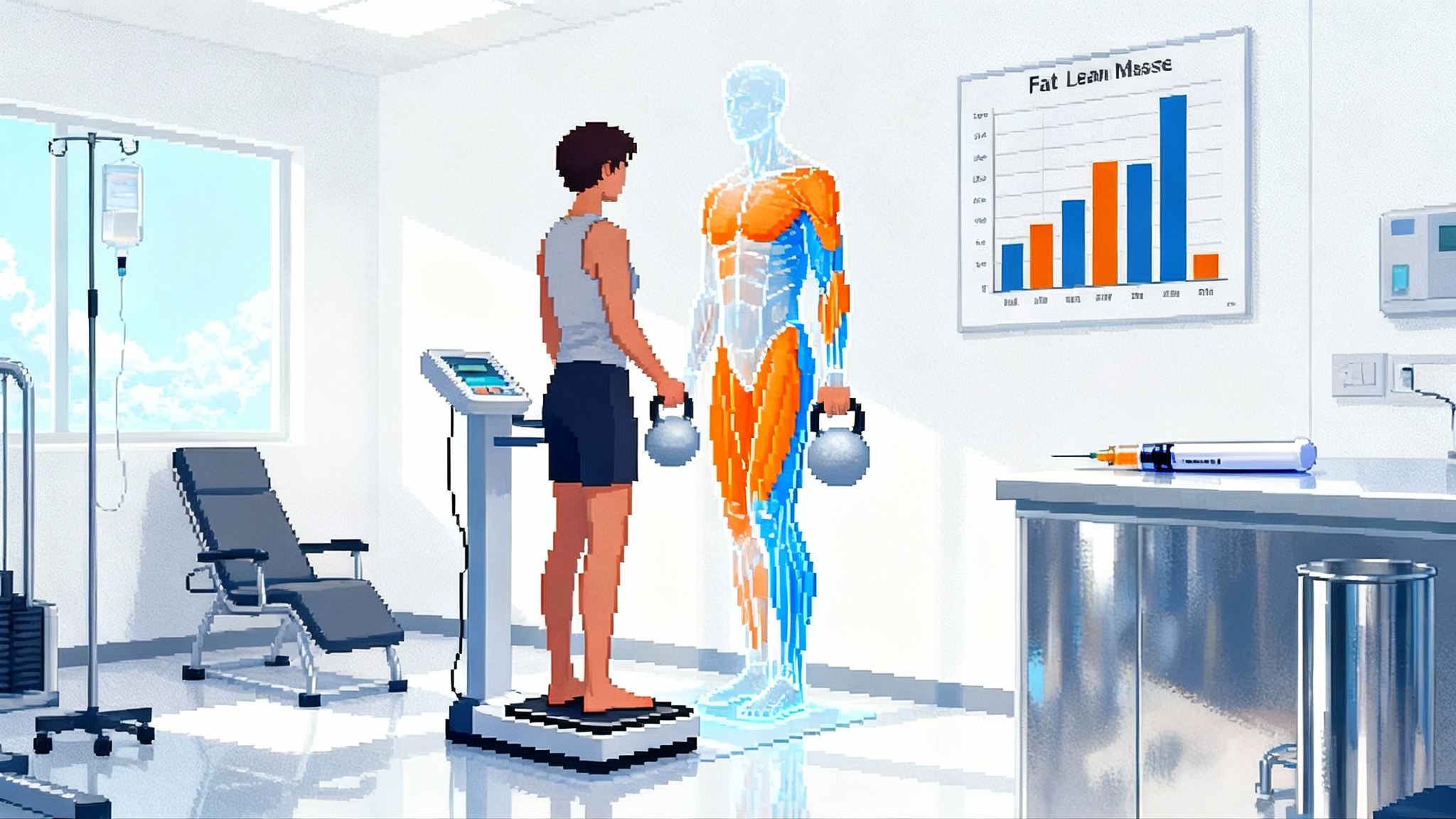
Sustained power output is what separates young heart, muscle, and brain from their older counterparts. Mitochondria generate the adenosine triphosphate that powers contraction, synaptic transmission, and endurance. Over decades, mitochondrial DNA accumulates point mutations and deletions, a process that drives heterogeneous populations of genomes inside the same cell. When the fraction of damaged genomes, known as heteroplasmy, crosses thresholds, the cell’s energy falls off a cliff. In cardiomyocytes the result is slower calcium handling and stiffening. In skeletal muscle the result is fatigue and loss of strength. In neurons it is reduced firing precision and vulnerability to stress.
In the hallmarks‑of‑aging framework, mitochondrial dysfunction is not a side character. It sits upstream of other hallmarks. Lower adenosine triphosphate worsens proteostasis by throttling chaperone and proteasome activity. It amplifies inflammatory signaling through mitochondrial damage‑associated molecular patterns. It fuels senescence by stressing the energy budget of repair pathways. If we correct mitochondrial function in old tissues, other hallmarks should soften. This is the same strategic logic that underpins targeted organ repair in areas like 2025 hearing gene therapy.
That is the strategic promise of mitochondrial base editing for longevity. It is not just a fix for a set of rare inherited disorders. It is a tool to push the power curve of aging tissues back toward youthful levels.
From untouchable DNA to editors that can move
Two molecular ideas unlocked this moment.
-
CRISPR‑free base editors for mitochondria. The organelle does not import guide RNAs efficiently, so classic CRISPR systems struggle there. Protein‑only editors solved the import problem by fusing DNA‑binding proteins called transcription activator‑like effectors to deaminase enzymes. For C to T changes, the DddA‑based editors established the first clear path. For A to G changes, the 2025 work showed that base excision repair can be coaxed to expose single‑stranded DNA inside mitochondria so an adenosine deaminase can act. The result is a complementary pair of editors that cover the two most common, therapeutically useful transitions.
-
Targeted protein traffic to mitochondria. Editors carry a short mitochondrial targeting sequence that acts like a street address on a package. Viral vectors or mRNA nanoparticles deliver the instructions to make the editor in the cell, the targeting sequence brings the protein to the organelle, and the transcription activator‑like effector arrays find the site in the small circular mitochondrial genome.
Technically, this is not simple. Editors are large, so most groups will use two vectors that reassemble the editor in the cell. But it is a solvable problem. Gene therapy has spent the last five years learning to move big cargos with split inteins and dual‑vector designs. That experience now transfers to mitochondria, just as new delivery tropisms spread across modalities during the xenotransplant pivot in 2025.
What changed in mid 2025
Three changes are particularly meaningful for a clinical path.
-
Higher efficiency with a mechanism. By showing that adenosine editing piggybacks on base excision repair, the March study gave teams a dial to turn. Engineer the repair context, and the edit rate goes up while bystanders go down. That is the difference between a stunt and a medicine, because clinical doses are shaped by how many cells you need to edit and how precisely.
-
In vivo editing at an injectable route, with honest safety signals. Systemic AAV9 delivery reached heart and muscle, corrected a defined defect, and revealed mitochondrial off‑target editing at high doses. That clarity is a gift. It tells developers to spend their time on editor specificity, vector tropism, and dose control rather than hoping problems will disappear in translation.
-
A delivery market that now includes mitochondria. Capsid engineering, muscle‑tropic serotypes, and targeted lipid nanoparticles were not built for mitochondria, but they are exactly what mitochondrial editing needs. Several companies specialize in these parts, from muscle‑specific capsids to protein‑delivery particles. The parts list exists.
The first in human path, next 12 to 24 months
The fastest and safest route is a focused early feasibility trial in a well‑characterized patient group where benefit can be measured quickly, and where tissues are reachable without heroic dosing.
-
Indication choice. Two rational entry points are adult patients with high‑burden mitochondrial myopathy driven by a dominant point mutation, or cardiomyopathy with a recurrent transfer RNA mutation that crosses heteroplasmy thresholds. Both groups have objective functional deficits, clear genetic targets, and accessible tissues for biopsy.
-
Product format and route. A dual AAV9 or muscle‑tropic variant encoding an optimized cytosine or adenosine editor is the leading option today for heart and skeletal muscle. A backup is lipid nanoparticles carrying mRNA for the split editors, paired with a peptide that promotes muscle uptake. Protein delivery via engineered virus‑like particles is emerging, but manufacturing scale and stability will trail mRNA and AAV in the near term.
-
Dosing. Start low on vector genomes per kilogram to stay under known mitochondrial off‑target thresholds, then escalate with adaptive rules tied to both safety labs and on‑target editing in sentinel muscle biopsies. Use a staggered single‑ascending dose design with at least four weeks between first and second participant at each level. Pre‑medicate to blunt innate responses, but avoid regimens that would mask early toxicity signals.
-
Manufacturing. Editors should include the latest specificity improvements and a mitochondrial targeting sequence that has been validated across species. Capsids must be screened for pre‑existing neutralizing antibodies during screening and enrollment. Impose strict release criteria on residual host cell proteins, empty capsids, and replication‑competent virus.
-
Off‑target safety. This is the hinge. It requires a layered plan:
- Mitochondrial genome. Use high‑depth, long‑read sequencing to detect rare edits and deletions across the full mitochondrial genome, not just around the on‑target site. Perform this in blood, in sentinel muscle, and in any available cardiac tissue if a device is implanted.
- Nuclear genome. Run exome plus a targeted panel for deaminase signatures. If mRNA delivery is used, perform whole transcriptome analysis to quantify RNA editing signatures in peripheral blood mononuclear cells.
- Dose response bounds. Predefine a ceiling for total off‑target burden per million mitochondrial genomes, above which no further dose escalation occurs. Tie that ceiling to animal data and a mechanistic rationale instead of a round number.
- Functional toxicology. Monitor cardiac troponin, brain imaging if indicated, and fasting plus post‑exercise lactate. Add electrophysiology monitoring for arrhythmia risk in the first month after dosing.
-
Biomarkers of benefit. Pick readouts that change within weeks, not years.
- Heteroplasmy shift at the target locus in muscle biopsy by droplet digital polymerase chain reaction, expressed as percentage‑point change from baseline.
- Phosphocreatine recovery time constant in calf muscle by phosphorus‑31 magnetic resonance spectroscopy after standardized exercise, a sensitive measure of mitochondrial oxidative capacity.
- Six‑minute walk test distance, hand grip strength, and a patient‑reported fatigue scale with daily smartphone prompts to reduce recall bias.
- For cardiomyopathy, left ventricular strain by speckle‑tracking echocardiography and natriuretic peptide levels.
-
Trial design. A single‑center, open‑label Phase 1 with three dose levels and three to four participants per level, followed by an expansion cohort at the best‑tolerated dose. Primary endpoints are safety and tolerability. Key secondary endpoints are heteroplasmy shift and the spectroscopy measure. Plan for interim analysis after the second dose level to decide whether to proceed to the heart‑enriched cohort or remain in skeletal muscle only.
-
Follow up. A two‑year follow up with predefined windows at day 7, day 28, month 3, month 6, year 1, and year 2. Bank blood and optional tissue for future off‑target methods that may become available. Include vector shedding assays for semen and saliva in the first month.
-
Patient safeguards. Independent data monitoring, clear stopping rules for any rise in off‑target burden above the ceiling, and real‑time disclosure of safety summaries to participants.
This plan is deliberately conservative on dose and aggressive on measurement. It leans into the 2025 lesson that the editors work in vivo and that dose drives risk.
How this fits the hallmarks of aging
If the trial shows safety and even a modest heteroplasmy shift with a concurrent gain in the spectroscopy readout, it would be the first direct demonstration that editing mitochondrial DNA in adult tissue can restore energy metabolism. That would strengthen the idea that mitochondrial dysfunction is not just correlated with aging, it is causally adjustable.
Downstream hallmarks should also move. Improved adenosine triphosphate production can lower reactive oxygen species burden and reduce stress signaling that feeds senescence and chronic inflammation. Better energy status can support protein quality control and autophagy, which are impaired in aged cells. Those shifts do not require a wholesale reprogramming event. They are the result of tipping the intracellular power budget back in the cell’s favor.
The clinical implications are not limited to rare disease. Sarcopenia, heart failure with preserved ejection fraction, and neurodegenerative conditions share a common constraint: reduced energy throughput in the most demanding cells. If a mitochondrial editor can safely lift that ceiling, even by a narrow margin, the effect on function could be meaningful because these systems operate near thresholds where small gains matter.
What industry should do now
-
Build editors that are boringly precise. Adopt the 2025 adenosine editor improvements and keep iterating on deaminase variants with lower RNA activity. Publish complete off‑target maps for the exact sequences you intend to put in people.
-
Match editor to tissue with intention. For skeletal muscle and heart, favor muscle‑tropic capsids or targeted lipid nanoparticles with validated detargeting of the liver. For brain, you will need intrathecal or intracisternal routes and a different risk framework, so start there later.
-
Use dose as a design variable. Set dose ceilings from animal mitochondrial off‑target data, not from nuclear gene therapy precedents. Include an adaptive protocol that can downshift capsid dose and upshift editor potency mid program.
-
Invest in measurements. If your spectroscopy and heteroplasmy assays are not sensitive and repeatable, you will miss the signal or mistake noise for risk. Build those capabilities in house or with partners early.
-
Share negative data. The field will move faster, and regulators will trust you more, if high‑dose or off‑target findings are shared promptly and in detail.
What regulators can do to speed the safe path
-
Define a mitochondrial off‑target rubric. Require full mitochondrial genome sequencing across compartments and set expectations for reporting low‑frequency edits. Encourage sponsors to prospectively define acceptable off‑target burden tied to animal function.
-
Encourage sentinel tissue sampling. A muscle biopsy for on‑target and off‑target analysis is defensible if it prevents broad exposure to unsafe doses. Make this clear in early meetings.
-
Create a redosing pathway. Immunity to capsids or editor proteins will matter. Provide guidance on plasmapheresis, immune modulation, and eligibility for redosing in the presence of neutralizing antibodies.
-
Support adaptive early trials. Allow dose and route adjustments based on real‑time biomarkers so that teams can learn without restarting studies.
Why this could be the next CRISPR‑scale inflection for longevity
Gene editing transformed rare disease and hematology because it gave developers a lever to move disease mechanisms with precision. Mitochondrial base editing points that lever at the energy core of aging tissues. The technical parts exist. The clinical measurement tools exist. The safety signals are visible early enough to engineer around. That combination is rare.
The scale comes from common diseases. If you can safely raise mitochondrial function in even a subset of skeletal muscle fibers and cardiomyocytes, you can alter trajectories of mobility, independence, and cardiac resilience in aging populations. If you can do the same for vulnerable neuronal populations, you can shift the balance between decline and stability in neurodegeneration. The path will be incremental, but the step function in capability has already occurred.
A pragmatic, slightly accelerationist closing argument
Move now, but move with discipline. The field finally has editors that make biological sense in mitochondria and delivery systems that can reach heart and muscle with an intravenous injection. Use them. Keep doses below the off‑target cliff. Measure everything that matters, from heteroplasmy to energy flux to function. Put the first needles into well‑chosen patient groups where a few percentage points of editing can change daily life.
If developers and regulators follow that script, mitochondrial editing will not replace other longevity strategies, it will power them. Improve cellular energy, and nutrition, exercise, and cardiometabolic therapies all work better. In a decade we may look back at 2025 as the year the energy problem moved from the margins to the center of medicine, and the year we found out that some of the decline we called aging was just a fixable shortage of power.