Moderna's CMV Failure Sparks A Geroscience Pivot
On October 22, 2025, Moderna ended its congenital CMV vaccine program after a failed primary endpoint. The loss points to a bigger win: treating CMV as a modifiable driver of immunosenescence with vaccines, T cells, and antivirals built for older adults.
Breaking: a vaccine setback becomes a systems-level opportunity
On October 22, 2025, Moderna disclosed that its cytomegalovirus vaccine failed its primary endpoint and that it would discontinue its congenital CMV program. The company said the shot’s efficacy in preventing primary CMV infection in seronegative women was far below target, and it will shift remaining CMV work to narrower settings. The news was disappointing. It also clarified the path forward. Rather than chasing primary prevention in pregnancy, the field can pivot to a wider geroscience question: can we control lifelong CMV to slow immune aging and extend healthy years? Moderna’s phase 3 readout sets the stage for that pivot.
Reframing CMV as a modifiable driver of immunosenescence
CMV is a herpesvirus that most people acquire early in life. It does not leave. Instead, it establishes latency and reactivates periodically. The immune system keeps it in check, but this long cold war has a cost. CMV does not just hide in our tissues. It quietly pulls T cells into a lifelong tug of war.
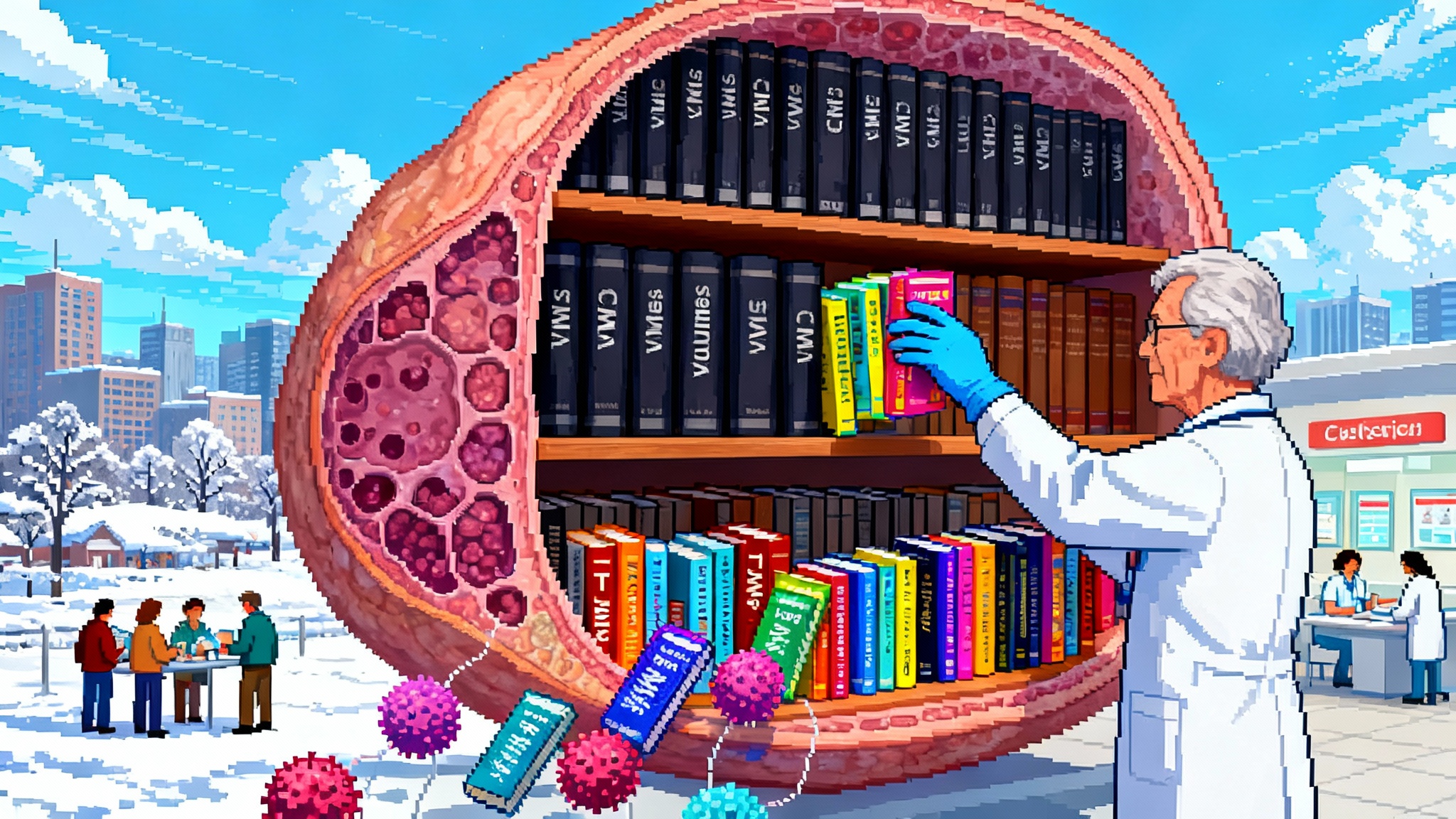
A simple metaphor helps. Picture your adaptive immune system as a library with finite shelf space. Each new pathogen adds books. CMV adds a whole series that never goes out of print and demands prominent display. Over decades, that shelf space is dominated by CMV titles. Immunologists call this memory inflation. The result is a T cell repertoire skewed toward CMV, with large expansions of late-differentiated effector cells and a shrinking pool of naive T cells available for new threats. A comprehensive review of CMV’s imprint on T cells details these dynamics and their spillover effects on immune function, especially in older adults. See the CMV memory inflation review.
The repertoire shift is not merely academic. When a large fraction of circulating T cells are preoccupied with CMV, the immune system can become less flexible. That shows up in several ways that matter for everyday health as people age:
- Reduced diversity in T cell receptors and fewer truly naive cells ready to learn new antigens.
- Expansion of CD57-positive, CD28-negative T cells that behave like well-worn soldiers. They are experienced, but less proliferative, and secrete more inflammatory cytokines.
- Elevated background inflammation, often called inflammaging, which correlates with frailty, cardiovascular risk, and slower recovery from stressors like surgery or infection. Related discussions of frailty appear in the St. Jude’s frailty trial.
Evidence linking CMV to weaker vaccine responses in older adults is mixed by platform and context. Some studies show little difference in antibody titers, others show diminished responses to certain vaccines. That inconsistency is a feature, not a bug. It points to a mechanism that is plastic and therefore targetable. If CMV is one of the forces that tilts the immune system toward rigidity and low-grade inflammation, reducing CMV’s load or rebalancing immunity against it could restore flexibility. The correct goal is not to eradicate CMV. The goal is to recalibrate the relationship.
The forward path: three levers to test in older adults
A practical geroscience program for CMV should combine three complementary approaches, each optimized for people over 60 and for those with multimorbidity.
1) Therapeutic CMV vaccines for older adults
Design intent shifts from preventing primary CMV infection to boosting control of latent virus and blunting reactivation. The product profile looks different from congenital prevention:
- Antigen selection: gB for neutralizing antibodies plus pp65 and immediate early proteins IE1 and IE2 to expand functional T cells that recognize diverse CMV life-cycle stages.
- Formulation and adjuvant: platforms that emphasize strong cellular immunity and durability. Vector or mRNA approaches can be tailored to maximize polyfunctional CD8 and Th1 CD4 responses, with safety margins acceptable for older adults.
- Dosing: a prime followed by periodic boosters every one to three years based on biomarker readouts of CMV-specific T cell breadth and function.
This is not theoretical. Transplant settings already show that vaccines designed to broaden CMV-specific T cells can reduce viremia and antiviral use. The transplant data are not a direct read-through to community-dwelling older adults, but they prove the immunology can be engineered.
How to trial it: enroll adults 65 to 85 who are CMV seropositive, stratify by baseline CMV viral load in saliva and plasma and by CMV-specific T cell breadth, and randomize to vaccine versus control on top of standard care. Power the study for changes in immune function and infection burden, not hard mortality endpoints. See pragmatic endpoints below.
2) Adoptive CMV-specific T cells for frail or repeatedly infected adults
Virus-specific T cell therapy is now routine in academic transplant centers. Manufacturing simplified, banks of partially matched T cells exist, and safety is favorable. The question is whether a lighter, outpatient version can help older adults who are frail, frequently hospitalized for respiratory infections, or repeatedly exhibit CMV reactivation along with functional decline. The transplant field is evolving alongside innovations like the 2025 pig kidney trials.
Practical contours of a first-in-population program:
- Indication: older adults with recurrent CMV reactivation or persistent high CMV DNAemia despite oral antivirals, compounded by poor vaccine responses and high hospitalization risk.
- Product: allogeneic CMV-specific T cells selected for breadth of epitope recognition and lower alloreactivity, at doses engineered for transient persistence.
- Setting: single infusion in day hospital with 90-day follow-up, on top of standard antivirals as needed.
- Readouts: CMV DNA area under the curve, hospital days, and improvement in CMV-specific T cell breadth without cytopenias or graft-versus-host phenomena.
Some companies’ multi-virus T cell programs have recently stumbled in late-stage trials in transplant populations. That cautionary signal should shape study design, not end it. Focus on narrower CMV biology, minimize heterogeneity, and use adaptive designs to find the dose and patient subgroup where benefit is largest.
3) Long-acting antiviral control for seasonal and situational risk
We already have effective CMV antivirals. Letermovir prevents replication by targeting the viral terminase complex and is widely used for prophylaxis in transplant patients. Valganciclovir and ganciclovir work but are limited by bone marrow toxicity. Maribavir targets UL97 and is approved for resistant disease. The geroscience question is whether we can control CMV reactivation in older adults during windows of vulnerability without adding new harms.
A near-term path is seasonal or event-triggered prophylaxis in high-risk settings. Think of winter respiratory season, rehabilitation stays, or the month after a major surgery. Two feasible designs:
- Letermovir pulses: six to twelve weeks of oral prophylaxis in seropositive adults with a history of winter hospitalizations for infections. Monitor CMV DNA in saliva and blood, antibiotic-days, and all-cause respiratory infection days.
- Maribavir rescue bundles: add maribavir for short courses in older adults with recurrent CMV DNAemia and fatigue or cytopenias that limit ganciclovir use. Track symptom recovery, hematologic safety, and virologic response.
Before long, longer-acting formulations are plausible. We have precedents in other viruses, and ophthalmology once used ganciclovir implants to suppress CMV retinitis for months. A quarterly injectable depot or implant is not ready for primary-time use in geriatrics, but it is a clear direction for medicinal chemistry and drug delivery groups.
Pragmatic endpoints that prove geroscience value
Regulators and payers will not accept “slows aging” as an indication. They will accept well-chosen surrogates and hard outcomes that matter to patients and systems. A strong CMV geroscience program should pre-specify three layers of endpoints and use them consistently across vaccine, cell, and antiviral trials.
- Immune age and CMV biology
- CMV-specific T cell breadth and polyfunction by standardized assays. Summarize as a composite score that captures epitope coverage and cytokine quality.
- T cell repertoire flexibility: proportion of naive CD4 and CD8 cells and reduction in terminally differentiated CD57-positive CD28-negative cells.
- Inflammatory age: a validated protein-based immune age clock such as iAge that integrates chemokines like CXCL9 into a continuous score of immune aging. Related biomarker approaches appeared in the 2025 plasma exchange trial.
- CMV DNA and shedding: copy number area under the curve in blood and saliva, frequency of reactivation episodes, and time to undetectable after trigger events.
- Vaccine responsiveness and immune function
- Serologic and cellular responses to routine vaccines given during the trial window, such as influenza, respiratory syncytial virus, and Covid boosters. Focus on neutralization titers, T cell cytokine profiles, and memory durability at 6 and 12 months.
- Delayed-type hypersensitivity or in vitro recall responses to neoantigens where appropriate and ethical.
- Infection burden and clinical utilization
- Days with symptomatic respiratory infection validated by multiplex polymerase chain reaction.
- Antibiotic-days and antiviral-days captured from pharmacy data.
- All-cause infection hospitalizations, emergency department visits for infection, and total hospital days in winter.
- Functional and quality-of-life measures sensitive to infection-driven setbacks, such as gait speed and activities of daily living recovery after a hospitalization.
These endpoints give a full stack view. They show whether the CMV relationship is calmer, whether the immune system learned better from vaccines, and whether that translated into fewer bad days and less costly care.
Milestones for 2026 to 2028
A realistic three-year arc can turn this pivot into practice.
-
2026
- Launch two Phase 2a therapeutic vaccine trials in community-dwelling seropositive adults 65 to 85. Primary endpoints: CMV DNA burden and immune age improvement at 6 months. Key secondary endpoints: responses to seasonal vaccines and winter infection days.
- Begin two pragmatic studies of seasonal letermovir prophylaxis in skilled nursing facilities and post-acute rehabilitation centers. Use cluster randomization and embed within electronic health record workflows for enrollment and outcome capture.
- Start a pilot of allogeneic CMV-specific T cells for older adults with recurrent CMV DNAemia and high utilization, using adaptive dosing and rigorous safety monitoring.
-
2027
- Read out vaccine trials with immune and infection outcomes through two winter seasons. If immune age improvements and infection reductions align, request Breakthrough Therapy or Fast Track designation for the most promising vaccine candidate.
- Expand antiviral prophylaxis pilots to regional health systems. Power for reductions in hospital days and antibiotic-days during winter.
- Generate the first prospective data linking changes in immune age scores to concrete clinical outcomes after CMV control. Use these data to refine surrogate endpoints with regulators.
-
2028
- Launch pivotal vaccine and antiviral trials with co-primary endpoints that blend immune function and real-world healthcare utilization. Consider accelerated approval for vaccines based on immune-age and CMV biology surrogates with commitments for post-market clinical outcomes.
- File for label expansions where justified, such as seasonal antiviral prophylaxis for defined high-risk older adult populations, supported by reductions in hospitalizations.
- Publish payer-facing economic models that translate trial outcomes into avoided costs, with sensitivity analyses for different winter severity scenarios.
Regulatory levers to speed evidence into access
- Surrogate endpoints with clinical grounding: regulators have accepted immunobridging for respiratory vaccines and virologic surrogates for antivirals. For CMV geroscience, pair virologic control and CMV-specific T cell breadth with validated immune-age measures that correlate with morbidity in longitudinal cohorts.
- Platform thinking: allow updating of vaccine constructs as new CMV antigens or delivery systems improve T cell quality, similar to strain updates in other vaccine categories.
- Enrichment and adaptive designs: enroll seropositive older adults with low CMV-specific T cell breadth or repeated reactivation to increase event rates and signal clarity. Use group-sequential monitoring and seamless Phase 2 to Phase 3 transitions for the most promising arms.
Payer levers to make it real in the places that need it most
- Coverage with evidence development for seasonal antiviral prophylaxis and the first therapeutic vaccines in older adults. Tie reimbursement to participation in registries that capture standardized immune and clinical endpoints.
- Medicare Advantage pilots: offer a winter CMV-control bundle that combines a vaccine booster window, antiviral availability, and home-based testing for CMV shedding and respiratory pathogens. Reward plans for reductions in infection hospitalizations and antibiotic-days.
- Pharmacy-first delivery: authorize community pharmacies to administer therapeutic CMV vaccines and dispense short antiviral courses aligned to personalized CMV and immune-age profiles. This is how to reach millions of older adults quickly.
What success looks like in plain numbers
By the end of 2028, a successful CMV geroscience program would target the following effect sizes, all prospectively defined and validated across independent datasets:
- 30 percent reduction in CMV DNA area under the curve over 12 months in vaccinated or prophylaxed older adults compared with controls.
- 20 percent relative increase in naive T cell proportions and a measurable expansion in CMV-specific T cell breadth without excess inflammation.
- 25 percent reduction in antibiotic-days and 15 percent reduction in winter infection hospitalizations among high-risk enrollees.
- A clinically meaningful improvement in immune-age scores that correlates with fewer hospital days and faster functional recovery after common stressors.
These are not moonshots. They are conservative targets chosen to matter for people and payers while being attainable with current tools.
Why de-risking CMV control could unlock healthspan gains
Healthspan is not an abstract concept. For older adults, it often means fewer infections, better recovery after them, and more resilient responses to vaccines. CMV management sits at the intersection of those goals. If we can reduce CMV’s constant pull on the T cell repertoire and dial down inflammatory tone, we give the immune system back some of its flexibility. That flexibility is what helps a flu shot work better, turns a winter cold into a nuisance rather than a hospitalization, and shortens the slow slide after a surgery or a fall.
The Moderna news changed the question, not the stakes. Congenital prevention remains a worthy aim, but the biggest near-term opportunity lies in older adults. The tools exist. The endpoints are measurable. The trial settings are ready. What is needed now is coordination across vaccinology, cell therapy, and antiviral pharmacology, aligned to practical readouts that matter to regulators and payers.
The bet is straightforward. Tame a lifelong viral tenant that monopolizes immune attention, and you make room for healthier aging. That is a geroscience pivot worth making.