CHIP Goes Therapeutic: 2025’s Shift From Marker to Target
ESC 2025 data show low-dose colchicine can slow TET2-driven clonal growth, while new mega-cohort analyses pinpoint who is at risk. Here is why routine CHIP screening is near and how a 12–24 month rollout could work.
The moment CHIP became actionable
In cardiology, some pivots arrive quietly. This one did not. At the European Society of Cardiology Congress 2025, investigators reported that daily low-dose colchicine slowed the growth of blood-cell clones driven by TET2 mutations, the very clones long linked to higher rates of heart attack, stroke, and heart failure. The effect was most pronounced where biology said it should be, in TET2-driven clonal hematopoiesis of indeterminate potential, often shortened to CHIP. For years clinicians treated CHIP as a red flag. In 2025 it started to look like a handle.
For context, the colchicine signal came from a prespecified genetic subanalysis nested in a large randomized trial. It tracked clonal growth over time and showed that people on colchicine had smaller increases in the size of TET2-mutant clones than those on placebo. The headline finding is detailed in an American College of Cardiology summary and simultaneous journal publication, which reported a marked attenuation of TET2 clonal growth with 0.5 milligrams daily of colchicine colchicine subanalysis in LoDoCo2.
A second thread of news at ESC 2025 was about risk calibration. Fresh analyses from large, long-running cohorts and trials refined how CHIP translates to cardiovascular risk at older ages. In the Women’s Health Initiative Long Life Study, which enrolled women with a median age of 80 years, specific CHIP subtypes still tracked with incident cardiovascular events. In particular, TET2, ASXL1, and JAK2 mutations were associated with outcomes including coronary disease, heart failure, ischemic stroke, venous thromboembolism, and cardiovascular death CHIP and cardiovascular outcomes in older women.
Taken together, these two pieces of evidence change the posture of the field. We now have a plausible way to slow the growth of a high-risk clone and a clearer map of who carries the risk into late life. That is enough to plan for clinical adoption.
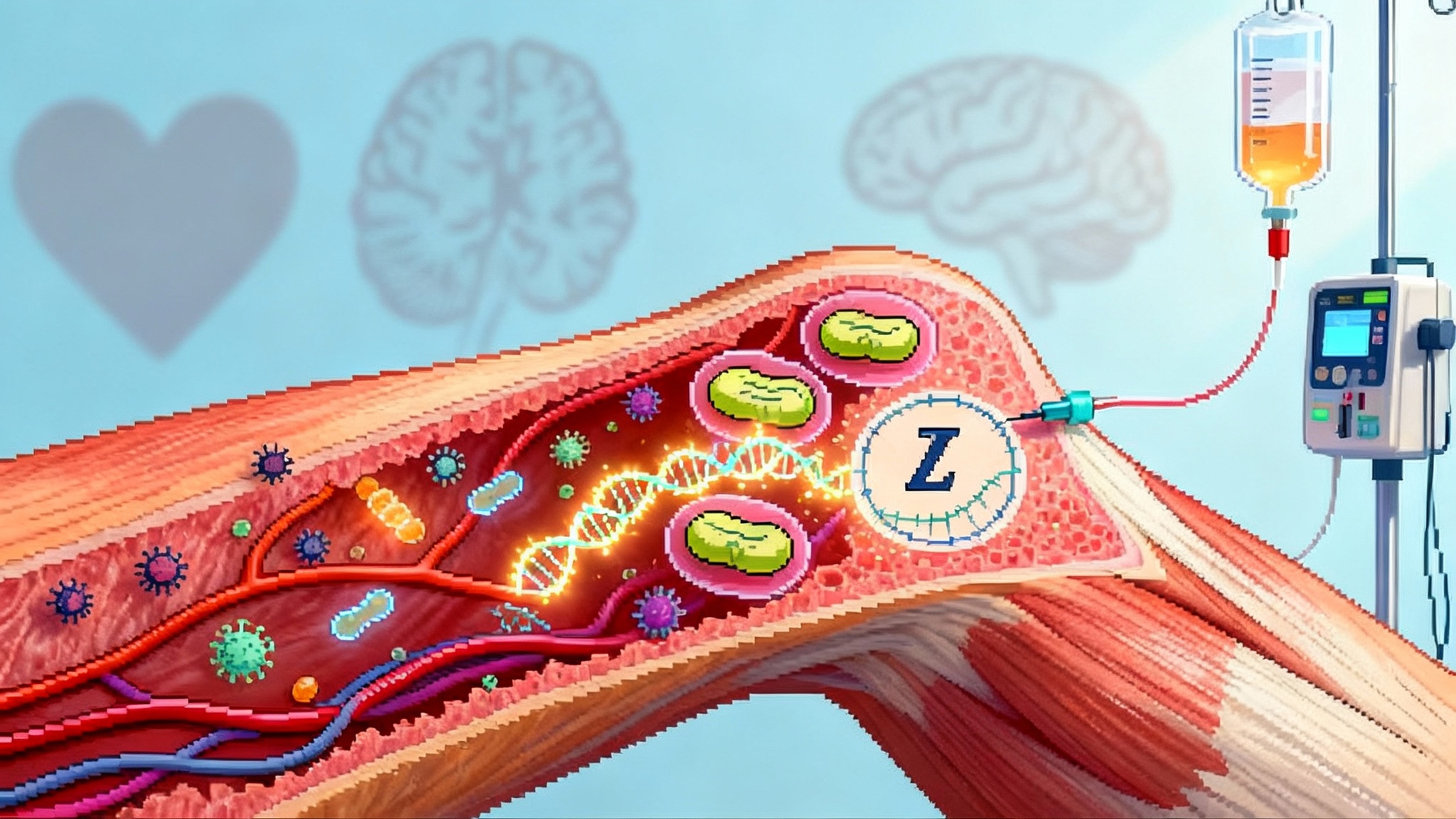
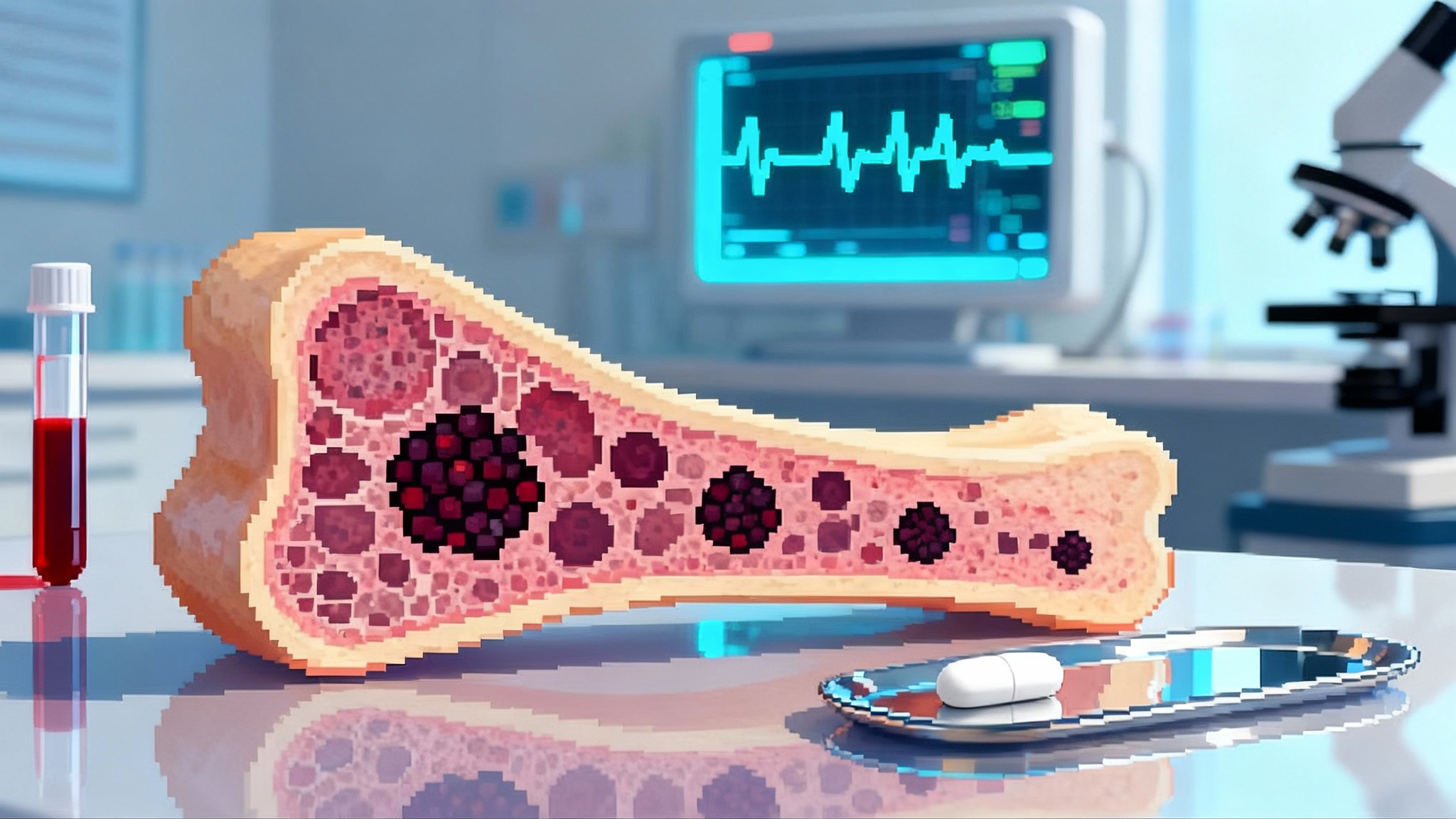
What CHIP actually is, in plain terms
Every so often, a single stem cell in the bone marrow picks up a mutation that lets it outcompete its neighbors. Its descendants spread slowly through the blood system. Imagine a small branch grafted onto a tree that grows faster than surrounding branches. That branch is the clone. When the branch carries a mutation in a gene like TET2, DNMT3A, ASXL1, or JAK2, the clone can skew the immune system toward a more inflammatory state. Over years, that bias can push atherosclerotic plaques and thrombosis in the wrong direction.
Clinically, we define CHIP by finding one or more leukemia-associated mutations in blood with a variant allele fraction of about 2 percent or higher, in people without evidence of a blood cancer. The number and size of clones matter. Larger clones, or multiple clones, generally carry higher risk. The gene matters too. TET2 and JAK2 tend to be more dangerous for the heart and brain than DNMT3A in many analyses.
Why ESC 2025 was different
There have been hints for years that tamping down inflammation could reduce cardiovascular events in people with CHIP. What changed at ESC 2025 was a direct look at the growth of the clone itself. In the colchicine analysis, serial blood sequencing showed that TET2-mutated clones expanded more slowly on low-dose colchicine than on placebo. It is as if the fast-growing branch on the tree met pruning shears that favored restraining that specific branch. That does not mean colchicine eliminates the clone, but it suggests we can slow its spread, and the biggest effect appears where the cardiovascular risk is highest.
The mechanistic logic fits what basic science has been saying. Loss of TET2 in blood cells pushes inflammatory pathways, including interleukin-1 beta and interleukin-6. Colchicine is a microtubule poison at low dose, but functionally it dampens inflammasome activation and neutrophil trafficking. The match between mechanism and clinical observation is tight enough to move from theory to practice. Work on reversing immune aging adds useful context for tailoring interventions by biology, not just by risk scores.
The case for routine screening
Screening only makes sense if three conditions hold. The condition must be common, testable, and actionable. CHIP is common. About one in ten people in their seventies has it, and prevalence climbs with age. CHIP is testable with a simple blood draw and targeted sequencing. And after ESC 2025, CHIP is actionable, at least for the highest risk subtypes. If a low-cost, once-daily drug can slow clonal growth in TET2 CHIP and potentially reduce events, then finding those carriers is no longer academic.
This approach should complement, not replace, lipid-lowering and risk-factor control. It pairs naturally with breakthroughs such as PCSK9 base editing in prevention and broader metabolic strategies like anti-glycation therapy trials.
Who should be tested first
Start where the signal is strongest and the clinical payoff is largest. A prioritized list for the first two years could look like this:
- Adults 65 and older with chronic coronary disease, especially if they have recurrent events or persistent high-sensitivity C-reactive protein above 2 milligrams per liter despite good control of blood pressure, glucose, and lifestyle.
- Adults of any age with premature or unexplained atherosclerotic events in the absence of conventional risk factor explanations.
- Patients with ischemic stroke or transient ischemic attack without a clear proximal cause, particularly if there is elevated inflammation.
- Patients with heart failure with preserved ejection fraction where systemic inflammation is suspected to contribute to symptoms or exacerbations.
- Patients with chronic kidney disease stages 3 to 4, who are at high vascular risk and, in recent analyses, appear to carry excess cerebrovascular risk when non-DNMT3A CHIP is present.
- Those being evaluated for early aortic valve stenosis progression, where growth in clone size and higher variant allele fraction seem to track with faster disease.
- Adults with persistent venous thromboembolism risk or a history of unprovoked clots, especially if JAK2 mutations are present, given their strong association with thrombosis and cardiovascular death in older cohorts.
A practical principle underlies this list. Test first in settings where a positive result would change therapy now, not in some theoretical future.
How the test works in practice
- Specimen and platform: Peripheral blood, standard venipuncture, sent for targeted next-generation sequencing of canonical CHIP genes. A focused panel that covers DNMT3A, TET2, ASXL1, JAK2, and a small set of additional myeloid drivers is sufficient for cardiovascular use.
- Thresholds: Report any pathogenic or likely pathogenic variant at a variant allele fraction of at least 2 percent. Laboratories can detect lower, but 2 percent is a practical floor that balances sensitivity and noise for clinical decisions. Report maximum variant allele fraction and the sum of clone fractions when multiple clones are present.
- Frequency: Baseline testing for eligible patients, then repeat in 12 months if positive to gauge growth. If variant allele fraction is above 10 percent or there are multiple high-risk clones, consider six-month rechecks for the first year to establish a slope of growth.
- Interpretation: TET2, ASXL1, and JAK2 carry the clearest cardiovascular signal. DNMT3A is common and may be lower risk. Larger clones matter more than tiny ones. Growth rate adds information beyond the baseline number.
- Counseling: Explain that CHIP is not cancer today, but it raises cardiovascular risk and small risks of blood cancers over many years. Emphasize the opportunity to act on the cardiovascular part now.
What to do when CHIP is positive
- TET2 or ASXL1 with variant allele fraction 2 to 10 percent: Discuss starting low-dose colchicine 0.5 milligrams daily, barring contraindications. Review possible gastrointestinal upset, drug interactions with strong cytochrome P450 3A4 inhibitors or P-glycoprotein inhibitors, and caution with significant renal or hepatic impairment. Check a baseline complete blood count and creatinine, then repeat after four to eight weeks.
- TET2 or ASXL1 with variant allele fraction above 10 percent or clear growth on serial testing: Strengthen the case for colchicine. Consider referral to a cardio-hematology or CHIP clinic if available. Establish a monitoring plan with blood counts and clone size at set intervals.
- JAK2 mutation: Evaluate for myeloproliferative features with a hematologist. From a cardiovascular standpoint, be proactive about antithrombotic strategy tailored to the full clinical picture. Colchicine may not address the thrombosis biology of JAK2 directly, so this group needs individualized plans.
- Multiple clones or very high clone fraction: Treat like a risk equivalent for recurrent atherosclerotic events. Intensify cardiovascular prevention suited to the patient’s profile. Use colchicine where TET2 or ASXL1 are present and tolerated.
Across these categories, do not chase inflammation with broad immunosuppression. Choose targeted agents with the best balance of evidence and safety for long-term use in older adults. Colchicine fits that bill now for selected subtypes. Agents that block interleukin-1 or interleukin-6 signaling may follow as the evidence matures, especially if future studies show an effect on clone dynamics, not just on events.
The 12 to 24 month roadmap to adoption
Here is a concrete timeline that health systems can execute without waiting for new laws or exotic technologies.
- Months 0 to 3: Form a small CHIP task force in cardiology with a hematology partner. Choose a sequencing lab and lock an order set in the electronic record that includes CHIP panel, high-sensitivity C-reactive protein, and baseline complete blood count with creatinine. Draft a one-page consent and counseling script.
- Months 3 to 6: Launch a pilot in one or two clinics that see many older adults with chronic coronary disease or recurrent events. Start screening per the criteria above. Track test yield, time to result, and prespecified therapy decisions. Begin prescribing colchicine for eligible TET2 or ASXL1 carriers. Create a pharmacist-led interaction check for colchicine initiations.
- Months 6 to 12: Expand to stroke and heart failure clinics. Add reflex re-testing at 12 months for positives. Build a simple registry that captures variant allele fraction, growth rates, adverse effects, adherence, and cardiovascular events. Negotiate coverage with payers using evidence packets that include the ESC 2025 data and large cohort risk analyses. Use existing next-generation sequencing billing codes where applicable, with clear documentation that testing informs cardiovascular therapy.
- Months 12 to 18: Publish or present pilot outcomes internally and to local quality committees. Update institutional prevention guidelines to recommend CHIP testing in the defined high-yield groups. Roll out automated electronic record prompts that suggest ordering CHIP testing when a high-sensitivity C-reactive protein result is persistently elevated or when a patient meets stroke or coronary disease criteria without recent events explained by conventional risk factors.
- Months 18 to 24: Integrate CHIP status into discharge checklists for myocardial infarction, stroke, and heart failure. Add variant allele fraction and clone subtype to risk dashboards that clinicians already use. Submit data and experience to national guideline committees. Prepare for payer coverage policy updates by standardizing documentation templates and patient education materials.
What makes this roadmap realistic is that every step uses existing infrastructure. Blood draw, targeted sequencing, a generic drug, and structured follow-up are standard tools. The novelty is the patient selection and the decision to treat a clone, not just a lab value.
How this could compress late-life cardiovascular mortality
Clonal hematopoiesis does not kill directly. It stacks the deck by making immune responses more inflammatory and blood more thrombosis-prone over time. That gradually increases the rate of events after age 65. The late-life mortality curve is driven by repeat events in people with damaged vascular beds, simmering inflammation, and reduced physiologic reserve. If you can cool the immune bias and slow the growth of the highest-risk clones, you reduce recurrent events and postpone first events that would otherwise occur in the eighth or ninth decade. The result is a lower tail of mortality from cardiovascular disease after age 75 and more people reaching very old age with less progressive vascular disability.
Importantly, this is not an argument against conventional prevention. It is a complement that addresses a different kind of residual risk. Two patients can have similar cholesterol, blood pressure, and glucose, yet very different inflammatory tone because one carries a TET2-mutated clone that keeps stoking vascular fire. Treating that specific driver may yield benefits that general risk control cannot fully capture on its own.
What clinicians can do next, starting Monday
- Pick your pilot population. Chronic coronary disease clinics with older adults are the most straightforward start.
- Choose a lab and a five-gene panel. Insist that reports include gene, variant, and variant allele fraction with detection thresholds and a recommended re-test interval.
- Build a short counseling script. Explain what CHIP is, why you are testing, and what you will do with the result.
- Create a standard colchicine order with a drug interaction checklist and a monitoring plan. Include a templated note that documents the rationale tied to clone subtype and variant allele fraction.
- Track outcomes in a small registry that records clone dynamics and cardiovascular events. That registry will be your lever for internal scale-up and external coverage discussions.
The open science questions worth watching
- Does colchicine reduce hard cardiovascular events more in TET2 or ASXL1 carriers than in noncarriers when used as background prevention in real-world practice?
- Will interleukin-1 beta or interleukin-6 directed therapies alter clone dynamics, not only inflammation, in specific CHIP subtypes?
- What is the minimal variant allele fraction and growth rate that justifies therapy in primary prevention, and how should that threshold vary by age and comorbidity?
- Can we build simple, validated clinical scores that combine age, high-sensitivity C-reactive protein, clone subtype, and growth rate to guide therapy initiation and intensity?
Bottom line
In 2025, clonal hematopoiesis crossed an invisible line. The field went from observing a risk signal to acting on a modifiable target. Slowing the growth of TET2-driven clones with a safe, inexpensive drug is not a silver bullet, but it is a practical handle that clinicians can use today in the right patients. With a focused testing strategy and a disciplined rollout, health systems can start compressing late-life cardiovascular mortality by treating a root cause that hides in plain sight: a small, pushy branch on the blood-cell family tree that responds when you finally give it a reason to slow down.